Introduction
Drug detection in postmortem specimens has many uses, all of which assist the investigating authorities in providing the relevant information pertaining to a case (Table 1). Ultimately, toxicology testing results will assist the coroner, medical examiner or equivalent in establishing evidence of drug use, or by refuting the use of relevant drugs. This latter is important because a pathological examination will often not show indicia suggestive of drug use. Drug use can only be confirmed by appropriate toxicology testing procedures. Clearly, in cases of sudden and unexpected death, use of drugs may provide a cause of death, or at least provide evidence of drug misuse or drug abuse. (‘Drug misuse’ is used here to define cases where inappropriate doses or drug combinations have been used, whereas ‘drug abuse’ is restricted to deliberate and usually recreational use of drugs of abuse. Neither term necessarily implies suicidal intent.)
Toxicology testing is particularly important in victims of homicide, to whom drugs may have been given by the assailant to reduce consciousness, and in cases in which drugs were used by the victim. In this latter scenario, modification of behavior by drug use may be important in criminal trials, not necessarily to mitigate the intent by the accused, but primarily to reconstruct, as far as possible, the events that led to the act. Such reconstruction may involve corrobora-tion of witness accounts of drug-using behavior.
Typical drugs used in these cases are alcohol, amphetamines, cocaine or one of the benzodiazepines (alprazolam, diazepam, flunitrazepam, etc.). Victims or perpretrators of violent crime may also have consumed medication to treat a psychiatric problem or a host of other medical conditions. The presence of
Table 1 Reasons for drug testing in postmortem cases.
Establishing drug use in victims of homicide Establishing drug use in drivers of motor vehicles Establishing drug use in persons involved in workplace accidents Establishing drug use in other cases of sudden and unexpected death
Assisting investigators with estimation of timing of drug ingestion drugs may therefore be indicative of such treatment, or at least confirm the person concerned has taken the medication. In some cases these medications may even have contributed to behavioral problems.
In practice, deceased persons have often consumed two or more drugs, and in many cases the investigating authority (pathologist, coroner, etc.) is not aware of all the drugs being used. Since the great majority of cases (> 70%) involve more than one drug, it is advisable to conduct a broad drug screen to include most of the common drugs, rather than target the analysis to one or a limited range of drugs suggested by the circumstances. This will also allow experts to determine if any adverse drug interactions have occurred.
Specimens
The preferred specimens collected at postmortem will depend on the type of case. Most typically, one or more blood specimens and urine are collected, although as Table 2 illustrates, a number of other specimens should be taken in certain case types. A useful forensic technical procedure in the autopsy suite is to take a ‘full’ set of specimens in all but the most obvious natural cause investigations. This will avoid the embarrassment of collecting insufficient or inappropriate specimens and give the toxicologist the best chance to complete the analytical investigation satisfactorily.
Blood is the most useful specimen that can be collected because drugs present in this fluid can best be related to a physiological effect and can be used to assess the likelihood of recent drug use or exposure to chemicals. A number of problems are associated with the collection of this fluid in cadavers. Two 10 ml samples of blood are recommended, one to be used for blood alcohol analyses and the other for blood toxicology. The splitting of the two blood specimens reduces the possibility of contamination in the laboratory and enables the blood alcohol specimen to be retained separately from the other blood specimen. Forensic technicians or pathologists should be aware that the collection of peripheral blood reduces the possibility of postmortem artifacts frustrating interpretation of any positive results (see Redistribution). The preferred collection site is the femoral region (leg); however, failure to ligate the femoral vessels can allow ‘contaminated’ abdominal blood to be withdrawn. Autopsy procedures should therefore accomodate these problems. Drug content is reported as milligrams per liter.
Urine is the second most important specimen collected. Since concentrations of drugs and metabolites of drugs are usually much higher than in blood, urine provides a valuable specimen for assessing drug use over the previous day or two. Urine can be collected after the opening of the abdomen, or by direct puncture of the bladder. An autopsy is therefore not necessary for collection of this specimen, or even blood and vitreous humor (see later). Drug content is normally reported as milligrams per liter.
