The spinal cord is a critical component for the transmission of sensory information to the brain as well as for the regulation of motor and autonomic functions. It receives sensory information from somatic and visceral receptors through dorsal roots, transmits this information to higher centers in the brain through ascending tracts, receives signals from higher centers through descending tracts, and transmits the signals to somatic and visceral target sites via the ventral roots. A number of reflexes are also mediated at the level of the spinal cord. These functions of the spinal cord and the anatomical, physiological, and clinical considerations associated with them are presented in this topic.
Gross Anatomy
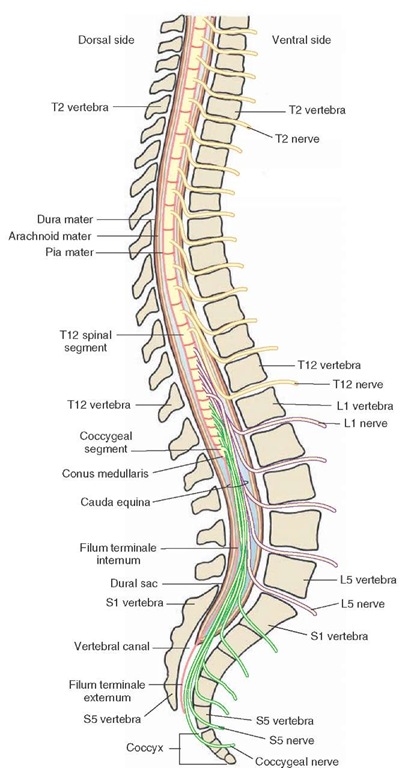
The spinal cord is located within the vertebral canal and extends from the foramen magnum to the rostral edge of the second lumbar vertebra (Figs. 9-1 and 9-2). The coverings (meninges) of the spinal cord.
FIGURE 9-1 Cervical spinal cord. Note that the spinal nerves from spinal segments C1-C7 exit through the intervertebral foramen located rostral to the cervical vertebra of the same name. The spinal nerve from C8 segment of the spinal cord exits through the intervertebral foramen located caudal to T1 (thoracic) vertebra.
FIGURE 9-2 Spinal segments caudal to the cervical region. Note that the spinal nerves from thoracic (T), lumbar (L), and sacral (S) segments of the spinal cord exit through the intervertebral foramen located caudal to the vertebra of the same name. Note also the conus medullaris (caudal end of the spinal cord) and the cauda equina.
The caudal end of the spinal cord and the structures associated with it are shown in Figure 9-2. The conical-shaped caudal end of the spinal cord, known as the conus medullaris, is located at the rostral edge of the second lumbar vertebra. A thin filament enclosed in pia and consisting of glial cells, ependymal cells, and astrocytes emerges from the conus medullaris. This filament is called the filum terminale internum. It extends from the conus medullaris and passes through the caudal end of the dural sac. At this level, a caudal thin extension of the spinal dura, called the coccygeal ligament (filum terminale externum) surrounds the filum terminale. The coccygeal ligament, with the filum terminale in it, attaches to the coccyx and, thus, anchors the spinal cord and the fluid-filled dural sac to the caudal end of the vertebral canal.
The spinal cord occupies the whole length of the vertebral canal up to the third month of fetal life. Then it lengthens at a slower rate than does the vertebral column. As a result, in an adult, the spinal cord occupies only the upper two thirds of the vertebral column. For this reason, the caudal end of the spinal cord in the normal adult is located at the rostral edge of the second lumbar vertebra (or caudal edge of the first lumbar vertebra). Therefore, the lumbar and sacral nerve roots have to descend some distance within the vertebral canal before they exit from their respective intervertebral foramina. The lumbosacral nerve roots surround the filum terminale and form a cluster that resembles the tail of a horse and that is called the cauda equina (Fig. 9-2). The subarachnoid space is widest from the caudal end of the spinal cord (i.e., caudal edge of the first lumbar vertebra) to the second sacral vertebra and contains no central nervous system (CNS) structures except the filum terminale and the nerve roots of cauda equina. This space is known as the lumbar cistern.Because of this anatomic feature, this space is most suitable for the withdrawal of cerebrospinal fluid (CSF) by lumbar puncture. The site for performing a lumbar puncture changes with age in childhood. For example, in children, the caudal end of the spinal cord is usually located at the third lumbar vertebra (L3); therefore, the needle for lumbar puncture is inserted at the L4-L5 level.
