Introduction
The term ‘blunt trauma’ can be defined as damage to the body due to mechanical force applied either by the impact of a moving blunt object or by movement of the body against a hard surface, both mechanisms resulting in the transfer of kinetic energy high enough to produce an injury (mainly by compression, traction, torsion and shear stresses). Blunt force injuries occur in criminal assaults (e.g. blow with a blunt-edged instrument, punch, kick), in physical child abuse, in traffic and industrial accidents, in suicides (jump from a height) and in accidental falls brought about by the victim himself.
Blunt Injuries to the Integument
Abrasions
Abrasions are superficial injuries to the skin characterized by a traumatic removal, detachment or destruction of the epidermis, mostly caused by friction. In so-called tangential or brush abrasions a lateral rubbing action scrapes off the superficial layers of the skin (for example from the body’s sliding across a rough surface) and leaves a denuded corium which is initially covered with serosanguineous fluid. In fresh grazes the direction of impact can often be determined by abraded epidermal shreds which remain attached to the end of the scrape. At a later time the tissue fluid dries out and forms a brownish scab. If the lesion does not reach the dermis, it heals within several days without scarring. Infliction just before or after death results in a leathery (‘parchmentlike’) appearance with yellowish-brown discoloration (Fig. 1).
Another type of abrasion is caused by a vertical impact to the skin (so-called pressure or crushing abrasion). In such cases the injuring object may be reflected by the shape of the skin injury, so that the patterned abrasion can be regarded as an imprint of the causative object.
Contusions
Contusions or bruises are extravasations of blood within the soft tissues originating from ruptured vessels as a result of blunt trauma. In this context,only the contusions that are visible externally are considered. Text topics usually differentiate between intradermal and subcutaneous bruises. In the first-mentioned category the hemorrhage is located directly under the epidermis, i.e. in the corium. This kind of superficial hematoma is usually sharply defined and red, whereas the more common bruises of the deeper subcutaneous layer have blurred edges and, at least initially, a bluish-purple color (Fig. 2).

Figure 1 Tangential abrasion confined to the upper layers of the skin. The shreds of epidermis indicate the direction of impact. The central parts of the nuded corium show a parchmentlike discoloration from drying.
Intradermal bruises may reflect the surface configuration of the impacting object (Fig. 2). The skin which is squeezed into grooves will show intradermal bleeding, whereas the areas exposed to the elevated parts remain pale. Especially in falls from a height, the texture of the clothing may produce a pattern of intradermal bruises corresponding to the weaving structure. Patterned extravasations of this type are also seen in tire tread marks, if an individual is run over by a wheel, and in bruises from vertical stamping with ribbed soles.

Figure 2 Patterned contusions from kicking to the thigh (partly in combination with curved abrasions corresponding to the front part of the perpetrator’s shoe).
Subcutaneous bruises are usually nonpatterned. Nevertheless there may be bruising of special significance. If the body is struck by a stick, a broom-handle, a pool cue, a rod or another elongated instrument, every blow leaves a double ‘tramline’ bruise consisting of two parallel linear hematomas with an undamaged zone in between. Victims of blunt force violence often sustain contusions from self-defense, typically located on the ulnar aspects of the forearms and on the back of the hands. The upper arms may show groups of roundish bruises from fingertip pressure in cases of vigorous gripping. A periorbital hematoma (‘black eye’) is either induced by direct impact (e.g. punch or kick) or indirectly (due to seepage of blood from a fractured orbital roof, a fractured nasal bone or from a neighboring scalp injury of the forehead).
In general bruises are regarded as a sign of vitality indicating that the contusion was inflicted prior to death. During life the blood from ruptured vessels is forced into the soft tissue by active extravasation. Nevertheless, to a limited extent postmortem formation of contusions is possible due to passive ooze of blood. In surviving victims, a deep bruise may not become apparent on the skin until several hours or even days later because of the slow percolation of free blood from the original site to superficial tissue layers.