Table 2 Recommended minimum specimens to be collected post mortem.
| Type of case | Recommended specimens collected |
| All cases | Peripheral blood (2 x 10 ml) |
| Urine (10 ml) | |
| Vitreous humor (2-5 ml) | |
| Homicides and suspicious cases | Liver, bile |
| Drug-related cases | Gastric contents, bile, liver |
| Volatile substance abuse cases | Lung fluid or tied-off lung, liver |
| Biochemical abnormalities (insulin, etc.) | Serum |
| Heavy metal poisoning | Liver, hair, kidney |
Vitreous humor is an ideal fluid to collect with ‘positive’ blood because the alcohol content of vitreous humor is very similar to that of blood and can prove useful in excluding putrefactive formation of alcohol in blood and visceral contamination. Vitreous humor is also a useful fluid for a range of drugs, including digoxin and antidepressants, as well as a number of biochemical markers. Since vitreous humor can be easily collected, it is strongly recommended that this specimen is included in a routine, sudden death investigation. Drug content is normally reported as milligrams per liter.
The liver is traditionally a favored tissue for toxicologists because drugs are often found in higher concentrations there than in blood, it can be readily homogenized and, of course, it is the main metabolic organ. A liver sample should be collected in all cases of suspected drug use. A 100 g aliquot is sufficient for most analyses. The right lobe is preferred, as this is least subject to postmortem diffusion of drug from bowel contents and the mesenteric circulation (see Redistribution). Drug content is normally reported as milligrams per kilogram of wet weight tissue.
Gastric content is invaluable in cases of suspected poisoning. The aim of using this specimen is to establish the actual content of drug (or poison) remaining in this organ at death, and it may allow the route of drug administration to be determined. Drug residues can be isolated by direct extraction with methanol, or another solvent, and analyzed by conventional chromatographic techniques. When little or no fluid is present in the stomach, provision of the whole stomach allows the analyst to dissolve any drug adhering to the sides of the walls. Toxicologists should be aware that small quantities of drug will derive from the bile, especially during agonal processes, hence drug content in the stomach does not necessarily imply oral ingestion. Results should be reported as milligrams (total gastric content).
Lung fluid, or tied-off lungs, are recommended in cases of suspected volatile substance abuse. Since quantitative results are rarely interpretable, ‘detected’ or ‘not detected’ results alone are usually sufficient (Table 3).
Bile is a useful fluid for morphine/heroin detection because biliary concentrations are much higher than in blood. A number of other drugs are also found in bile in relatively high (and therefore more easily detectable) concentrations, including other narcotics, benzodiazepines and glucuronide metabolites. Report bile results as milligrams per liter.
Occasionally other specimens can provide valuable information in a case. Hair can provide a history of drug use, or exposure to chemicals if chronic exposure is thought to occur. Hair can therefore provide evidence of drug use for much longer periods of time than urine. The relation between dose and hair concentration is usually poor, although some comparisons can be made as to the extent of drug use, e.g. regularity of heroin use. Hair concentrations are normally reported as micrograms per gram weight.
Table 3 Useful substance detections in various tissues.
| Tissue | Substances detected |
| Blood/urine/liver/hair/ | All drugs and poisons |
| gastric contents | |
| Vitreous humor | Alcohol, antidepressants, narcotics, |
| creatinine, urea, glucose | |
| (>10 mmolr1) | |
| Bile | Morphine and other narcotics, |
| benzodiazepines | |
| Lungs | Volatile substances (toluene and |
| other solvents, butane and other | |
| aerosol gases, automobile and | |
| aviation fuels) |
Samples of brain tissue may be more relevant for some centrally active (i.e. in the brain and spinal cord) drugs, such as morphine; and skin (with associated subcutaneous tissue) may show large deposits ofdrugs left behind after an injection. Results are normally expressed as milligrams per gram wet weight tissue.
In cases of extreme putrefaction, the recommended list of specimens will no longer be appropriate. Muscle tissue, hair and bone can be useful specimens in this type of case, although the physical state of the body will determine what specimens are available for collection. Body fluids will be present in some putrefied bodies but this is no longer blood, rather liquified tissues; but this fluid can be used to screen for the presence of drugs. Quantitative results are of little use in badly putrefied cases.
