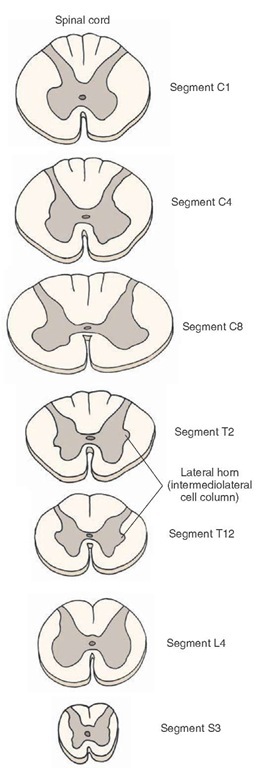
Spinal Segments
The spinal cord consists of 31 segments (8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal) based on the existence of 31 pairs of spinal nerves. Each segment (except the first cervical and coccygeal segments) receives dorsal and ventral root filaments on each side. A schematic representation of different spinal segments is shown in Figure 9-5. The functions of various tracts and neuronal groups located in these segments are described later in this topic in the section, "Spinal Cord Tracts."
Cervical segments are the largest spinal cord segments. In each half of the spinal cord, the dorsal funiculus is divided into two major ascending pathways called the fasciculus gracilis and fasciculus cuneatus.
Thoracic segments are smaller than the cervical segments because they contain a smaller amount of gray and white matter. A lateral horn, which contains the IML (described earlier), is present in all thoracic segments (Fig. 9-5). The IML of the thoracic and lumbar spinal cord contains preganglionic sympathetic neurons. In all thoracic segments, a prominent structure called the dorsal nucleus of Clarke contains large cells and is located medially at the base of the dorsal horn. At rostral levels of the thoracic cord (T1-T6), both the fasciculi gracilis and cuneatus are present, whereas at caudal levels (e.g., T7-T12), only the fasciculus gracilis is present. The spinal nerves emerging from the rostral levels of the thoracic cord (except T1) provide motor innervation to the back and intercostal muscles (axial muscles). The spinal nerves emerging from the caudal thoracic levels innervate abdominal muscles in addition to axial muscles.
FIGURE 9-5 Spinal cord segments. Cervical segments are the largest segments. The thoracic and sacral segments are relatively small. Note the presence of intermediolateral cell column in the thoracic and sacral segments. C = cervical; T = thoracic; L = lumbar; S = sacral.
The lumbar segments appear circular in transverse sections (Fig 9-5). The segments at L1 and L2 are similar to those located at lower thoracic levels. These segments contain the IML. The lumbar segments located at L3 to L5 do not contain IML. These segments provide motor inner-vation to the large muscles in the lower extremities.
The sacral segments are relatively small. They contain relatively small amounts of white matter and more abundant quantities of gray matter. The IML of sacral segments S2-S4 contains the parasympathetic preganglionic neurons.The coccygeal segments resemble the sacral segments.