In a living person the contusion undergoes a temporal series of color changes. Initially most subcutaneous bruises appear purple-blue. As the hematoma resolves during the healing process, the hemoglobin released from the red blood cells is chemically degraded into other pigments such as hemosiderin, biliverdin and bilirubin. The color changes – usually in the course of several days – to green and yellow before it finally disappears. However, the rate of change is quite variable and depends on numerous factors, above all the extent of the bruise.
The size of an intradermal or subcutaneous hematoma is not always indicative of the intensity of the force applied to the affected area. Elderly people or patients suffering from bleeding diathesis may get bruises from slight knocks or for other minor reasons. On the other hand, absence of an externally visible injury does not necessarily mean that there was no relevant trauma. Subcutaneous bruises of surviving victims are often followed by gravity shifting of the hemorrhage leading to a secondary downward movement of the hematoma.
A special type of blunt injury to the soft tissues is frequently seen in pedestrians who have been struck or run over by motor vehicles. Both the skin and the subcutaneous layer may be avulsed from the underlying fascia or bones by shearing forces so that a blood-filled pocket is formed, typically in combination with crush damage to the adjoining fatty tissue.
Lacerations
Lacerations are tears of the skin or of internal organs (see below). They may be caused by blows from blunt objects (such as a hammer, a whipped pistol, a rod, a toe-cap of heavy footwear or a fist); other lacerations are produced by impact from vehicles or by a fall to the ground. Lacerations occur most commonly in body regions where the integument directly overlies a firm bony base acting as support (scalp, face, back of the hand, shins). When the force acts on the skin, the subcutaneous tissue is squeezed between the injuring object and the bony platform so that the integument is compressed and crushed until it tears and splits sideways (Figs 3 and 4).
Lacerations are characterized by abraded, bruised and crushed wound margins. The edges of the tears are typically irregular and ragged with bridging tissue strands (vessels, nerves and fibers) running from side to side. The wound slits may be linear (especially in blows with a narrow, edged instrument), Y-shaped or star-like. If the impacting object hits the skin at an oblique angle, one of the edges will be ripped away resulting in unilateral undermining (undercutting, avulsion) which indicates the direction of the force. Sometimes foreign material from the causative instrument/surface is deposited in the depth of the wound slit. The abrasion surrounding the tear may correspond to the shape and dimensions of the impacting blunt-surfaced instrument (Fig. 4) or – in case of a fall to the ground – the area of contact.
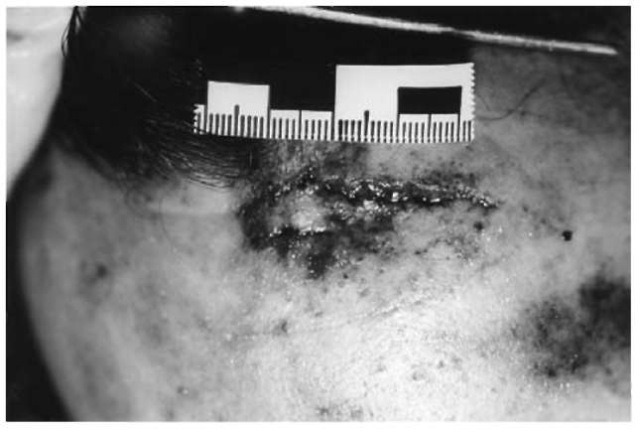
Figure 3 Laceration to the forehead. Note the irregular wound slit with abraded and contused margins.

Figure 4 Parietal region of a man whose scalphas been shaved before autopsy, showing two stellate lacerations from hammer blows to the head. The abrasion which belongs to the upper injury approximately reproduces the shape of the rectangular hammer face.
Head Injuries
The head is a common target in assaults with blunt objects; other frequent causes of head injuries are traffic accidents, falls from a height and falls from a standing position. The area of impact usually reveals injuries of the scalp or the facial skin, but it has to be stressed that severe and even lethal trauma-tization is not necessarily associated with scalp bruising, marked swelling, excoriation and/or laceration. There may be no externally visible signs, especially in skin areas covered with hair and in cases of a fall onto a flat surface. An impact site on the vertex suggests that the head sustained a blow whereas in falls from standing positions the scalp injuries are expected at the level of the brim of the hat.
