Introduction
The presence and diagnosis of antemortem pathology on human skeletal remains can sometimes assist in the personal identification of unknown human remains. The disease should have been of such nature and severity that the individual and his close contacts would have known about it. If records of the medical condition, and in particular radiographs are available, a positive identification, provable in court, can be made. This may be of particular use in cases where no other means of individual identification exist, e.g. no dental records.
Not all diseases affect bones. Arthritis, for example, is mainly a disease of the musculoskeletal system, but very few of the 200 known varieties leave traces on bone. For any disease to alter bone takes a long time, and therefore usually only diseases of chronic nature are observable. These markers of disease are also often nonspecific in nature, which precludes a positive diagnosis. One of the problems with proper recording of skeletal disease is the lack of consistent, standardized terminology. Another problem that may arise in diagnosis is the incompleteness of the remains. Often only parts of the skeleton are present, whereas the diagnosis of some diseases may require the presence of smaller bones such as those of the hand or foot. Police and other people involved in this type of work should, therefore, be trained to make a special effort to retrieve all fragments.
Despite these problems, many advances in the study of bone pathology have been made over the last few years. Several topics on the subject have been published. Although the main theme of their study was disease in history, the descriptions of osseous changes are also applicable to bones of forensic origin. Traditional pathologists are seldom confronted with dry bones, and therefore much of the groundwork has been done by paleopathologists. This field of study has also gained impetus with the formation of the North American and European Associations of Paleopathology.
When examining lesions on bone, care should be taken to determine whether the observed feature is, in fact, pathological and not part of the normal variation seen in all human populations. Detailed knowledge of the morphology of normal bone is therefore essential. This is often true in younger individuals, where normal porosity in metaphyses, due to growth, may be misinterpreted. When investigating remains for evidence of disease, the observer should look for changes in shape and size, abnormal bone loss or formation, fractures and dislocations. The left and right sides of the body should be compared, in order to detect any asymmetries. The distribution of lesions, for example on what bones they occur and on what surfaces, is very important.
Diseases are generally divided into a number of broad categories, namely congenital (inherited), infectious, traumatic, degenerative, circulatory, metabolic and proliferative (including malignant diseases). Antemortem bony lesions are found in diseases from all these categories. Dental disease falls outside the scope of this discussion, but may be found in many other texts. In order to diagnose any of these diseases, the remains should, of course, have undergone a complete anthropological investigation, and it is assumed that the age, sex and population affinity of the individual are known since this information is often necessary before a diagnosis can be made.
There are a number of nonspecific signs of disease on skeletons, which may indicate poor health, malnutrition or anemia in general. These may help to make a general assessment of health status and living conditions of an individual, although they cannot be used for personal identification.
Congenital Diseases
Many congenital diseases are incompatible with a normal life span, and may have led to early death in prehistoric situations. With the onset of modern medicine, however, some of these conditions are treatable or manageable, and the patients may survive for longer. A case such as that illustrated in Fig. 1 would have been obviously very recognizable in life. This individual, from a modern skeletal collection, suffered from an in utero defect in the migration and closure of the first and second branchial arches which led to incomplete formation of the nose area and hypertelorism (eyes wide apart). Cases like this are extremely rare, more so in countries where modern medical facilities are available.
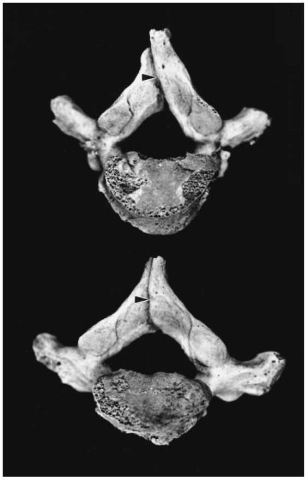
Some of the more common conditions include spina bifida, hydrocephalus, craniostenosis, and cleft palate. Spina bifida is a nonclosure of the spinal canal, where the two halves of the neural arches of the vertebrae have not fused. This occurs most commonly in the lumbosacral area. It may be asymptomatic if small, and is then called spina bifida occulta (Fig. 2). People with spina bifida may have abnormalities of the overlying skin, and sometimes also excessive growth of hair in the area. In severe cases the spinal cord is affected, resulting in neurological disorders such as paraplegia and incontinency.