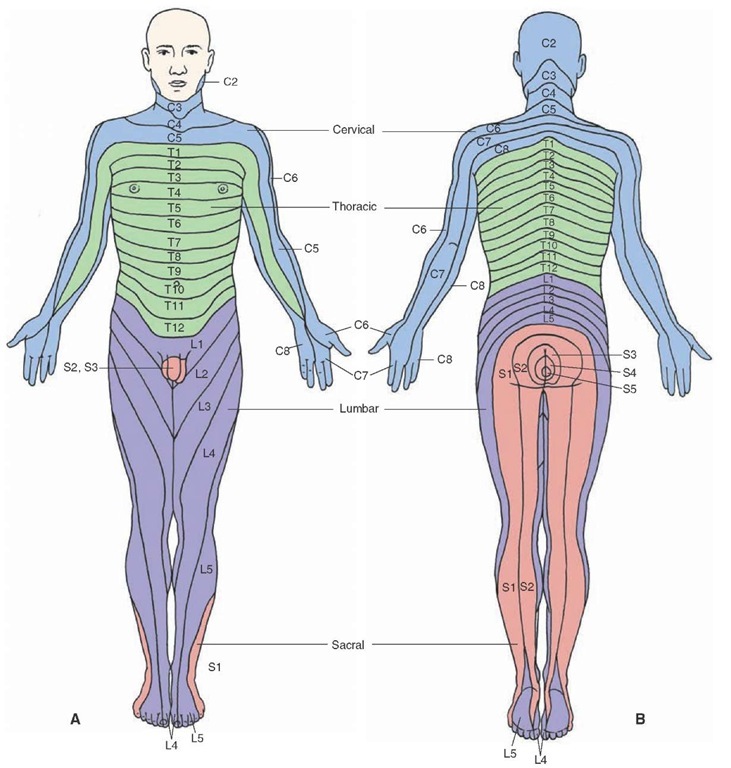
A dermatome is defined as the area of skin supplied by the right and left dorsal roots of a single spinal segment. Dermatomal maps of the peripheral distribution of spinal nerves reveal a set of bands on the surface of the body (Fig. 9-6). If one dorsal root is sectioned, the sensation in the corresponding dermatome is not lost because several adjacent dorsal roots innervate overlapping areas on the skin. Usually three adjacent dorsal roots have to be sectioned in order to lose sensation in one dermatome.
FIGURE 9-6 Dermatomal maps of the peripheral distribution of spinal nerves. (A) Front view. (B) Back view. Labels indicate the innervation of each dermatome. C = cervical; T = thoracic; L = lumbar; S = sacral.
Spinal Cord Tracts
As noted earlier, tracts, or fasciculi, are bundles of fibers that have the same origin, course, and termination. Different tracts are clustered together in the white matter of the spinal cord and are referred to as dorsal, ventral, and lateral funiculi. The dorsal funiculus (dorsal column) contains two ascending tracts, the fasciculus gracilis and fasciculus cuneatus, which are described in the following sections. The lateral aspect of the funiculi contains long ascending and descending tracts, whereas the region adjacent to the gray matter contains the short tracts that connect different spinal segments.
Long Ascending Tracts
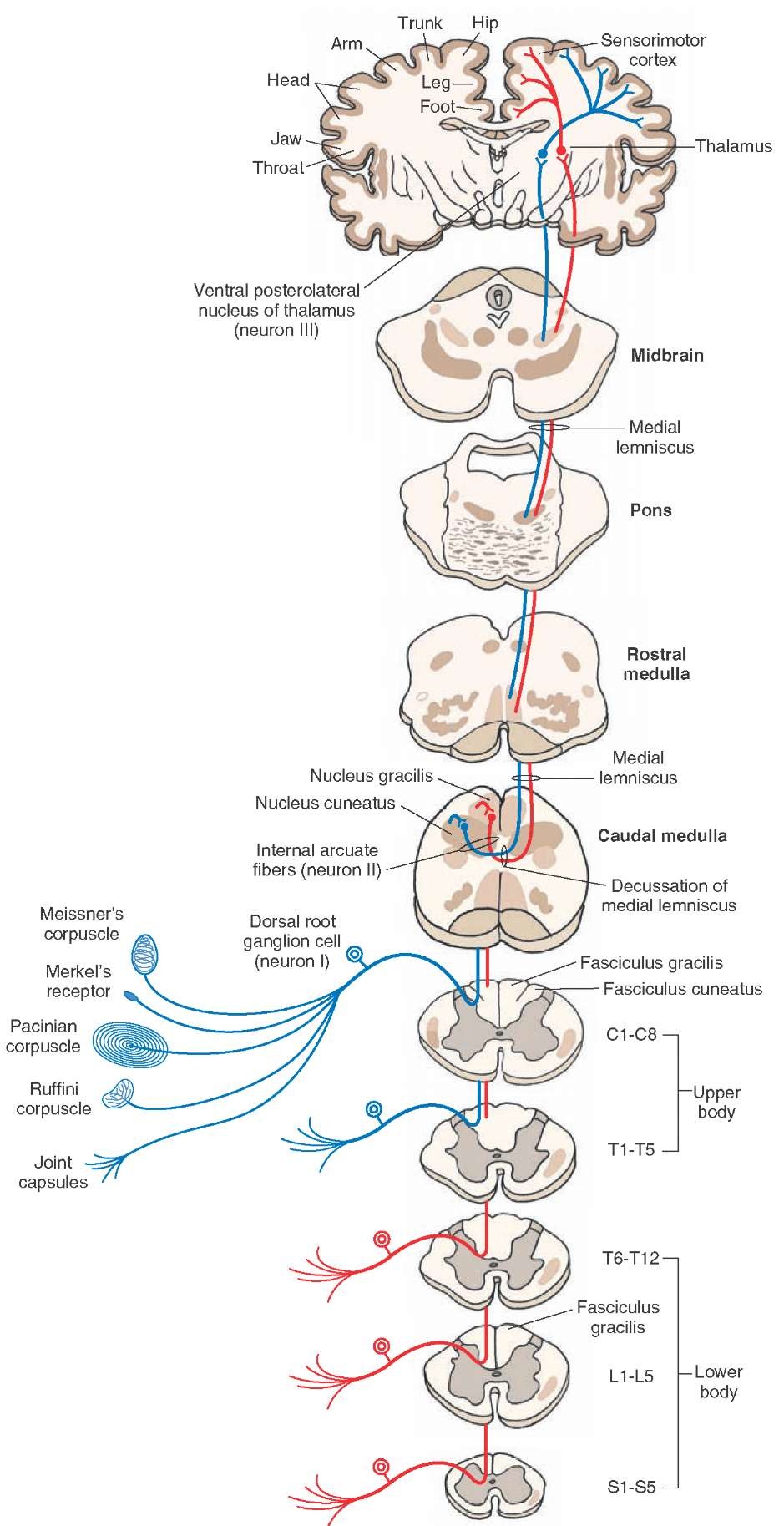
Fasciculus Gracilis