Skull fractures
These may involve the cranial vault, the base of the skull and the facial skeleton. Though the presence of a skull fracture indicates severe traumatization, the fracture itself rarely threatens the victim’s life. There are several types of skull fractures to be distinguished.
Single or multiple linear fractures are caused either by a blow with an object with a broad flat surface area or by a fall on the head so that the skull is deformed (flattening/indenting at the point of impact and outward bending/bulging in the periphery). The fracture lines originate where the bone is bent outwards and therefore is exposed to traction forces exceeding the limits of the bone’s elasticity; from these extruded parts of the skull the fractures extend towards the area of impact, but also in the opposite direction. For this reason, either of the ends is often in congruity with the impact injury of the scalp. Several fracture lines may radiate outward from a central point of impact (Fig. 5) where the skull is often depressed and/or shattered to pieces forming a spider’s web or mosaic pattern consisting of circular and radiating linear fractures. The sequence of skull injuries may be determined according to Puppe’s rule: a later fracture does not cross a pre-existing fracture line but terminates when reaching an earlier one.
Before fusion of the cranial sutures (i.e. in children and young adults), a fracture may travel along the seam resulting in diastasis (diastatic fractures). If a gaping fracture runs from one side of the cranial base to the other (mostly after lateral impact or side-to-side compression), this transverse type is called a hinge fracture (Fig. 6) because of the independent movement of the front and rear halves of the skull base.
Longitudinal fractures of the base of the skull frequently occur due to a fall on the occiput; in such instances the linear fractures typically run through the posterior fossa either ending near the foramen magnum (Fig. 7) or extending to the floor of the middle and anterior fossa. On the other hand, longitudinal fractures of the base can also be produced by impaction of the frontal region.
Depending on its course and location, a base fracture may be followed by several clinical signs: bleeding from the ear (in fractures of the temporal bone with concomitant hematotympanon and rupture of the eardrum); bleeding from the nose and mouth (in fractures involving paranasal sinuses which provide a communication with the nasopharynx); periorbital hematoma (from fractures of the orbital roofs); leakage of cerebrospinal fluid coming out of the nose or the ear (if the dura is injured along the fracture); bacterial infection of the meninges (by spread from the nasal cavity, the paranasal sinuses and the middle ear, especially when the fracture is accompanied by a tear of the dura).
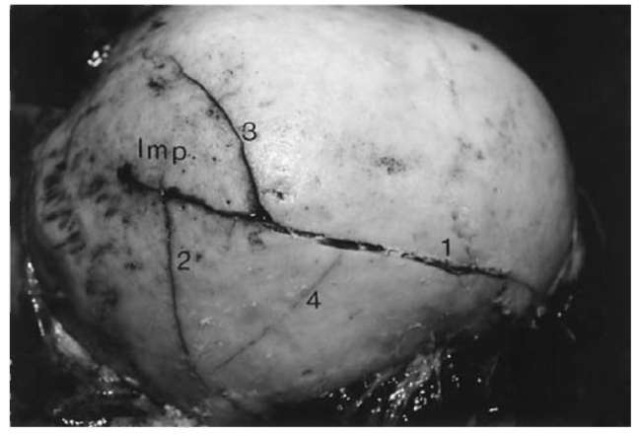
Figure 5 Right half of a cranial vault with two fractures (1, 2) radiating outward from the area of impact (Imp.) and in addition two incomplete circular fractures (3, 4).
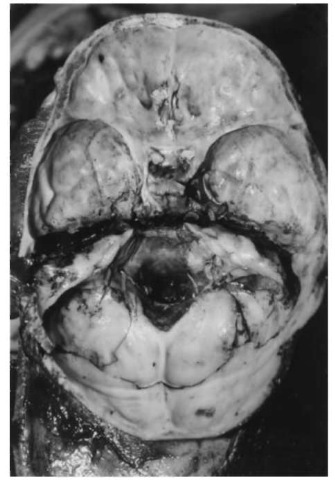
Figure 6 Transverse (side-to-side) ‘hinge fracture’ dividing the base of the skull into a front and rear half.