Hydrocephalus involves an obstruction of the flow of cerebrospinal fluid, resulting in fluid accumulation in the lateral ventricles. Since this condition usually prevails since birth, the patients may have a very large and misshapen brain case, and in the case of young individuals the fontanelles close much later than expected, as was the case of the individual illustrated in Fig. 3. This child, although about three years old, as judged by the dentition, still had a wide open anterior fontanelle. Hydrocephalus may also be associated with other diseases of the neurological system, such as meningitis, abscesses and tumors.
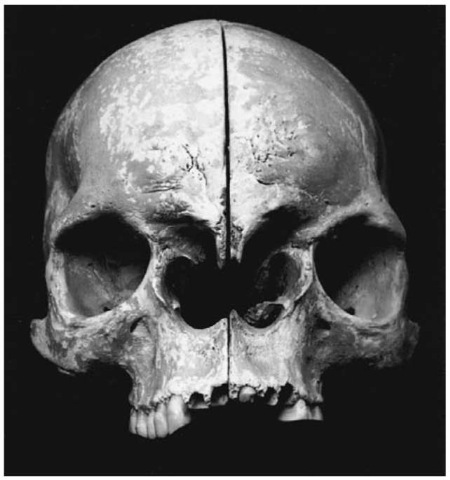
Figure 1 Individual with congenital defects of the face
Figure 2 Spina bifida occulta
In the case of craniostenosis, some of the cranial sutures close prematurely, resulting in abnormal head shapes. Premature closure of the sagittal suture, for example, will lead to an elongated head with a prominent forehead (scaphocephaly), whereas fusion of the coronal suture produces a short skull with a very high forehead. Conditions like these would have been very noticeable during life.
Cleft palate may occur alone or in combination with a cleft lip. A cleft palate is due to incomplete formation of the hard palate, whereas cleft lip also involves the maxilla. It may be complete or incomplete, unilateral or bilateral. In modern remains it can be expected that an attempt at some sort of reconstructive surgery would have been made.

Figure 3 Possible hydrocephalus in a 3-year-old child (Pretoria skeletal collection).
Figure 4 Periostitis in a long bone
Infectious Diseases
A number of infectious diseases may leave signs on bones, most of which would have been of a chronic nature. It is not possible, from bones alone, to diagnose acute diseases such as gastroenteritis or pneumonia. Advanced chronic infectious disease such as leprosy and syphilis with bone involvement are seldom seen in affluent societies, although they may be more common in less-developed countries. Osteomyelitis, on the other hand, is primarily a bone disease, and sometimes becomes chronic even after treatment with antibiotics, and may therefore be seen in all societies. Acquired immunodeficiency syndrome (AIDS), although of chronic nature, does not affect bones per se, but is often associated with other infectious diseases such as tuberculosis, syphilis, and fungal infections of the lungs. In countries where tuberculosis is common, AIDS sufferers often die of tuberculosis even without the AIDS being diagnosed.
Periostitis of bone occurs as a reaction to pathological changes on the underlying bone. It results in new bone formation by the inner layer of the periosteum, and layers of new bone are laid down on the surface of the underlying bone. These bone deposits may be irregular and of varying thickness, often with a woven appearance (Fig. 4). It may be due to infection, as in the case of osteomyelitis, or result from trauma or even in the recovery phase of deficiency syndromes (e.g. vitamin C deficiency). Periostitis is usually nonspecific, and occurs in many diseases. It may, however, sometimes lead to a definitive diagnosis. In these cases the distribution of the lesions may give valuable clues, as in the case of syphilis where the lesions are commonly found on bone surfaces close to the skin (e.g. anterior surface of the tibia).
