Definitions
The consequences for the patient when drug concentrations either fall below the therapeutic window or exceed it can be life threatening. The rate of removal of the drug from the body determines whether it will disappear from, or accumulate in the patient’s blood. A concept has been devised to understand and measure rate of removal; this is known as ‘Clearance’. This term does not mean that the drug disappears or is ‘cleared’ instantly. The definition of clearance is an important one that should be retained:
Clearance is the removal of drug by all processes from the biological system.
A more advanced definition could be taken as:
A volume of fluid (plasma, blood or total body fluid) from which a drug is irreversibly removed in unit time.
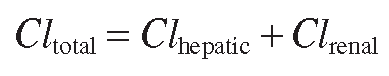
Clearance is measured in millilitres of blood or plasma per min (or litres per hour) and is often taken to mean the ‘clearance’ of the drug’s pharmacological effectiveness, which resides in its chemical structure. Once the drug has been metabolized, or ‘biotransformed’, even though only a relatively trivial change may have been effected in the structure, it is no longer as it was and products of metabolism, or metabolites as they are known, often exert less or even no therapeutic effect. Whether or not they retain some therapeutic effect, metabolites are usually removed from the cell faster than the parent drug and they will eventually be excreted in urine and faeces. There are exceptions where metabolites are as effective as the parent drug (some tricyclic antidepressants, such as desipramine and morphine glucuronides), and there are metabolites that are strangely even less soluble in water and harder to excrete than the parent compound (acetylated sulphonamides), but in general, the main measure of clearance is known as total body clearance, or sometimes, systemic clearance:
This can be regarded as the sum of all the processes that can clear the drug. Effectively, this means the sum of the liver and kidney contributions to drug clearance, although the lung and other organs can make some contribution.
For drugs like atenolol or gabapentin, which unusually do not undergo any hepatic metabolism, or indeed metabolism by any other organ, it is possible to say that:
So renal clearance is the only route of clearance for these drugs, in fact it is 100 per cent of clearance.
For paracetamol and for most other drugs, total body clearance is a combination of hepatic and renal clearances:
For ethanol, you will probably already be aware that there are several routes of clearance, including hepatic, renal and the lung, as breath tests are a well-established indicator of blood concentrations.
Once it is clear what clearance means, then the next step is to consider how clearance occurs.
Means of clearance
In absolute terms, to clear something away is to get rid of it, to remove it physically from the system. The kidneys are mostly responsible for this removal, known as elimination. The kidneys cannot filter large chemical entities like proteins, but they can remove the majority of smaller chemicals, depending on size, charge and water solubility. The filtrate eventually reaches the collecting tubules that lead to the ureter and the bladder. As the kidney is a lipophilic (oil-loving) organ, even if it filters lipophilic drugs or toxins, these can easily leave the urine in the collecting tubules and return to the surrounding lipophilic tissues and thence back to the blood. So the kidney is not efficient at eliminating lipophilic chemicals.
One of the major roles of the liver is to use biotransforming enzymes to ensure that lipophilic agents are made water soluble enough to be cleared by the kidney. So the liver has an essential but indirect role in clearance, in that it must extract the drug from the circulation, biotransform (metabolize) it, then return the water-soluble product to the blood for the kidney to remove. The liver can also actively clear or physically remove its metabolic products from the circulation by excreting them in bile, where they travel through the gut to be eliminated in faeces. Bacterial effects on this process can lead to the reabsorption of the metabolite or parent drug into the gut, a process known as enterohepatic recirculation.
The liver has an impressive array of enzymatic systems to biotransform drugs, toxins and other chemical entities to more water-soluble products. However, the ability of the liver to metabolize a drug can depend on the structure and physicochemical characteristics of the agent, so some drugs are easy for it to clear and some are difficult.