Some special types of skull fractures can only be mentioned briefly. A ring fracture is located in the posterior fossa and encircles the foramen magnum. It mostly occurs in a fall from a height onto the victim’s feet or buttocks so that the cervical spine is driven into the skull.
Bone impressions and depressed fractures are always localized at the point of impact where the head is struck with an object having a relatively small surface area such as a hammer or a protruding corner of a piece of furniture (Fig. 8). The outline of a clean-cut defect in the outer table may reproduce the shape and size of a sharp-edged instrument. If only limited force is applied, the depressed fracture can be restricted either to the outer or, less often, to the inner table of the skull (the latter with inward displacement of the bone fragments). A depressed fracture from a blow which struck the skull cap at an angle may be concentrically terraced. Hole fractures from bullets perforating a flat bone of the skull are mostly roundish and clean-cut at the site of entrance, but beveled out in a crater-like manner at the exit site.

Figure 7 (A) Base of the skull with linear fracture (arrow) in the posterior fossa extending downwards into the foramen magnum, sustained in a fall on the occiput. Note the presence of secondary fractures in the anterior fossa floor. (B) Close-upview of the fractured left orbital roof with dark coloration from underlying blood.
Blunt force applied to the occiput, mostly as a consequence of a fall on the back of the head, frequently causes independent fractures of the anterior cranial fossa such as cracks of the thin orbital roofs (secondary fractures at the site of the contrecoup).
Intracranial hemorrhages
A space-occupying bleeding into the brain membranes is followed by local displacement of the brain and raised intracranial pressure with concomitant flattening of the cerebral hemispheres.
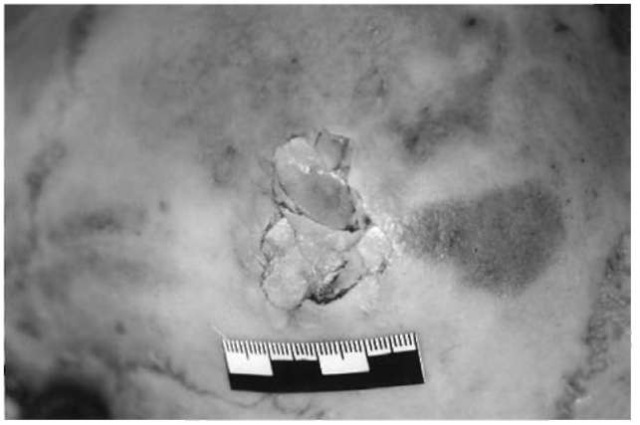
Figure 8 A depressed fracture of the skull cap from a blow with a heavy monkey-wrench.
Intracranial hematomas as well as traumatic brain swelling, which often accompanies head injuries, may result in transtentorial (uncal) herniation (in cases of supratentorial mass lesion) and/or herniation of the cerebellar tonsils which are forced into the foramen magnum leading to compression of the brainstem with secondary damage and failure of the medullary respiratory centers.
From the clinical and forensic point of view, the possible occurrence of a so-called ‘lucid’ or ‘latent’ interval has to be mentioned. After initial unconsciousness (due to cerebral concussion) there may be a symptomless period of several hours or even days before the victim becomes comatous again because of the increased hemorrhage and the consequently raised intracranial pressure.
Epidural (extradural) hemorrhages are located between the skull and the underlying dura mater which is stripped from the bone by bleeding from a torn vessel (Fig. 9). Epidural hematomas have a typical disc- or lens-shaped appearance. The most common site is the temporal and the adjacent parietal region where the branches of the middle meningeal artery are easily lacerated in the course of a transecting fracture line. Since the well-adherent dura has to be avulsed from the bone, epidural hematomas more frequently originate from arterial bleeding than from venous bleeding (e.g. due to a torn dural sinus). In the great majority an extradural hemorrhage is associated with a cranial fracture.

Figure 9 Extradural (epidural) hemorrhage in the parieto-temporal area. The hematoma (arrow) is located between the inner surface of the skull and the detached dura.