The term osteomyelitis generally describes infection of the bone, caused by any of a number of microorganisms. Most of these infections (8090%), however, are caused by Staphylococcus aureus. Microorganisms may reach the bone (1) through the bloodstream, (2) by the extension of an adjacent infection, or (3) directly via trauma or surgery. The last two are the most common in developed countries, where the jaws and skull are often involved due to dental infections or sinusitis. It is also common in bones of the feet and hands in diabetic patients. Hematogenous osteomyelitis is more common in developing countries, where long bones of children and vertebrae of adults are often involved. The disease usually starts as an acute infection, but may become chronic in about 20% of cases.
Hematogenous osteomyelitis usually starts from the bone marrow, and then penetrates the endosteum.
The bone cortex then becomes infected, and the infection spreads to the periosteum, where it may form a subperiosteal abscess. Penetration of the periosteum may cause sinus tracts (cloacae) through the cortical bone. Small or larger portions of the bone may undergo necrosis, causing a sequestrum (fragment of dead bone). The infection may also spread to adjacent joints, causing septic arthritis. In some cases the infection may become localized and form a chronic area of infection, which is then called a Brodie’s abscess. The chronic infection may also stimulate osteoblastic activity, which results in new bone formation under the periosteum (involucrum).
Bones of individuals suffering from osteomyelitis thus show bone destruction, subperiosteal new bone formation, bone deformation, sequestration, and cloacae formation. It may also lead to excessive growth of the affected bone. Osteomyelitis usually leaves bone changes even in well-healed cases. Septic arthritis as a complication of osteomyelitis, is often destructive, and may lead to ankylosis of the bones of the joint.
Tuberculous osteomyelitis is not commonly seen in developed countries, but may occur in compromised patients (e.g. with diabetes or AIDS). In developing countries it usually occurs in young adults and adolescents. It may be slower in onset than is the case in pyogenic osteomyelitis, but is usually much more destructive and difficult to control. It is most common in the spine and long bones where it causes extensive necrosis often resulting in sinuses that drain to the skin. When it occurs in the spine it is called Pott’s disease, and here it often leads to compression fractures which in turn give rise to serious deformities such as kyphosis and scoliosis. Next to spinal involvement, the hand and foot bones are commonly affected, followed by ribs, tibia and fibula. Any joint can be diseased, and this is usually associated with infection of the adjacent bones. The knee, hip and elbow joints are most often involved. Skeletal lesions develop in less than 7% of individuals with tuberculosis.
Syphilis (Treponema pallidum), although still a common disease in many countries, very seldom progresses to a stage where the bones are involved. There are four syndromes associated with treponemal infection (pinta, yaws, nonvenereal syphilis and venereal syphilis), although they are difficult to distinguish from each other as far as the bone lesions are concerned. Some attempts have been made to do this, mostly by looking at the frequencies of involvement of various bone. Venereal syphilis is either congenital or acquired. In the congenital form the disease is transmitted to the fetus in utero via the mother. Severe disease may develop, of which the bone lesions include periostitis and diaphyseal osteomyelitis in young children, and saber-shin deformation of the tibia, gum-mata on the long bones and deformation of the teeth in older children. In acquired syphilis, the tibia is most frequently involved, followed by various bones of the skull, but virtually all bones can be affected (Fig. 5). This usually manifests as periostitis and/or osteitis and gummata. In osteitis the bone itself is affected, often with thickening and an irregular appearance of the whole bone. Due to the thickening of the cortex, the medullary cavities are small. Gummata form as a result of thrombosed blood vessels and toxic products of the microorganism. They vary in size, and may occur in the medulla or subperiosteally. The bone is destroyed in the region of the gummata, but the surrounding bone becomes sclerotic. Skull lesions typically involve erosion of the cranial vault by gum-mata and nasal-palatal destruction. Skeletal lesions occur in 10-20% of cases with venereal syphilis.
Leprosy is extremely rare in developed countries, but still occurs relatively frequently in poor tropical countries. Various skeletal manifestations that can be found include lepromatous osteomyelitis and periostitis, neurotrophic bone and joint lesions, and ordinary osteomyelitis due to secondary infection. As many as 50% of leprosy patients may have bone lesions.

