High extraction drugs
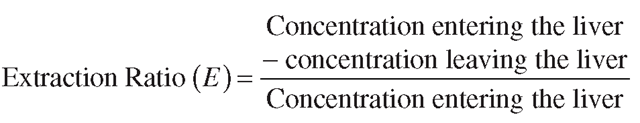
Hepatic extraction is a useful term to measure how easily the liver can process, or metabolize, a given drug or toxin. The term ‘hepatic extraction’ effectively means the difference between the drug level in blood that enters the liver (100 per cent) and the amount that escapes intact and unmetabolized (that is, 100 per cent minus the metabolized fraction). Extraction is usually termed E and is defined as the extraction ratio, or
Clinically, most drugs ’ hepatic extraction ratios will either be high (E > 0.7), or low (E < 0.3), with a few agents falling into the intermediate category (E is >0.3, but <0.7). For high extraction drugs, the particular enzyme system that metabolizes this drug may be present in large amounts and drug processing is very rapid. This often happens if the drug is very similar in structure to an endogenous agent, which is normally processed in great quantity on a daily basis. Hence, the early anti-HIV drug AZT (zidovudine), is a close structural analogue of the DNA constituent thymidine and so possesses a half-life of an hour or less in man. In the case of a high extraction drug, the inbuilt or ‘intrinsic’ ability of the liver to metabolize the drug means that the only limitation in the liver’s ability to metabolize this type of drug is its rate of arrival, which is governed by blood flow.
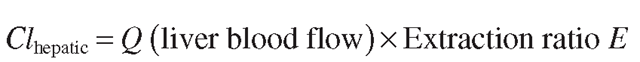
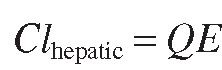
So, in the case of a high clearance drug, where the liver’s intrinsic ability to clear it is very high:
i.e.
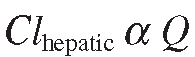
So, basically, hepatic clearance is directly proportional to blood flow:
During intensive exercise, human liver blood flow can fall temporarily by more than 70%, but during normal day-to-day living, blood flow through the liver does not normally vary that much. This means that a high extraction drug will be cleared at a fairly predictable rate. However, hepatic blood flow can be significantly reduced in old age and end-stage cirrhotic alcoholism.Patients with impaired cardiac output, either as a result of congestive heart failure or myocardial infarction, also experience marked reductions in liver blood flow. All these circumstances have been shown to reduce the clearance of high extraction drugs clinically and should be borne in mind during drug dosage determination in these patients.
Many drugs are bound in plasma to proteins such as human serum albumin (HSA) or alpha-1 acid glycoprotein (AAG). HSA usually transports endogenous acidic agents, such as fatty acids, bilirubin and bile acids, although it also binds drugs such as warfarin, ibuprofen and diazepam. The endogenous function of AAG is not fully understood, but may involve modulation of the immune system. AAG will bind basic drugs such as erythromycin and protease inhibitors.
Usually, for any given drug, there is equilibrium between protein-bound and free drug. In effect, high extraction drugs are cleared so avidly, that the free drug disappears into the metabolizing system and the bound pool of drug eventually becomes exhausted. As the protein binding of a high extraction drug is no barrier to its removal by the liver these drugs are sometimes described as undergoing ‘unrestricted’ clearance. Drugs in this category include pethidine (known as meperidine or Demerol in the US), metoprolol, propranolol, lignocaine, nifedipine, fentanyl and verapamil.
You also might see the term ‘intrinsic clearance’ which reflects the inbuilt ability of the liver (independent from other variables like blood flow) to remove a drug; high extraction drugs have a high intrinsic clearance. As mentioned above, the only limitation in clearance for these drugs is how much drug the blood can deliver. If blood flow was to be infinite, then hepatic clearance would be the same as intrinsic clearance.
Low extraction drugs
On the opposite end of the scale (E < 0.3), low extraction drugs are cleared slowly, as the metabolizing enzymes have some difficulty in oxidizing them, perhaps due to stability in the structure, or the low capacity and activity of the metabolizing enzymes. The metabolizing enzymes may also be present only in very low levels. These drugs are considered to be low intrinsic clearance drugs, as the inbuilt ability of the liver to remove them is relatively poor.
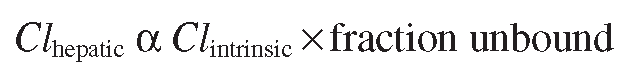
If a low extraction drug is not extensively bound to protein (less than 50 per cent bound) then how much drug is cleared is related directly to the intrinsic clearance of that drug. In the case of a low extraction, strongly protein bound drug, then the liver finds clearance even more difficult, as the affinity of drug for the protein is much greater than the liver’s affinity for the drug. The anticonvulsants phenytoin and valproate are both highly protein bound (~90 per cent) and low extraction drugs and so the amount of these drugs actually cleared by the liver really depends on how much unbound or free drug there is in the blood. This means that:
Therefore, clearance is proportional to the ability of the liver to metabolize the drug (Clintrinsic) as well as the amount of unbound or free drug in the plasma that is actually available for metabolism. Hepatic blood flow changes have little or no effect on low extraction drug plasma levels, but if the intrinsic ability of the liver to clear a low extraction drug falls even further (due to enzyme inhibition or gradual organ failure), there will be a significant increase in plasma and tissue free drug levels and dosage adjustment will be necessary. Conversely, if the intrinsic clearance increases then free drug levels may fall and the therapeutic effects of the agent will be diminished.
It is worth noting, that with drugs of low extraction and high protein binding such as phenytoin and valproate, a reduction in total drug levels due to a fall in protein binding (perhaps due to renal problems or displacement by another, more tightly bound drug) will actually have no sustained effect on free drug plasma and tissue levels, as the ‘extra’ free drug will just be cleared or enter the tissues and the bound/unbound drug ratio will quickly re-assert itself. Since the free drug is pharmacologically active and potentially toxic whilst the bound drug is not, it is not usually necessary to increase the dose in these circumstances. The concentration of the free drug has the greatest bearing on dosage adjustment considerations and laboratory assay systems are now routinely used to determine free drug levels with highly bound, low extraction drugs which are therapeutically monitored, such as with phenytoin and valproate. Other examples of low extraction drugs include paracetamol, mexiletine, diazepam, naproxen and metronidazole. The term ‘restrictive’ clearance is also used to describe these drugs, as their clearance is effectively restricted by their protein binding.