Subdural hematomas are intracranial bleedings located beneath the dura mater and above the arachnoid (Fig. 10). Most often the hemorrhage arises from the tearing of overstretched bridging veins that traverse the subdural space between the surface of the cerebral hemispheres and the superior sagittal sinus. Other possible sources of subdural bleeding are injuries to venous sinuses or to the cerebral parenchyma (such as cerebral contusions with concomitant laceration of the arachnoid). The subdural hemorrhage usually covers one cerebral hemisphere in a cap-like manner from the parasagittal area via the lateral surface down to the basal fossas; on a horizontal section it appears as a sickle-shaped accumulation of blood. In contrast to epidural hematomas, subdural hemorrhages are often not associated with skull fractures; additional damage to the brain tissue may also be absent. A high percentage of subdural bleedings are caused by acceleration or deceleration of the head, for instance in falls when the head impacts a hard surface, but also in traffic accidents and physical child abuse (battered child and shaken baby syndrome). Apart from acute and subacute subdural hemorrhages there are prolonged cases of hematoma formation and organization, mainly in elderly people and sometimes without a history of previous traumatization. Such chronic subdural hematomas typically consist of brown and gelatinous blood accumulations adherent to the meninges and sometimes covered with a tough membrane.
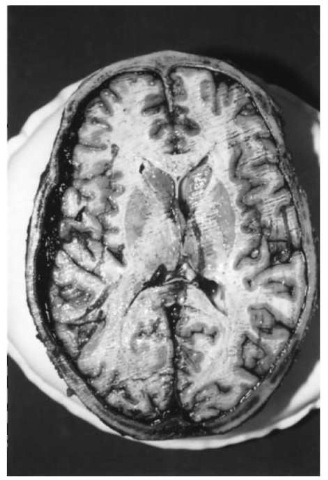
Figure 10 Acute subdural hemorrhage. The unilateral space-occupying lesion has slightly shifted the midline of the brain to the opposite side.
Traumatic subarachnoid bleeding may result from damage to the cortex such as brain contusion (e.g. contrecoup lesions), from penetrating injuries to the brain and as a consequence of vessel tears within the subarachnoid space. An extensive hemorrhage on the ventral surface and around the brainstem may arise from a laceration of an artery belonging to the circle of Willis or from another great vessel (such as a torn basilar and vertebral artery).
Cerebral injuries
‘Concussion of the brain’ is a clinical diagnosis which means a disorder of cerebral function following immediately upon a (blunt) head injury. It is usually characterized by a transient loss of consciousness (initial coma) with subsequent amnesia from the actual moment of trauma; it is often combined with retrograde amnesia and vegetative signs such as nausea and vomiting. In mere concussions the unconsciousness lasts only for a relatively short time (less than 1 h) and the brain tissue does not show any evidence of structural damage. Nevertheless even a simple cerebral concussion may be followed by the victim’s death, if the head trauma is joined by interfering mechanisms (for instance drowning or aspiration of gastric contents during unconsciousness).
Cerebral contusions are traumatic lesions of the brain frequently seen in the cortex and sometimes extending into the underlying white matter (Fig. 11). Fresh contusion hemorrhages are mostly located on the crests of the gyri and composed of grouped streak-like or punctate blood extravasations. The cortical lesions are often covered with subarachnoid bleeding. In contrast to cerebral contusions, the term ‘laceration’ means a major destruction of the anatomical context (for instance mechanical separation of the tissue due to bone fragments or penetrating bullets). In case of survival, the contusion hemorrhages are reabsorbed and assume a yellowish-brown appearance with softening and finally liquefaction of the affected areas.