Figure 5 Syphilitic lesions on a tibia (Pretoria skeletal collection). Left, diseased tibia; right, normal tibia. Note the periostitis and bowing of the affected bone.
Although all bones may be affected, the face and small bones of the hand and feet are most commonly diseased. In the face, the nasal bones, nasal spine and hard palate are often destroyed, and the upper incisors frequently lost (Fig. 6). Bone absorption is the most common feature of the hand and foot involvement, and usually starts in the distal phalanges.
Several other infectious diseases, such as brucellosis, parasitic infections and a variety of fungi may leave bone lesions, but they are relatively rare.
Traumatic
Healed traumatic lesions are possibly the most helpful of all antemortem bone changes as far as positive identification is concerned. They leave long-lasting signs, which are usually recorded on radiographs. Mostly the trauma occurs as a single incident, which may be well remembered by friends or relatives. Severe trauma is often followed by surgery, where various devices such as pins and plates are used.
It is useful to include all surgery where these devices are used into this category, although they are of course not all due to traumatic lesions. Prostheses such as hip replacements usually follow after degenerative disease (Fig. 7), whereas various forms of metal clips and/or wiring may occur in the sternum after open thoracic surgery. Other devices, such as pacemakers, silicone implants, artificial blood vessels, and heart valves, may also be associated with the remains. Although any fracture may be surgically treated, pins and plates are most commonly found on the femur (Fig. 8). In 1988 in the USA it was estimated that about 4.6% of the population had at least one medical device implant. The importance of these devices, depending on their size, is that they can usually be traced back to their manufacturers, and are often issued with a unique serial or production lot number. Manufacturers are supposed to keep records of who these devices are sold to, and in this way it can be traced back to the individual.
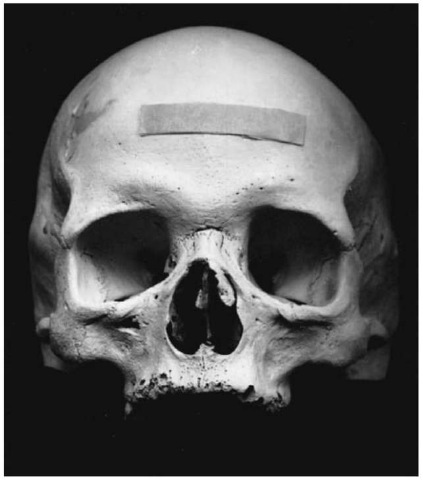
Figure 6 Forensic case with possible leprosy. Note the deformity of the nose, and the resorption of the alveolar bone resulting in antemortem loss of the upper central incisors.
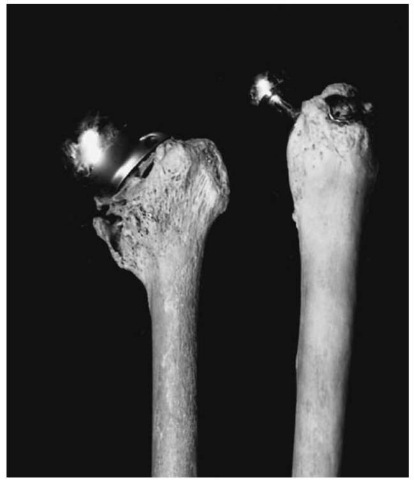
Figure 7 Prosthesis of the hip joint (Pretoria skeletal collection).
Fractures are usually either pathological, or due to trauma. Pathological fractures occur where underlying disease, such as osteoporosis or carcinoma, is present. In traumatic fractures, the type of fracture sustained depends on the amount and mechanism of force. With direct force the bone may break at the point of impact, usually with much soft tissue damage. Indirect force causes the bone to break some distance from where the trauma occurred, and therefore the soft tissue damage is less. If the direct force is tapping (direct blow), a transverse fracture is caused; if it is crushing, comminuted fractures can be caused. Indirect forces may be twisting, causing spiral fractures; angulating, causing transverse fractures; angulating combined with axial compression, causing a partly transverse fracture with a separate triangular fragment; or a combination of twisting, angulating and axial compression which causes short, oblique fractures. Avulsion fractures occur where muscle action pulls off the bony attachment of the muscle. The above descriptions apply mainly to long bones. Other bones, such as vertebrae, can sustain crush or compression fractures.