General Techniques
The range of techniques available for the detection of drugs in the specimens collected post mortem are essentially identical to those collected ante mortem. These range from commercial kit-based immuno-assays (enzyme multiplied immunoassay technique (EMIT), fluorescence polarization immunoassay (FPIA), cloned enzyme donor immunoassay (CEDIA), radioimmunoassay (RIA), etc.), traditional thin-layer chromatography (TLC), to instrumental separation techniques such as high-performance liquid chromatography (HPLC), gas chromatography (GC) and capillary electrophoresis (CE). Mass spec-trometry (MS) is the definitive technique for establishing proof of structure of an unknown substance and can be linked to GC, HPLC and more recently to CE.
The specimens analyzed in postmortem cases are most often blood and liver, rather than urine and serum, which are used in antemortem analysis, and the other specimens listed earlier. The use of blood and liver, and indeed all other postmortem specimens, require separate validation to those methods used in antemortem analysis. The methods used require modification to ensure a reliable extraction recovery, a low level of interference and reproducible quantitative results. Special attention to these factors is required on partly or fully putrefied specimens to ensure lack of interference from endogenous substances. Cutoff values often used in workplace, sports and drugs-of-abuse testing are no longer appropriate in postmortem cases involving specimens other than urine. Even postmortem urine should not normally be tested to cutoff limits used in drugs-of-abuse testing because the presence of a small concentration of drug may be of forensic significance.
The range of immunoassays used in antemortem analysis can also be used in postmortem analysis,providing suitable modification of the preparation of the specimen is conducted. Urine-based kits can be used for urinalysis; however, blood or tissue homogenates require special treatment to remove matrix effects. Urine is often unavailable in pos-mortem cases. Precipitation of blood proteins by treatment with methanol, acetonitrile, dimethylform-amide or acetone, and direct analysis of the supernatant are frequently used techniques; however, the high-potency drugs are not always detected. Prior extraction of blood or liver homogenates with a solvent (e.g. butyl chloride) provides an improved detectability, as a concentration step can be employed and most interference has been removed. Not all drugs are extracted with all of these techniques. Individual validation must be conducted to ensure adequate detectability for target drugs and to determine the range of drugs that can, and those that cannot, be detected.
False-positive results with immunoassays occur, either from structurally related drugs, or from metabolites of other drugs that are recognized by the antibodies. While HPLCand GCtechniques are more specific than immunoassays, any positive result should be confirmed by mass spectral identification, unless sufficient validation of another method has been conducted to assure courts of the reliability of the result. Unconfirmed drug results, if reported, should be flagged as presumptive, or words with similar intent.
Solid-phase extraction, using small columns to absorb drug selectively from the matrix (e.g. Extrelut, Sep-Pak, Bond-Elut, etc.), provides an excellent alternative to conventional liquid-liquid extraction techniques. Solid-phase techniques have been published for most analytes, tend to be quick, often provide clean extracts and can be readily automated.
The use of deuterated internal standards provides an ideal way to monitor changes in chromatographic performance, and, most importantly, essentially eliminates matrix effects caused by poor recoveries of drug. While recoveries of drug may vary from one matrix to another, and even between calibrators, the deuterated internal standard will correct for this. For this reason, assays involving MS should use deuter-ated internal standards wherever possible in postmortem analyses.
Recommended Techniques for Postmortem Analysis
As indicated before, it is important that a drug screen encompass the widest number of drugs and poisons without seriously compromising the ability of the laboratory to work on sufficient cases. Urinanalysis (or blood or another fluid) using one of the commercial immunoassays, or even TLC, is recommended for the main classes of drugs. These usually include amphetamines, barbiturates, benzodiazepines, can-nabinoids, cocaine metabolites and morphine-like opiates.
In addition, a series of other (usually chromato-graphic) tests is strongly recommended. The schema shown in Fig. 1 illustrates a typical analytical profile for routine case screening of blood. Blood is analyzed for alcohol and is subject to a few screening techniques aimed at capturing a wide selection of chemical substances to which humans are likely to be exposed.
An acidic screen includes the nonnarcotic analgesics (acetaminophen, aspirin), the nonsteroidal antiinflammatory drugs (naproxen, ketoprofen, ibuprofen, etc.), many of the diuretics (frusemide,hydrochlorothiazide, etc.), the anticonvulsants (car-bamazepine, lamotrigine, phenobarbital, phenytoin, valproate), barbiturates and the more potent benzo-diazepines, the xanthines, theophylline and caffeine. The use of a solvent extraction technique at acidic pH, or simple precipitation of blood proteins with acetonitrile, enables these substances to be detected by gradient HPLCwith multiwavelength or photo-diode array detection.