Spinal segmentation is based on the sites where spinal nerves emerge from the spinal cord. Thirty-one pairs of spinal nerves emerge from the spinal cord. At each level, the spinal nerves exit through the intervertebral foramina. In the thoracic, lumbar, and sacral regions of the cord, spinal nerves exit through the intervertebral foramina just caudal to the vertebra of the same name. In the cervical region, these nerves exit through the intervertebral foramina just rostral to the vertebra of the same name. The eighth cervical spinal nerve (C8) exits through the intervertebral foramen just rostral to the first thoracic vertebra (Fig. 9-1).
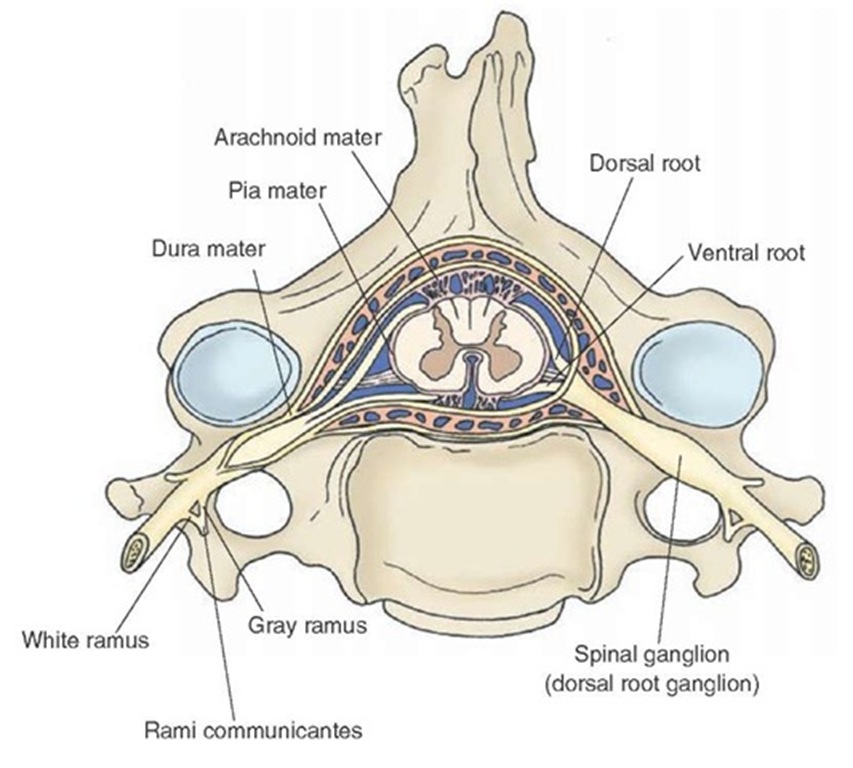
Each spinal nerve consists of a dorsal root (containing afferent fibers) and a ventral root (containing efferent fibers). The dorsal root is absent in the first cervical and coccygeal nerves. The dorsal and ventral roots travel a short distance within the dural sac surrounding the spinal cord, penetrate the dura, and enter the intervertebral foramen. The spinal ganglion (dorsal root ganglion) is located within the intervertebral foramen and contains the neurons that give rise to afferent fibers entering the spinal cord. The dorsal and ventral roots are joined distal to the spinal ganglion and form the common spinal nerve trunk (Fig. 9-3). The common spinal nerve trunk is connected with the sympathetic chain of paravertebral ganglia that are located on either side of the vertebral column through the white and gray rami (rami communicantes.