Figure 8 Surgical intervention following a femur fracture. Note the severe shortening of the bone (Pretoria skeletal collection).
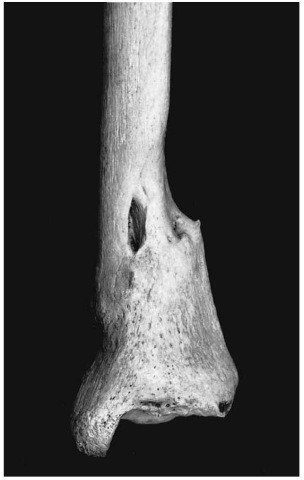
Figure 9 Healed fracture of tibia (Pretoria skeletal collection).
Fractures heal by the formation of callus (Fig. 9), which undergoes complete or incomplete resorption with time. Complications of fractures which may leave long-lasting signs on bone include incomplete healing with pseudoarthrosis (false joint formation), bone deformity, traumatic arthritis, joint fusion and traumatic myositis ossificans. Amputated limbs are easy to recognize, and may lead to a positive identification (Fig. 10). Usually fractures and their complications leave signs long after the event has occurred, thus providing a personal history of the individual.
Face and skull fractures follow after direct trauma. Depressed cranial fractures are mostly due to localized trauma, and may heal with a depressed area still visible on the skull. Healed nasal fractures are rather commonly found (Fig. 11), but fractures may be found in any of the facial bones. In severe trauma, such as motor vehicle accidents involving the face, multiple fractures are common, and surgical intervention is needed. Since the mandible is tightly fixed at its two ends, it usually fractures in more than one place.
Dislocation in itself does not leave signs on bones, but may do so if the bone remains dislocated for a significant period of time. In the case shown in Fig. 12, a secondary articular facet developed on the scapula. In this position, the arm of the individual would have been dysfunctional, and permanently laterally rotated.
Sharp trauma, such as those caused by knives, axes and pangas, may also leave signs on bones (Fig. 13). If the bone tissue around the injury shows signs of healing, the individual survived for some time after the incident. The first signs of healing after bony trauma usually appear after about 7-10 days.
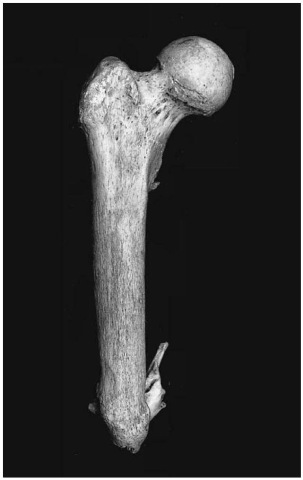
Figure 10 Amputated femur (Pretoria skeletal collection).
Peri- and postmortem trauma can be very difficult to distinguish. Perimortem trauma is usually associated with a ‘green bone response’ or bending, due to the presence of collagen in the bone. Fresh bones may splinter, forming irregular edges. Dry bone is usually brittle, and postmortem trauma may therefore produce shattering resulting in smaller bone fragments.
Degenerative
Degenerative disease may also be helpful in determining the identity of an individual. It usually occurs in older individuals. Radiographs of the diseased joint often exist, and in some cases surgical procedures, such as implantation of prostheses, may have been done. In a case from South Africa, for example, the body of an elderly individual with severe arthritis of the hip was discovered near a small town. Positive identification was easy when records of a missing person were found who was already booked in for a hip replacement.

Figure 11 Healed nasal and zygomatic fractures (Pretoria skeletal collection).
Although there are many causes of arthritic disease, only a few can be diagnosed with the help of dry bone only. These are osteoarthritis, vertebral osteophyto-sis, traumatic arthritis, rheumatoid arthritis, ankylos-ing spondylitis, infectious arthritis and gout. Of these diseases, only osteoarthritis and vertebral osteo-phytosis are truly degenerative in nature.