A basic extraction procedure using butyl chloride (preferred solvent, but others are also suitable), or a solid-phase extraction procedure using octadecyl-bonded cartridges or mixed-phase cartridges, will provide a reasonably clean extract from postmortem blood (and other tissues) for analysis by capillary GC. The use of an MS detector is preferred (to allow simultaneous detection and confirmation), although a nitrogen-phosphorus detector (NPD) will provide a higher sensitivity for many substances than full-scan MS. Electron capture detectors (ECD) are extremely useful for benzodiazepines. The use of dual detectors (NPD and MS, or NPD and ECD) provide an additional degree of specificity and detection over one detector alone.
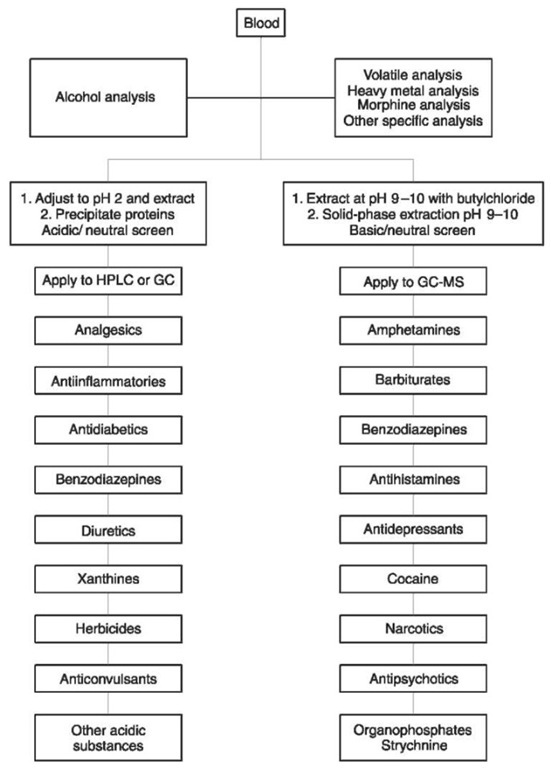
Figure 1 Extraction steps for blood analyses and substance classes likely to be detected. GC, gas chromatography; GC-MS, GC mass spectrometry; HPLC, high-performance liquid chromatography.
These two screening procedures will also enable a number of unusual poisons to be detected. Organo-phosphates and strychnine are readily detected by GC-NPD, while HPLC of acid extracts enables detection of a number of herbicides and other agricultural chemicals. If circumstances suggest volatile substance abuse, exposure to heavy metals, lysergic acid diethylamide (LSD) and other nonamphetamine hallucinogens, or other noxious substances not covered earlier, specific additional tests will need to be performed. It is advisable to perform a blood test for morphine if heroin or morphine use is suspected (or needs to be ruled out) and the urine test for opiates is negative, as morphine does not chromatograph well underivatized. Heroin deaths have been missed if screening for morphine is restricted to urine because acute deaths in naive users may not show morphine in urine.
Postmortem Artifacts in Analysis
Dying imparts a number of special processes that affect the collection and analysis of specimens obtained at autopsy.
Redistribution
Foremost is the process of redistribution, which affects all analyses in which concentrations of drugs in blood and tissues alter due to disruption of cellular membranes, causing alterations of drug concentrations within tissue elements and diffusion from one tissue to another. This process is particularly significant for drugs with high lipid solubility, as these drugs tend to show concentration differences in tissues and blood. Table 4 shows the extent of these changes for selected drugs when comparisons are made between blood collected from the heart and that collected from the femoral region.
The femoral blood is least subject to redistribution after death; however, drugs with much higher concentrations in muscle tissue will still diffuse through the vessel walls and elevate the neighboring blood concentrations. If the femoral vessels are not tied off from the vena cava and aorta, then the process of drawing blood can also extract blood from the abdominal cavity that has been contaminated from diffusion of gastric and intestinal contents. It is therefore advisable to reduce these processes by collecting blood specimens as soon as possible after death from the femoral region, with blood vessels tied off to reduce contamination.