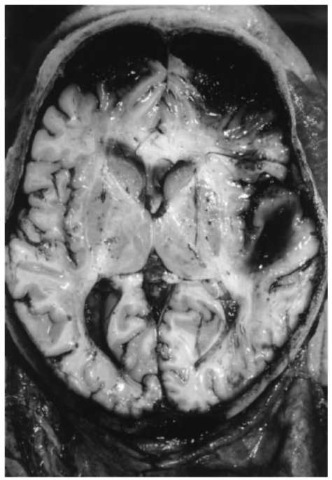
Figure 11 Contrecoup contusions of the frontal poles opposite to the point of impact (fall on the back of the head) with concomitant subarachnoid hematoma; traumatic intracerebral (sub-cortical) hematoma in the white matter of the right temporal lobe (in close vicinity to cerebral contusions in the overlying cortex).
Due to the injuring mechanism, most cerebral contusions occur in brain regions that are directly opposite to the point of impact. This contrecoup type of contusion is classically caused by a fall on the occiput, when the moving head is suddenly decelerated with the consequence that the inlying brain is damaged due to inertia. In falls on the back of the head, the contrecoup areas of the brain (poles and undersurfaces of the frontal and temporal lobes) are subjected to an ultrashort negative pressure (‘cavita-tion’) resulting in vessel ruptures and cortical hemorrhages (Figs 12 and 13). On the other hand, the so-called coup contusions arise at the area of impact due to the local deformation and compression of the brain. Even severe coup and contrecoup injuries are not necessarily associated with skull fractures. In victims with both coup and contrecoup lesions, the degree of contrecoup damage is usually more marked. Fracture contusions are localized in topographical correspondence to fracture lines and/or depressed fractures.

Figure 12 Contrecoupcontusions on the undersurface of the frontal lobes (mostly located at the crests of the convolutions) with slight subarachnoid hemorrhage.
Diffuse axonal injury (DAI) is considered a consequence of shear and tensile strains from sudden acceleration/deceleration or rotational movements of the head. Overstretching of the nerve fibers in the white matter leads to axonal injury varying from temporary dysfunction to anatomical transection, the latter being followed by microscopically visible club-shaped retraction-balls on the axons. The sites of predilection include the corpus callosum, the par-asagittal white matter, the superior peduncles and the upper brainstem. In the course of the repair process, microglial cells proliferate in the areas of axon damage. In victims of substantial head injuries, especially after traffic accidents, diffuse axonal injury may be responsible for prolonged coma and a fatal outcome even in the absence of an intracranial mass lesion.
Cerebral edema is a frequent finding in significant head injuries. The formation of edema is due to an increase in the fluid content of the brain, predominantly in the white matter. Post-traumatic edema may be generalized (diffuse) or related to focal tissue damage (e.g. adjacent to an area of cerebral contusion or laceration). At autopsy the weight of the brain is increased, the gyri are pale and flattened with shallow sulci in between. From the pathogenetic point of view, edema is attributed to a heightened vascular permeability which in turn may be worsened by additional hypoxia.

Figure 13 Close-upview of the frontal lobes with characteristic streak-like, densely arranged contusion hemorrhages in the cortex.
As with space-occupying lesions such as subdural or epidural hematomas, cerebral edema is a common cause of raised intracranial pressure. The enlarged volume of the edematous brain results in a displacement of cerebral tissue downwards through the mid-brain opening resulting in grooving of the unci and/or hippocampal herniation. Expansion of the subtentor-ial brain leads to herniation of the cerebellar tonsils which are forced into the foramen magnum. Hernia-tion with concomitant compression of the brainstem may be followed by secondary hemorrhages (localized in the midbrain and pons) and finally by lethal dysfunction of the vital centers.
Injuries of the Chest
Nonpenetrating blunt force may damage the thoracic wall and/or the chest organs. Rib fractures are caused either by direct or by indirect violence. In the first case a localized force is applied and the underlying ribs are broken in the contact area; the other (indirect) type of rib fracture occurs away from the impact, mainly due to compression of the chest.
Rib fractures are frequently associated with complications that may be dangerous or even life-threatening.
• If a victim sustains numerous fractures, the rib cage loses its rigidity so that the injured section of the chest wall will not participate in the expansion of the thorax during inspiration with the result of paradoxical respiration (flail chest) and concomitant hypoxia.