The dorsal (posterior) white column of the spinal cord consists of the fasciculi gracilis and cuneatus (described in the next section). The fasciculus gracilis (containing ascending fibers from the lower body) is located medially, whereas the fasciculus cuneatus (containing ascending fibers from the upper body) is located laterally in the dorsal column. A schematic diagram of the course of fibers in the fasciculus gracilis is shown in Figure 9-7. This tract exists at all levels of the spinal cord and contains afferent fibers from the sacral, lumbar, and thoracic segments T6—T12, which mediate sensations from the lower body.
The neurons located in the dorsal root ganglion represent the first-order neurons (i.e., neuron I). The peripheral processes of the first-order neuron innervate the Pacinian corpuscle (sensing tactile and vibratory stimuli) and Meissner’s corpuscle (sensing touch) in the skin as well as proprioceptors in joints that are involved in kinesthesia (sense of position and movement). The central processes of the first-order neuron ascend ipsilaterally in the spinal cord (i.e., the ascending fibers of first-order neurons are uncrossed) and terminate somatotopically on second-order neurons (i.e., neuron II) in the ipsilateral nucleus gracilis in the medulla. Axons of the second-order neuron in the nucleus gracilis travel ventromedially as internal arcuate fibers and cross in the midline to form the medial lemniscus (decussation of medial lemniscus). This crossed tract ascends through the medulla, pons, and mid-brain and finally terminates on the third-order neurons (i.e., neuron III) located in the contralateral ventral posterolateral nucleus of the thalamus. Axons of the third-order neurons terminate in the medial aspect of the sensorimotor cortex. The fasciculus gracilis is involved in mediating conscious proprioception that includes kinesthesia and discriminative touch.