FIGURE 9-3 Spinal nerves. Note the location of dorsal and ventral roots and the dorsal root ganglion (as described in the text).
The spinal cord is cylindrical in shape and is enlarged at the cervical and lumbar regions. The cervical enlargement includes four lower cervical segments and the first thoracic segment. The nerve roots emerging from this enlargement form the brachial plexus and innervate the upper extremities. The lumbar plexus (comprising the nerve roots from L1-L4) and sacral plexus (consisting of nerve roots from L4-S2) emerge from the lumbar enlargement. The lumbar plexus innervates the lower extremities. The sacral spinal nerves emerging from the conus medullaris contain para-sympathetic fibers and motor fibers innervating the bladder and its sphincters, respectively.
Internal Structure
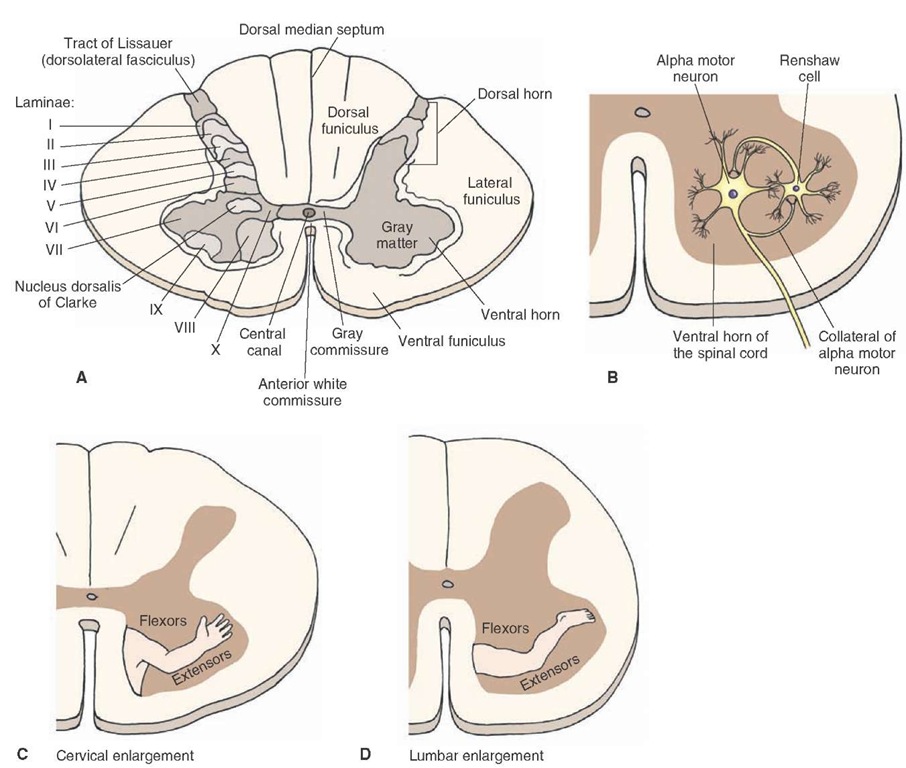
Examination of a transverse section of the spinal cord reveals the presence of central gray matter, shaped like a butterfly, which contains cell columns oriented along the rostro-caudal axis of the spinal cord. This butterfly-shaped gray area is surrounded by white matter consisting of ascending and descending bundles of myelinated and unmyelinated axons that are called tracts or fasciculi. The neurons comprising these tracts have similar origins and sites of termination. A bundle containing one or more tracts or fasciculi is called a funiculus. In each half of the spinal cord, there are three funiculi: (1) the dorsal (posterior) funiculus, which is located between the dorsal horn and a midline structure called the dorsal (posterior) median septum; (2) the lateral funiculus, which is located between the sites where the dorsal roots enter and ventral roots exit from the spinal cord; and (3) the anterior (ventral) funiculus, which is located between the anterior (ventral) median fissure and the site where the ventral roots exit (Fig. 9-4A).