Bone changes due to old age are very common, and can be seen in most people over the age of 50.

Figure 12 Forensic case with secondary articular facet for head of humerus on scapula.
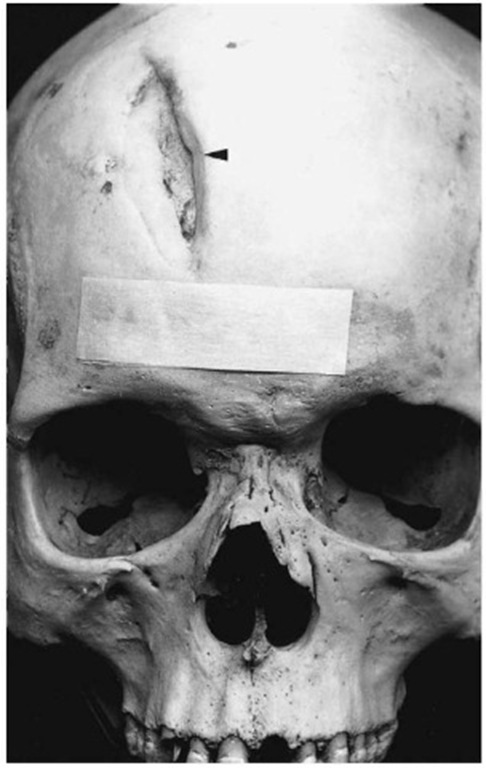
Figure 13 Healed sharp trauma on the skull (Pretoria skeletal collection).
Osteoarthritis is usually characterized by deterioration of the joint cartilage and formation of new bone near the joint surfaces. The subchondral bone shows irregular pits, and lipping or osteophytes form near the margins of the joint. If the overlying cartilage completely disappears, the bone is exposed. The bone may then become sclerotic with a polished (ebur-nated) appearance (Fig. 14). Weight-bearing joints, such as the hip and knee, are most commonly affected, whereas distal interphalangeal joints are also frequently affected. Although more than one joint is usually affected, the disease is not as generalized as is the case with rheumatoid arthritis.
Rheumatoid arthritis is an autoimmune disease. It affects many joints, including proximal interphalan-geal, metacarpophalangeal, tarsal and temporoman-dibular joints. It occurs in younger individuals, and females are more often affected than males. Osteoporosis of adjacent bones, subluxation and ankylosis may be found.
Degenerative disease of the vertebrae may involve the apophysial (facets of the vertebrae) or interver-tebral joints and is characterized by osteophytes. This condition is so common that it is unlikely to help in a positive identification. Its presence may, however, confirm that the remains are of an elderly individual.
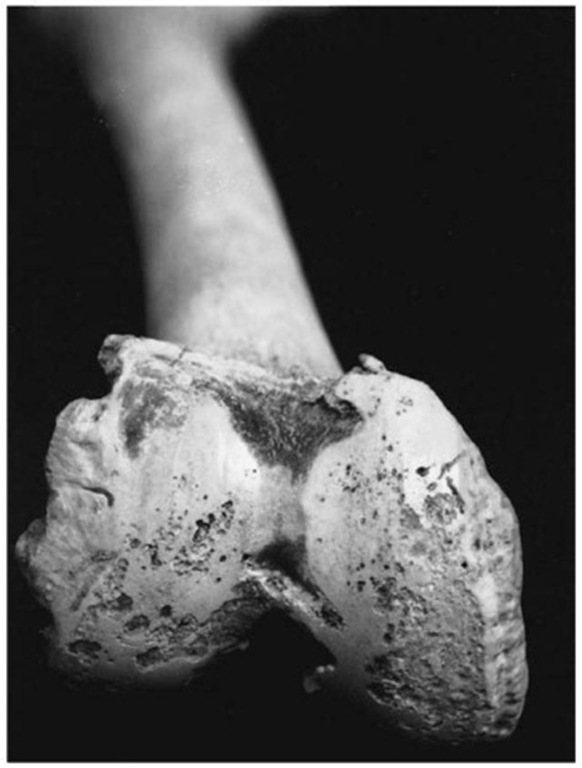
Figure 14 Eburnation of distal femoral joint surface (Pretoria skeletal collection).
