Introduction
The clinical diagnosis of death is beyond the scope of this article. ‘Death’, as generally understood, is the extinction of personality, accompanied by the loss of vital signs such as heart beat, reflexes and respiration. This is known as ‘somatic death’. Thereafter, cellular death follows over a period of time. The survival of individual organs and cells, appropriately handled, provides the basis for organ transplantation.
So-called suspended animation is mentioned here only briefly. The clinical diagnosis of death may be difficult in the elderly, the myxedematous, those under treatment with phenothiazines or under the influence of sedative and narcotic drugs. Voluntary suspended animation has been described amongst Indian holy men. Edgar Allen Poe gives a suitably gruesome account of Monsieur Valdemar’s demise in his Tales of Mystery and Imagination.
Immediate Changes after Somatic Death
Within minutes of cessation of the heart beat, death, as understood by the laity, is usually obvious. The body becomes flaccid, the muscles lose their tone and the corneal and light reflexes disappear. The globes of the eyes become soft due to falling intraocular pressure. Upon ophthalmoscopic examination, the columns of red cells within the retinal veins break up, so-called ‘trucking’, and gradually tumble over the margins of the fovea centralis. This phenomenon may be observed for several hours after death, provided the cornea is moistened with water or saline to minimize the effects of clouding.
The pupillary muscles respond to mydriatics and to miotics for some hours after death. Abortive attempts were made to use these phenomena as a means of estimating postmortem interval, but proved unreliable. Similarly, voluntary muscles, particularly those of the face and limbs, may respond to electrical stimuli or direct tapping with a reflex hammer during the immediate postmortem period, but these techniques have also proved of little value.
Hypostasis (Postmortem Lividity, Sugillation)
This is one of the earliest signs of death. Blood, under the influence of gravity, begins to settle in the vessels of the dependent parts of the body within an hour or so. It may appear even earlier in the obese and ‘full blooded’. Indeed, it was said to occur before death in certain wasting or dehydrating diseases such as cholera, but this author has no first hand knowledge of the phenomenon.
Pressure of even a mild degree prevents hypostasis developing. Thus a person dying on the back shows areas of pale ‘contact flattening’over the shoulder blades, elbows, buttocks, thighs and calves. Hypo- stasis becomes fully developed within about 6 h and ‘fixed’within a few hours thereafter. Thus, if a body is moved for innocent or malign reasons, the primary as opposed to secondary hypostasis, which is often paler in color, will remain and will reveal that such interference has occurred.
Hypostasis normally has a cyanotic or violaceous hue. Vanezis and his coworkers have attempted to use electrocolorimetric methods to determine the intensity of color and thus assess postmortem interval. This, like other attempts to determine postmortem interval, has proved unreliable.
In a naked body exposed to air, transcutaneous oxygenation may impart a pinker hue. This is also well seen in bodies exposed to cold, be it hypothermia or deliberate refrigeration. The marked ‘pinking’may lead to a mistaken diagnosis of death by carbon monoxide or cyanide poisoning. Certain poisons which cause methemoglobinemia, for example sodium chlorate, nitrates or aniline derivatives, can produce a color ranging from slate gray to dark chocolate brown.
After about 12 h hypostasis is very firmly fixed (Fig. 1), but may be cleared by firm massage of the affected part of the skin with a moist sponge. Underlying bruises may then be revealed. If doubt persists as to the authenticity of a purple mark, it should be incised. In a genuine bruise the blood lies free within the subcutaneous muscle and fat. The microscopic examination of tissue from a suspect area should remove any remaining doubt.
In postural asphyxia or in cases where death has occurred with the deceased’s head in a dependent position (for example an intoxicated person who has fallen half out of bed), the hypostasis may be so intense that capillaries may rupture, producing petechial type hemorrhages of varying size. However, these usually extend down below the root of the neck and on to the chest in an ‘open neck shirt’ distribution, so the distinction from throttling or ligature strangulation is usually easy. Hemorrhagic spots may also be seen in the legs of those victims of hanging who have been left suspended for several hours.