In each half of the spinal cord, the dorsal horn of the butterfly-shaped gray matter reaches the surface where the dorsal rootlets of the spinal nerves enter. The ventral horn of this butterfly-shaped gray matter does not reach the ventral surface of the spinal cord. The two sides of the gray matter are connected by a band of gray matter called the gray commissure. The anterior white commissure, consisting of decussating axons of nerve cells, is located ventral to the gray commissure. The central canal is located in the gray commissure (Fig. 9-4A). The lumen of the central canal in the adult spinal cord may be filled with debris consisting of macrophages and neuroglial processes.
FIGURE 9-4 Gross anatomy of the spinal cord in transverse section. (A) The central gray matter is shaped like a butterfly. Note the three funiculi in each half of the spinal cord: the dorsal (posterior) funiculus, the lateral funiculus, and the ventral (anterior) funiculus. The two sides of the gray matter are connected by the gray commissure. Note the location of laminae I through X. Lamina VII contains the nucleus dorsalis of Clarke. (B) A collateral emerging from the axon of an alpha motor neuron activates the Renshaw cell, which, in turn, inhibits the alpha motor neuron. (C and D) Note the somatotopic arrangement of neurons in laminae VIII and IX and the location of the neurons innervating the flexors and extensors.
The gray matter of the spinal cord contains primarily neuronal cell bodies, dendrites, and myelinated and unmy-elinated axons, which are either projecting from the white matter to innervate neurons located in the gray matter or exiting from the gray matter to the white matter. The white matter consists of ascending and descending tracts of myelinated and unmyelinated fibers.
Cytoarchitectural Organization of the Spinal Gray Matter
The architectural organization of the spinal gray matter was described by Rexed in 1952. He reported that clusters of cells are arranged in the spinal cord in 10 zones. A description of these zones, referred to as Rexed laminae I—X, is provided in the following paragraphs, and their location is shown in Fig. 9-4A. For important structures located in these laminae, see Table 9-1. The zone of Lissauer (dorsolateral fasciculus) consists of fine myelinated and unmyelinated dorsal root fibers that enter the medial portion of this zone. A large number of propriospinal fibers, which interconnect different levels of the substantia gelatinosa (described later in this section), are also present in this zone. Laminae I through IV are located in the dorsal horn of the spinal cord. The cells situated in these laminae receive primarily exteroceptive (i.e., pain, temperature, and tactile) inputs from the periphery.
Lamina I contains terminals of dorsal root fibers mediating pain and temperature sensations that synapse, in part, on the group of cells called the posteromarginal nucleus. The axons of the cells in the posteromarginal nucleus cross to the opposite side and ascend as the lateral spinothalamic tract. Lamina II is located immediately below lamina I and contains the substantia gelati-nosa. The neurons in the substantia gelatinosa modulate the activity of pain and temperature afferent fibers. Activation of peripheral pain receptors results in the release of substance P and glutamate in the substantia gelatinosa. Laminae III and IV, both of which contain the proper sensory nucleus, are located in the lower aspect of the dorsal horn. The proper sensory nucleus receives inputs from the substantia gelatinosa and contributes to the spinothalamic tracts mediating pain, temperature, and crude touch. Lam-ina V is located at the neck of the dorsal horn; neurons located in this lamina receive descending fibers from the corticospinal and rubrospinal tracts and give rise to axons that contribute to the spinothalamic tracts. Lamina VI is present only in cervical and lumbar segments. It contains a medial segment that receives muscle spindle and joint afferents, and also contains a lateral segment that receives fibers from descending corticospinal and rubrospinal pathways. Neurons in this region are involved in the integration of somatic motor processes. Lamina VII, which is located in an intermediate region of the spinal gray matter, contains the nucleus dorsalis of Clarke, which extends from C8 through L2. This nucleus receives muscle and tendon afferents. Axons of this nucleus form the dorsal spinocerebellar tract, which relays this information to the ipsilateral cerebellum.