Circulatory Diseases
There are very few circulatory diseases which involve bone. In Perthes’ disease, for example, the epiphyses of the head of the femur undergoes aseptic avascular necrosis. It mostly occurs in boys between 5 and 10 years. The head of the femur usually flattens, and the neck thickens. After revascularization the head of the femur is mushroom-shaped with an overhanging margin.
Aneurisms (saccular dilatation of an artery) may erode closely situated bone. Aortic aneurisms, for example, may erode the posterior surface of the sternum. This mostly happens in syphilitic aortitis, but is uncommon.
Metabolic Diseases
Examples of metabolic diseases that may influence bone include endocrine diseases, osteoporosis, Paget’s disease, deficiencies (e.g. vitamin C) and gout. Although nutritional diseases are relatively rare in developed countries, many people, mostly from Africa and Asia, suffer from primary malnutrition. Therefore, diseases such as scurvy (vitamin C deficiency) and rickets (vitamin D deficiency) may be found in skeletal remains of children especially. Skeletal signs of scurvy may show as transverse fractures in the metaphysis near the epiphyses, thin bone cortex and reactive periosteal bone deposition. Rickets leads to bone deformation, softened cranial bones (craniotabes), frontal bossing and the formation of a square head, and a pigeon chest (sternum projecting anteriorly).
Endocrine diseases include, among others, gigantism or acromegaly and dwarfism. Excessive production of growth hormone (somatotropin) leads to gigantism when it starts in the growing years and acromegaly when it begins in adults. Acromegaly is usually due to a tumor of the pituitary and is, therefore, usually associated with an enlarged sella turcica. Since epiphyseal plates are already closed, only the periosteum and cartilage can respond to the stimulation of the growth hormone. The result is elongation of the mandible and bony buildup at the chin, enlarged hands and feet, accentuated supraorbital ridges, enlargement of the facial bones and thickening of the cranial vault. A deficiency of growth hormone may lead to dwarfism.
Osteoporosis is an extremely common disease, in which the bones lose their density and become fragile. It is more common in women, especially after the menopause. This disease is too common and nonspecific to be of any use in personal identification, but its presence usually indicates an older individual.
Paget’s disease usually starts after 40 years of age, and becomes more and more prevalent thereafter. It is common in Caucasoids of Europe, North America, Australia and New Zealand, and reaches a frequency of 10% in males and 15% in females by about 90 years of age. It is rare in native Asians and Africans. The disease occurs in three phases: first an initial osteolytic stage; then a mixed osteolytic-osteoblastic stage; and finally a burnt-out osteosclerotic state. Virtually any bone of the skeleton can be affected, and in skeletal remains it is often seen as sclerotic, thickened and enlarged bones. Medullary spaces are diminished, and the distinction between cortex and medulla is obscured. Thickening of the bones of the skull vault is frequently seen. Although signs of Paget’s disease on bone are quite obvious, the disease may be asymptomatic or not diagnosed. Symptoms may include pain due to small fractures, increase in head size, and nerve impingement due to foraminal narrowing. Sarcomas may develop on affected bone.
Proliferative Diseases
Proliferative diseases affecting bone include a whole range of conditions, often malignant in nature. Benign tumors of bone include osteomata and osteoblastoma. ‘Ivory’ or ‘button’ osteomata are commonly found on bones of the cranial vault (Fig. 15), but usually it does not have any clinical significance.
Malignant tumors may be either primary or meta-static. Primary bone malignancies usually occur in younger, and metastases in older individuals. Primary malignant bone tumors include osteosarcoma, chon-drosarcoma, and Ewing’s sarcoma. Osteosarcoma most frequently occurs in adolescence, and affects males more commonly than females. It is usually associated with enchondral growth, and commonly appears in the metaphyses of the distal femur, proximal tibia and proximal humerus. The appearance may range from total lytic lesions (destruction of bone), to the formation of massive sclerotic bone.