Table 4 Likely extent of postmortem redistribution for selected drugs.
| Drug/drug class | Redistribution3 |
| Acetaminophen | Low |
| Alcohol (ethanol) | Low |
| Barbiturates | Low to moderate |
| Benzodiazepines | Low to moderate |
| Cocaine | Low |
| Digoxin | Very high |
| Methadone | Moderate |
| Morphine | Low |
| Phenothiazines | Moderate to high |
| Propoxyphene | Very high |
| Salicylate | Low |
| Serotonin reuptake inhibitors | Low to moderate |
| Tricyclic antidepressants | High |
These processes are not limited to blood. Liver and lung tissue show differences in the concentration of drugs, depending on the nature of the drug and whether diffusion of drug has occurred from neighboring tissues or the blood supply. For example, the left lobe of the liver is more likely to exhibit elevated drug concentrations than the right lobe.
Metabolism and byconversion
A number of drugs can undergo chemical changes in the body after death. These chemical changes can be either metabolically mediated or caused by spontaneous degradative processes. For example, the metabolism of heroin to morphine occurs in life and also occurs in recently deceased persons by the action of blood and liver esterases. For this reason, heroin or the intermediate 6-monoacetyl morphine are rarely detected in cadaveric tissues. Morphine is therefore the target drug. Aspirin is converted rapidly to salicy-late by hydrolytic mechanisms. Most prodrugs activated by de-esterification or hydrolysis will be subject to similar processes.
Nitro-containing drugs, such as the benzodiaze-pines, nitrazepam, clonazepam, nimetazepam, fluni-trazepam and others, are also rapidly biotransformed after death to their respective amino metabolites by the action of certain types of bacteria (obligate anaerobes). Toxicologists must therefore target their analyses to these transformation products rather than the parent drug.
Sulfur-containing drugs, such as dothiepin, thio-pental, thioridazine, etc., are also subject to bacterial attack post mortem, leading to progressive losses over time during putrefaction. Of course, the parallel process of tissue loss will also affect the tissue concentration during putrefaction.
Chemical instability occurs in a number of drugs and metabolites even when specimens are stored frozen at — 20°C. Some benzodiazepines and benzo-diazepine metabolites, antipsychotics such as thior-idazine, and the p-stimulant fenoterol show time-dependent losses. Stability characteristics have not yet been evaluated for many drugs.
Alcohol will be lost to evaporation unless sealed tubes are stored at — 60°C, however, alcohol can also be produced by bacterial action on glucose and other sugars found in blood. The use of potassium fluoride as preservative (minimum 1% w/v) is required to prevent bacterial activity for up to 1 month after collection, when stored at 4°C.
Reports
Once an analysis is complete, a report that accurately details the analytical findings must be issued to the client(s). These results should indicate the type of tests conducted, the analytical method used (i.e. HPLC, GC-MS, etc.), on which specimens the analyses were conducted, and, of course, the result(s). The result(s) should be unambiguous, using such terms as ‘detected’ or ‘not detected’. The use of the term ‘not present’ should be avoided, as it implys no possiblity of the substance being present. A toxicologist can rarely be so definite and can only indicate that a substance was not detected at a certain threshold concentration. A detection limit should therefore be provided when tests for specific substances produce ‘not detected’ results.
For quantitative results, consistency in units is advised and should not be given with more significant digits than the accuracy will allow. For example, there is no point in reporting a result for blood morphine as 0.162mgl — 1 when the accuracy and precision of the method is +20%. A result of 0.16mgl — 1 would suffice.
For drug screening results, it is advisable to provide clients with an indication of the range of substances a method is capable of detecting, and some indication of the detection limits, i.e. ‘at least therapeutic concentrations’ or ‘only supratherapeutic concentrations’. Positive immunoassay results should also be reported even if this presumptive detection has not been confirmed. This information can be useful because it may imply (to an expert later investigating the case) that the substance may have been present but at very low concentrations, or there was another immu-noreactive compound which was not excluded in the confirmation assay. To exlude these results could be construed by courts as a deliberate withholding of evidence.
To enable proper interpretation of evidence, all reports should indicate the site of blood sampling, and provide, where relevant, some comment on the possibility of postmortem artifacts, such as redistribution. By incorporating these comments, uninformed persons reading the report are less likely to unwittingly misinterpret the results.