Other important neurons located in lamina VII include the sympathetic preganglionic neurons, which constitute the intermediolateral cell column (IML) in the thora-columbar cord (T1-L2), parasympathetic neurons located in the lateral aspect of sacral cord (S2-S4), and numerous interneurons such as Renshaw cells. The output of alpha motor neurons, which are located in the ventral horn of the gray matter, is regulated by Renshaw cells through a mechanism called "recurrent inhibition." Renshaw cells are interneurons that make inhibitory (glycinergic) synapses on the alpha motor neurons and receive excitatory (cholinergic) collaterals from the same neurons. When an alpha motor neuron is excited, it activates Renshaw cells via the excitatory (cholinergic) collaterals. Renshaw cells, in turn, inhibit, via glycinergic synapses, the activity of the same alpha motor neuron (Fig. 9-4B).
TABLE 9-1 Key Structures in the Spinal Rexed Laminae
|
Laminae |
Key Structures |
|
I |
Dorsal root fibers mediating pain, temperature, and touch sensations; posteromarginal nucleus |
|
II |
Substantia gelatinosa neurons mediating pain transmission |
|
III & IV |
Proper sensory nucleus that receives inputs from substantia gelatinosa and contributes to spinothalamic tracts mediating pain, temperature, and touch sensations |
|
V |
Neurons receiving descending fibers from corticospinal and rubrospinal tracts; neurons that contribute to ascending spinothalamic tracts |
|
VI |
Present only in cervical and lumbar segments; lateral segment receives descending corticospinal and rubrospinal fibers; medial segment receives afferents from muscle spindles and joint afferents |
|
VII |
Nucleus dorsalis of Clarke extending from C8-L2 receives muscle and tendon afferents; axons from this nucleus form spinocerebellar tract; intermediolateral cell column containing sympathetic preganglionic neurons from T1-L3; parasympathetic neurons located in S2-S4 segments; Renshaw cells |
|
VIII & IX |
Located in the ventral horn; alpha and gamma motor neurons innervating skeletal muscles; neurons in medial aspect receive inputs from vestibulospinal and reticulospinal tracts and innervate axial musculature for posture and balance; neurons in lateral aspect receive inputs from corticospinal and rubrospinal tracts and innervate distal musculature |
|
X |
Gray matter surrounding central canal |
Laminae VIII and IX are located in the ventral horn of the gray matter of the spinal cord. Neurons in this region, which receive inputs from the descending motor tracts from the cerebral cortex and brainstem, give rise to both alpha and gamma motor neurons that innervate skeletal muscles. Neurons in these laminae are somatotopically arranged; neurons providing innervation to the extensor muscles are located ventral to those innervating the flexors, and neurons providing innervation to the axial musculature are medial to those innervating muscles in the distal parts of the extremity (Fig. 9-4, C and D). Neurons situated in the medial aspect of the ventral horn receive afferents from the vestibulospinal and reticulospinal systems and, in turn, innervate the axial musculature. This anatomical arrangement allows descending pathways to regulate the axial musculature (i.e., posture and balance). In contrast, neurons situated in the lateral aspect of the ventral horn receive afferents from the corticospinal and rubrospinal pathways. Axons of these neurons mainly innervate the distal musculature. This arrangement provides a basis by which these descending pathways can have a preferential influence upon the activity of the distal musculature. Thus, in the ventral horn, motor neurons are located according to the muscle that they innervate. Neurons providing innervation to the extensor muscles are located ventral to those innervating the flexors. Neurons providing innervation to the axial and limb girdle musculature are medial to those innervating muscles in the distal parts of the extremity. In the cervical part of the spinal cord (segments C3, C4, and C5), lamina IX contains phrenic motor neurons that provide innervation to the diaphragm. Thoracic respiratory motor neurons, which innervate intercostal and other rib cage and back muscles, are located in lamina IX of the thoracic segments. The gray matter surrounding the central canal constitutes lamina X.