Fasciculus Cuneatus
A schematic representation of the course of this tract is shown in Figure 9-7. It exists in thoracic segments above T6 and cervical segments and contains long ascending fibers from the upper body. Myelinated afferents from the dorsal root ganglion enter the dorsal funiculus, medial to the dorsal horn, and the ascending fibers occupy a lateral position in the dorsal funiculus. The peripheral processes of the first-order neuron innervate Pacinian and Meissner’s corpuscles in the skin and proprioceptors in joints, and central processes of the first-order neuron ascend ipsilaterally to terminate on second-order neurons located in the ipsilateral nucleus cuneatus of the medulla. As noted earlier, axons of these second-order neurons travel as internal arcuate fibers, crossing the midline to form the medial lemniscus, and terminate on third-order neurons located in the contralateral ventral posterolateral nucleus of thalamus. The axons of these third-order neurons then terminate in the lateral aspect of the sensorimotor cortex. The fasciculus cuneatus is also involved in mediating conscious proprioception.
The fasciculi gracilis and cuneatus are also referred to as the dorsal (posterior) columns. Damage to these tracts results in symptoms that appear ipsilateral to the affected dorsal columns in the dermatomes at and below the level of the spinal cord lesion. The symptoms include loss of tactile sense (vibration, deep touch, and two-point discrimination) and kinesthetic sense (position and movement). The patient with a lesion affecting the cervical cord cannot identify an object placed in his or her hand ipsilateral to the lesion. If the lesion is located at the level of the lumbar cord, then the loss of these forms of sensation will be restricted to an ipsilateral lower limb. The patient cannot perceive sensations, such as touch or pressure, and his or her movements are poorly coordinated and clumsy because of the loss of conscious proprioception of his or her position in space.
Dorsal (Posterior) Spinocerebellar Tract
The course of this tract is shown in Figure 9-8A. The peripheral processes of the first-order neurons (located in the dorsal root ganglion) innervate mainly muscle spindles and, to a lesser extent, Golgi tendon organs (located at the junction of the muscle and tendon). The central processes of these sensory neurons project to the nucleus dorsalis of Clarke that extends from C8 to L2. Axons of neurons located in the dorsal nucleus of Clarke ascend ipsilaterally (i.e., the tract is uncrossed), reach the inferior cerebellar peduncle (restiform body) in the medulla, and terminate ipsilaterally in the cerebellar vermis of the anterior lobe. Although the nucleus dorsalis of Clarke receives afferents from all parts of the body (C8-L2) except the head and neck, functionally it transmits information about muscle spindle and tendon afferents from the ipsilateral caudal aspect of the body and legs. In so doing, this tract provides the cerebellum with information about the status of individual muscles as well as groups of muscles (e.g., how long each muscle is, how fast each muscle is moving, and how much tension is on each muscle). The individual is not aware of this information going to the cerebellum (non-conscious proprioception). With this information, the cerebellum is enabled to coordinate and integrate neural signals controlling movement of individual lower limb muscles and posture. Damage to the dorsal spinocerebellar tract results in the loss of nonconscious proprioception and coordination ipsilateral to the lesion.
FIGURE 9-7 Diagram showing the course of fibers in the dorsal column. The fasciculus gracilis exists at all levels of the spinal cord and contains long ascending fibers from the lower limbs (shown in red). The fasciculus cuneatus exists in thoracic (T) segments above T6 (T1-T6) and cervical (C) segments (C1-C8) and contains long ascending fibers from the upper limbs (shown in blue). The axons of second-order neurons (neuron II) in the nucleus gracilis and cuneatus travel as internal arcuate fibers and cross in the midline to form the medial lemniscus, which ascends through the medulla, pons, and midbrain and terminates in the contralat-eral ventral posterolateral nucleus of the thalamus. Axons of third-order neurons (neuron III) in the thalamus travel in the internal capsule and terminate in the senso-rimotor cerebral cortex. For other details, see text. neuron I = first-order neuron; L = lumbar; S = sacral.
FIGURE 9-8 (A) The dorsal (posterior) spinocerebellar tract. (B) The cuneocerebellar tract. See text for details. C = cervical