• Sharp, pointed ends of the rib fragments may penetrate the pleura and lacerate the lung and/or the intercostal blood vessels with consecutive bleeding into the chest cavity (hemothorax).
• A leak in the visceral pleura permits air to enter the pleural cavity (pneumothorax) so that the lung collapses, if it is not fixed to the chest wall by pre-existing pleural adhesions. A valve-like leakage in the pleura leads to a so-called tension-pneumo-thorax caused by an increasing pressure of trapped air in the pleural cavity and followed by a complete collapse of the affected lung and a shift of the mediastinum to the opposite side.
• The presence of air bubbles in the subcutis or in the mediastinum (subcutaneous/mediastinal emphysema) may derive from injuries of the trachea, the bronchi, the thoracic wall or the lungs by air entering the adjacent soft tissues.
Blunt-force injuries to the lung are mainly encountered as contusions or lacerations. A contusion is typically caused by a substantial impact on the chest with consecutive inward bending of the thoracic cage. In young victims contusions are not necessarily accompanied by fractures of the ribs or of the sternum because of the high pliability of the juvenile thoracic cage. From the morphological point of view, a contused lung shows bruising either as a subpleural suffusion or as an intrapulmonary hemorrhage. Lacerations of the lung can result when a severe compressive or crushing force is applied to the chest so that the pulmonary tissue bursts or tears. Another possible mechanism is inward displacement of a fractured rib which impales the lung.
Blunt traumatization of the heart manifests itself as concussion, contusion or myocardial rupture. In most cases the force is directly applied to the anterior chest, which compresses or crushes the heart between the sternum and the vertebral column. Bruises of the cardiac wall may be localized in the subepicardial fatty tissue (sometimes in combination with post-traumatic coronary occlusion) or within the myocardium which then appears dark red from interstitial hemorrhage. Lacerations of the heart are most often seen in the relatively thin right ventricle or in the atria; they are less common in the left ventricle, the papillary muscles, the cardiac valves, the interatrial and the interventricular septum. The risk of cardiac rupture is especially high during diastole when the heart chambers are filled with blood and therefore easily burst when they are exposed to a sudden compressive force. Such injuries usually have a fatal outcome either from massive blood loss and hemorrhagic shock (if the pericardial sac is torn and the blood pours into a pleural cavity) or from cardiac tamponade (blood accumulation in the pericardial sac resulting in insufficient filling of the cardiac chambers and impaired forward circulation).
Traumatic aortic ruptures typically occur in vehicular accidents and in falls from a height. The most important mechanism is sudden deceleration, possibly in combination with compression and/or shearing. Traction forces tear the aorta transversely at two sites of predisposition: in the descending part of its arcus (near the attachment of the ligamentum arteriosum) (Fig. 14) or immediately above the cusps of the aortic valve. Other locations (for instance in association with a dislocated vertebral fracture) are rather rare. The laceration of the aorta may occur either as a complete or partial transection. In the latter case the outer layers of the vascular wall are not damaged; the intimal tears are often multiple, semicircular and parallel (so-called ladder-rung tears). If the trauma is survived at least for a short time, a parietal thrombosis or a post-traumatic aneurysm may follow as secondary complications.

Figure 14 Transection of the aorta in the distal part of the arch (deceleration injury).