Multiple myeloma is a plasma cell tumor, which manifests as multifocal destructive bone lesions throughout the skeleton. The lesions appear as punched-out, circular defects. This disease occurs in older individuals, and males and females are equally affected.
Various carcinomas metastasize to the skeleton, but they occur less frequently in sarcomas. The most common tumors to metastasize to the skeleton are breast cancer in women and prostate cancer in men. The bones most commonly involved are the spine, femur, ribs, sternum and skull. Fast-growing tumors are usually lytic in nature, and slow-growing tumors osteosclerotic.
Nonspecific Markers of Disease
There are various signs of disease that may act as nonspecific indicators of stress and/or malnutrition.

Figure 15 Ivory ‘button’ osteomata on the skull (Pretoria skeletal collection).
Although they are not useful in making personal identifications, they give some indication of the living conditions and socioeconomic background of an individual.
Enamel hypoplasia of the teeth present as horizontal lines or pits in the enamel. They are indicative of periods of malnutrition and acute disease/fever during the developmental phase of the teeth which are severe enough to inhibit normal enamel formation. The age at which the defect formed can be calculated from the distance between the hypoplastic line and the cement-enamel junction.
The etiology of transverse radio-opaque lines (Harris lines) of long bones is the same as for enamel hypoplasia. These lines, which can be seen on radiographs, are formed when the normal growth at the epiphyses had stopped, and then started again. The number of lines may serve as an indicator of the amount of stress/disease during the growing years.
Cribra orbitalia refers to pitting in the roof of the orbit, but if it is severe it may also involve the rest of the skull (porotic hyperostosis). Currently the general conclusion seems to be that this is the result of longstanding anemia. The anemia causes bone marrow hyperplasia, resulting in the pitted appearance of the overlying bone.
Conclusions
The importance of health assessment and reconstruction of life from the skeleton has been discussed in a number of forensic anthropology topics. It is important to note that assessment of health from skeletal remains is significant in a number of forensic matters; for example, it may give an indication of socioeconomic status. Diseases like osteomyelitis are rare in affluent countries and may more often be associated with individuals of lower socioeconomic status or those living in undeveloped countries. This same assumption may also be made for individuals with inadequate dental care. A correctly diagnosed skeletal lesion of antemortem origin can also lead to the identification of missing people. This is especially true for individuals with previous fractures who are readily recognized by members of their community, or who have detailed medical records. Correct assessment of a lesion can also aid in determining the manner of death. If a claim is made that the deceased died of cranial fractures, it is possible to observe if the fractured area shows evidence of bone remodeling. The presence and amount of growth or healing may lead the investigator to conclude that the fractures have occurred sometime before death.
When advanced disease is present on bones of forensic origin, there may be a question of whether the cause of death was, in fact, natural. Cause of death can be very difficult to determine when these kinds of chronic disease are present. It should be kept in mind that the observed disease may not have been fatal. Since bodies are usually not discovered in unusual places or buried in shallow graves, it is recommended that they are treated as potential unnatural deaths. This is obviously the case in affluent countries, although the situation in undeveloped countries with large rural areas may be different. In these countries it is possible that the recovered remains were those of homeless people dying of natural causes in less inhabited areas.
Antemortem diseases of bone are often difficult to diagnose specifically, and it is recommended that specialist opinions be sought. Radiographs should be taken in all cases to confirm the diagnosis. Modern investigative techniques, such as tomography and magnetic resonance imaging may also help in diagnosis. With the increased development of techniques for DNA extraction from bone, the diagnosis of infectious diseases from the DNA of microorganisms may also be possible.
The most important principle in the evaluation of antemortem disease remains the careful, systematic observation of every bone. It is unfortunate that record keeping of patients by physicians and dentists is not uniformly carried out in every country. Therefore, sometimes even a correct diagnosis of ante-mortem pathology of a deceased individual may not lead to a positive identification.