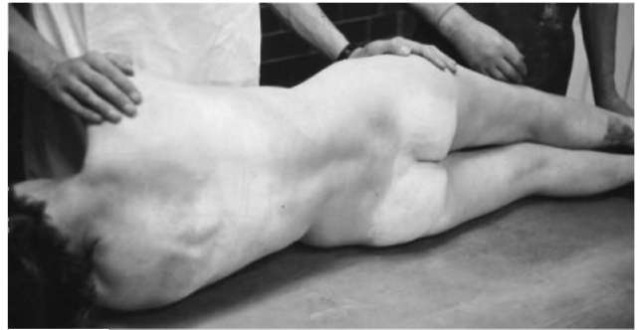
Figure 1 Hypostasis in a body that has been lying on the back for 12 h.
Rigor Mortis
The flaccidity which immediately succeeds death is soon followed by the onset of progressive stiffening of the muscles. In general terms, it appears first in the small muscles of the face (hence the need to close the eyes and bind the jaw of the newly dead as part of last offices). Larger muscle groups are then affected progressively, and rigor is usually complete in 4-6 h. It may become so intense that considerable force needs to be applied to break it down and compose the body in the anatomical position. Indeed, fractures of the neck of the femur and the upper humerus may be produced by such clumsy endeavors. Similarly, postmortem fractures of the cervical spine are not uncommon. Rigor usually begins to pass off in about 18 h, and the body returns to its flaccid state in 36 h or so. The process occurs in reverse order, and residual stiffness of the fingers and eyelids often persists for the longest period of time.
In the past, great emphasis was placed upon the value of rigor in assessment of postmortem interval. This has resulted in miscarriages of justice. It cannot be too strongly emphasized that numerous factors, both intrinsic and extraneous, affect the development of rigor. Extremes of heat and cold both produce rapid stiffening, but in hot conditions it passes off quickly due to the effect of putrefaction. On the other hand, stiffening persists until such time as the body is brought into a temperate environment; it then passes off quickly.
Those who die with a raised body temperature, be it due to illness or violent exertion, may show a rapid onset and loss of rigor. Conversely, those who die of inanition, wasting disease and cachexia develop only weak and transient rigor, the onset of which may be delayed for 12 h or more.
The biochemistry of rigor mortis is still not fully understood. Its onset is accelerated by fatigue and high lactic acid levels in muscle. Muscle proteins include myosin and actin, which form a contractile compound, actomyosin, under the influence of the enzyme adenosine triphosphate (ATP). After death ATP is progressively destroyed, and the actomyosin forms a firm gel until, under the influence of putrefaction, protein disintegration and progressive loss of rigor begins.
Instantaneous rigor (cadaveric spasm)
This is rare. This author has encountered a bare handful of cases. It is usually associated with violent death, for example suicide by handgun or cut throat,and may be localized, with the weapon so firmly gripped in the hand that its removal is difficult. Even more rarely, it may be generalized, with the whole body fixed in the position in which death occurred. For example, a suicidal cut-throat victim may be found sitting bolt upright on a stool with the razor blade clutched between finger and thumb (Fig. 2). Perpetrators of homicide sometimes attempt to simulate suicide by placing the weapon in the victim’s hand and closing the fingers around it. Under those circumstances, the rigor is more readily broken down, and the distinction is easily made. Furthermore, the weapon is often incorrectly positioned, making the stratagem even more obvious.
Late Postmortem Changes
Putrefaction (Fig. 3) is the final and incontrovertible sign of death. The speed of its onset and its varying pathways are greatly affected by the environment. This description is therefore restricted to events as they usually occur in temperate conditions (i.e. 20-40°C). In cold conditions putrefaction may be delayed, but not completely averted. At high temperatures, even only relatively slightly above 40°C, it may be rapid indeed.
Putrefaction is the consequence of bacterial and enzyme activity. Fungi and the depredations of insects and animals also have their part to play. The most dominant factor in the development of putrefaction is the spread of bacteria from the intestine. Thus the earliest sign of putrefaction is greenish discoloration in the right lower quadrant of the abdomen overlying the cecum. This discoloration, due to the breakdown of blood to methemoglobin and sulfhemoglobin, rapidly spreads to involve the whole of the abdomen and chest. Within 4-7 days the surface veins of the limbs also become prominent and discolored (marbling) and the trunk (and external genitalia in the male) begin to swell. The rise in intrathoracic and intraab-dominal pressures results in the expulsion of fluid from the nose and the mouth. These discharges are known to funeral directors as ‘lung purges’and ‘stomach purges’, respectively. Feces may also be expelled from the anus. The fluid at the nose and mouth is often so heavily blood-stained that some form of assault might be thought to have taken place. By this time, the body has a foul odor due to the production of compounds such as indole and skatole.