Abdominal injuries
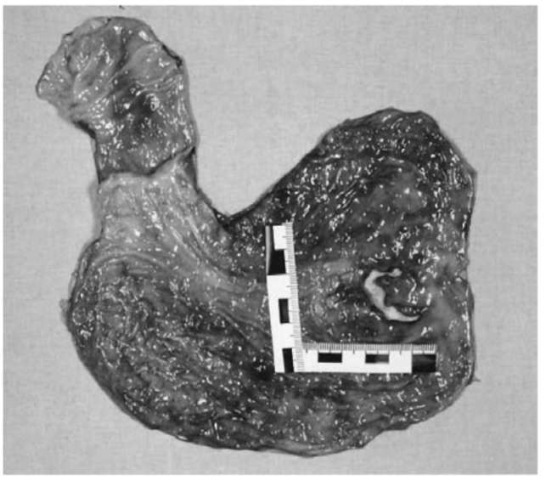
Blunt force injuries of the abdomen are frequently seen in traffic and work accidents, in child and spouse abuse, in other criminal assaults (with kicking, stamping and punching), but also in suicidal falls from heights. The abdominal organs most vulnerable to blunt trauma are the solid liver and spleen on the one side and the mesentery on the other. Concomitant external signs of blunt traumatization such as contusions or abrasions are by no means obligatory. Substantial injuries to the liver, the spleen and the mesentery always have to be regarded as life-threatening and potentially fatal, especially in cases without rapid surgical treatment. The main reason is internal bleeding into the peritoneal cavity from lacerations (Figs 15 and 16). Ruptures of the liver and spleen can be classified as either transcapsular subcapsular laceration. In the first case both capsule and parenchyma are injured so that the blood instantaneously pours into the peritoneal cavity. The second type of laceration is characterized by the initial formation of a subcapsular hematoma which expands continuously and possibly causes a delayed rupture when the covering capsule tears due to overstretching (mostly several hours or even days after the trauma).
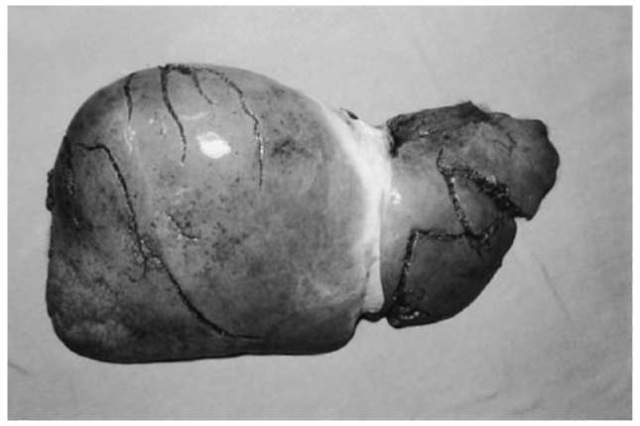
Figure 15 Multiple transcapsular lacerations of the liver.
The stomach and the intestine are less susceptible to blunt traumatization than the parenchymatous abdominal organs. The hollow viscera are more likely to rupture, if they are filled with food or fluid. Another reason why the intestine or stomach might be prone to damage is squeezing of the organs between the indented abdominal wall and the lumbar vertebrae. Fatal outcomes from contusions or lacerations (Fig. 17) of the gastrointestinal tract are usually due to diffuse peritonitis.
Renal injuries are a relatively rare source of severe bleeding since the kidneys are deeply located behind the peritoneum. Nevertheless they can be ruptured by a heavy impact to the loin (for instance in traffic accidents or assaults).

Figure 16 Lacerations of the spleen.
Figure 17 Laceration of the stomach.
Though the empty urinary bladder is placed within the pelvis, when filled it moves upwards and is therefore exposed to blunt traumatization of the lower abdomen. Consequently, rupture of the empty bladder is expected to be extraperitoneal and accompanied with pelvic fractures, whereas a bladder distended with urine may rupture into the peritoneal cavity.
Blunt traumatization of a pregnant uterus is a possible cause of fetal death, mostly due to separation or rupture of the placenta.
Injuries to the Extremities
Apart from injuries to the skin and the subcutaneous layer (see above) other anatomical structures such as the muscles, the bones and the joints may be involved in blunt-force trauma. Extensive crushing of the soft tissues, the formation of blood-filled cavities, comminuted fractures and severence of large vessels are frequent findings in victims of automobile-pedestrian accidents. Internal bleeding (from closed injuries) and external bleeding (from traumatic amputation, severe avulsive wounds and compound fractures) are important factors contributing to hemorrhagic shock. Another sequel to blunt trauma is pulmonary and systemic fat embolism (caused by globules of fat, usually subsequent to fractures or damage of fatty tissues). In cases of prolonged survival, intercurrent infection and pulmonary embolism (originating from post-traumatic venous thrombosis) are dangerous and often fatal complications of an originally non-lethal injury.