Figure 2 Suicide: cadaveric spasm.

Figure 3 Putrefaction: death in a centrally heated flat 4 days previously.
In the next stage the gas formation extends to the head and limbs. The skin acquires a crepitant ‘bubbly’ texture, and blisters filled with pinkish fluid appear. These may be readily distinguished from antemortem burns and scalds by the lack of pink ‘vital reaction’at their margin. The superficial layers of skin begin to peel away even upon the lightest touch (so-called ‘skin slip’). Body fluids soak into the surrounding bedding, floor coverings, etc. – or even into the room below.
The onset and progress of putrefaction are hastened by pyrexia of whatever cause, infection and by any perforation of the gut. It is said that poisoning by arsenic or cyanide delays the onset of putrefaction. Certainly the only case of homicidal arsenic poisoning seen by this author was remarkably well preserved upon exhumation several weeks after death and the initial autopsy.
The internal organs putrefy at different rates. The brain rapidly liquefies. The liver first becomes foamy owing to the production of gas, then semiliquid. The spleen liquefies within a matter of hours. The pancreas and kidneys show early microscopic change, even though their general configuration is preserved. The heart and lungs may remain recognizable and often examinable by the naked eye for weeks or even months after death. The nongravid uterus and the prostate gland may still be identified in remains that are otherwise skeletonized.
Adipocere and Mummification
Traditionally these processes, in which putrefaction is arrested due to changes in skin and fat, are described separately, but they can occur together in different parts of the same body given the appropriate conditions.
Adipocere is a spontaneous form of partial preservation by the hydrolysis or saponification of body fat. It is therefore more commonly seen and is more prominent in women and in young, well-nourished children. The hydrolysed fat is at first yellowish-brown in color and of firm consistency; as time passes, it becomes white and friable. It has an offensive, pervasive and persistent odor. When ignited, it burns with a smoky yellow lambent flame.
Its formation is dependent upon the presence of adequate moisture (for example, immersion in water or burial in a bog) (Fig. 4). Acidity is also an important factor. Bodies buried in peat bogs, which are highly acid, or interred in coffins with oak shavings rich in tannin, may be preserved for hundreds, or even thousands, of years.
Mummification is uncommon in temperate climates. The drying out and hardening of the tissues associated with this condition require temperatures far higher than those normally achieved. This author has seen mummified fetuses (and adults) recovered from lofts in the days before fibreglass roofing insulation became commonplace, and has also encountered one case where a burglar became trapped within the ventilation duct of a large office block, and was discovered 7 years later (Fig. 5).
The skin becomes dry, brittle and shrunken. It is usually of dark brown colour. The tips of the fingers and toes may be lost. The hair, irrespective of its colour in life, is usually foxy red. The internal organs are also dry and shrunken, but may be sufficiently well preserved for a naked eye diagnosis to be made. Microscopy is unrewarding, both in mummified and adipocerous bodies.

Figure 4 Adipocere in a body immersed in fresh water for over a year.

Figure 5 Mummification: trapped in a heating duct for 7 years.
Postmortem Entomology and Other Artifacts
The common bluebottle or blowfly lays its eggs when the skin temperature falls below 27°C. The eggs rapidly hatch into maggots, which have a voracious appetite and invade all parts of the body, including the cranium, thorax and abdomen. Beetles lay their eggs on older bodies. Bodies immersed in water are not immune to insect activity. Caddis flies, water beetles, etc., in common with all insects, will ‘nibble’ at exposed surfaces, producing areas of apparent abrasion.
Animals such as rats and mice attack exposed parts of bodies. Foxes will also eat carrion. Even domestic dogs and cats will turn to their owners once the contents of the biscuit bowl have been exhausted. Fungi attack the skin even in embalmed and/or refrigerated bodies. When wiped away, the underlying exposed areas of skin are often discolored and roughened; these changes may lead to the mistaken diagnosis of bruises or abrasions sustained during life. Occasionally, a clumsily handled body may be damaged while being lifted into the coffin or wheeled through the corridors of a mortuary, producing abrasions upon the skin, usually over bony prominences. These abrasions are readily distinguished from ante-mortem injury. They are light brown in colour and rapidly become hard, shiny and slightly depressed. There is no vital reaction around them, and they show no microscopic changes of injury.
