Learning Objectives
1. Name the major hormones that influence the female reproductive system.
2. Describe the functions of the ovaries, uterus, clitoris, and vagina.
3. Explain the role of the mammary glands in the reproductive process.
4. Describe the functions of LH, FSH, estrogens, and progesterone in the female reproductive system.
5. Discuss the process of oocyte maturation and ovulation.
6. Explain the three phases of the ovarian cycle, including what occurs during each phase.
7. Describe the three phases of the uterine cycle, including what occurs during each phase.
8. Discuss menopause and the physical changes that accompany it.
9. Identify two effects of the aging process on the female reproductive system other than menopause, and list the nursing implications for each effect.
|
IMPORTANT TERMINOLOGY |
||
|
Bartholin’s gland hymen |
ovary |
|
|
cervix |
labia majora |
oviduct |
|
clitoris |
labia minora |
ovulation |
|
embryo |
mammary gland |
perineum |
|
endometrium |
menarche |
progesterone |
|
estrogen |
menopause |
uterus |
|
fallopian tube |
menstruation |
vagina |
|
fimbriae |
mons pubis |
vulva |
|
gonadotropic |
oocyte |
zygote |
|
hormone |
ova |
|
|
Acronyms |
|
|
ERT |
HRT |
The male and female reproductive systems are responsible for the continuation of the human species. Human reproduction occurs by internal fertilization via sexual intercourse. The erect penis of the male is inserted into the female vagina; ejaculation of semen containing the male sperm is deposited in the vagina. The female system produces eggs, or ova. Sperm can fertilize ova, thereby beginning the reproductive process. The female reproductive system also has the amazing added function of providing an environment necessary for growth and development of a fetus (a developing infant in the uterus). The word element gyn- or gyneco- means woman. (A physician specializing in treating disorders unique to women is a gynecologist.)
Development of both the reproductive and urinary systems is closely related. A structure called the Müllerian duct in fetal life develops to form a number of female structures.
In addition, a number of fetal structures are the same in the male and female, but develop differently as a result of hormones. Although they are the same in fetal life, they are differentiated between the sexes in adult life. These structures are known as homologous structures. Examples include:
• Cowper’s gland in male; Bartholin’s glands in female— secrete lubricants
• Penis in male; clitoris in female—contain erectile tissue and contribute to sensation
• Testes in male; ovaries in female—produce gametes
• Prostate gland in male; Skene’s gland in female—produce ejaculatory fluid and sensation.
Although men begin to produce sperm during puberty and continue to do so for the rest of their lives, a woman’s reproductive capacity is limited, beginning with the first menstrual period and ending during menopause. The menstrual cycle is extremely important in understanding the female reproductive system. It is explained later in this topic.
FIGURE 29-1 · The female reproductive system (interior view), illustrating the location of fertilization of the ovum. Red arrows indicate the path of the ovum to the site of fertilization. Blue arrows indicate the path of spermatozoa. (The fertilized ovum then continues down into the uterus.)
Structure and Function
The female reproductive system consists of paired ovaries and oviducts, and the uterus, vagina, and external genital structures. The internal organs—uterus, vagina, and ovaries—are located within the pelvis between the urinary bladder and rectum. These structures are held in place by a group of ligaments, the most conspicuous of which are the broad and round ligaments.
FIGURE 29-2 • The female reproductive organs, as seen in sagittal section.
The external structures consist of components of the vulva. The mammary glands (breasts) are also considered female reproductive organs. Figures 29-1 and 29-2 illustrate the female reproductive system. Box 29-1 reviews its primary functions.
REPRODUCTIVE ORGANS
Ovaries
The gonads (sex organs) in women are the ovaries. The ovaries produce female gametes or ova (singular: ovum) and secrete female sex hormones (estrogens). Although several estrogens exist (the primary one is estradiol), the entire classification estrogen commonly refers to all female sex hormones collectively. The ovaries are two almond-shaped glands, each about 1.5 inches (3.8 cm) in length, located within the brim of the pelvis, one on either side of the uterus (see Fig. 29-1). (The combining form relating to ovary is oophor/o-.)
BOX 29-1. Functions of the Female Reproductive System
Development of Sexual Characteristics
♦ Secrete hormones that initiate puberty
♦ Maintain specific female sexual characteristics
♦ Secrete mucus, vaginal fluids, and other substances
Reproduction
♦ Produce ova
♦ Pass genetic information to offspring
♦ Participate in copulation and fertilization
♦ Maintain and nourish fetus until birth
Infant Nourishment
♦ Produce breast milk
Oviducts
Sometimes called uterine tubes or ovarian tubes, the oviducts or fallopian tubes are the passageway for the ovum between the ovary and the uterus (see Fig. 29-1). The oviducts are 4-5 inches (10-12.5 cm) long. One oviduct is connected to each side of the uterus; each is associated with one ovary.
Key Concept The human ovum consists of protoplasm enclosed within a two-layered cell wall.The outer layer is the zona pellucida; the inner layer is the vitelline membrane.) The ovum cell contains a large nucleus, within which is a nucleolus called the germinal spot. It is believed that all the ova a female will ever have are present at birth. The ovum is larger than the sperm cell and is the only human cell normally visible to the naked eye.
As the ovum bursts from the ovary into the pelvic cavity, the oviduct catches it in structures called fimbriae. Fimbriae are the fringe-like ends of the oviducts. Cilia on the inner surfaces of the fimbriae, and on the lining of the oviducts, help move the ovum toward the uterus. Smooth muscles of the oviducts contract in peristaltic waves, which also help to propel the ovum. The inner layer of the oviducts contains mucus-secreting cells that assist in transporting the ovum, and may also provide nutrients for the ovum as it travels in the oviducts. (The transit of the ovum from the ovary to the uterus may occur in a few hours or may take several days.)
Fertilization of the ovum (the meeting of the sperm and the ovum) normally occurs about midway in the oviduct. The fertilized ovum is called a zygote. The zygote travels to the uterus, where it becomes embedded in the uterine lining in preparation for further growth. Once the zygote becomes completely embedded in the lining, it is called an embryo. If fertilization does not occur, the ovum dissolves. Because no closed connection exists between the ovary and the oviduct, it is possible for the ovum to “escape” into the abdominal cavity.
Key Concept Normally fertilization occurs in the outer third of the oviduct, although it may occur in the uterus. It is the oviduct that is ligated (tied) and cut in the sterilization procedure called tubal ligation.
Nursing Alert An ectopic (outside the uterus) pregnancy within the oviduct is an emergency situation, endangering the life of the mother. In this situation, the fertilized ovum becomes lodged in the oviduct; this can lead to ductal rupture and hemorrhage.
Uterus
The uterus (womb) is a hollow, muscular, upside-down-pear-shaped organ in the center of the pelvic cavity above and behind the urinary bladder (see Fig. 29-2). The uterus is considered to be the major female sex organ, even though the gonads are the ovaries. The non-pregnant uterus is about 3 inches (7.5 cm) long, 2 inches (5 cm) wide, and 1 inch (2.5 cm) thick. The zygote matures into a full-term fetus in the uterus. The uterus normally is tipped forward (ante-verted), but in some women it is tipped posteriorly (retro-verted). Although it is movable, the uterus is held in position by strong structures, the broad ligament (see Fig. 29-1) and the round ligament. During pregnancy, the uterus increases its size about 16 times (from about 60 g to about 950 g); its capacity increases from about 2.5 mL to 5,000 mL. After a term pregnancy, the uterus shrinks considerably, but never returns to its original size.
Figure 29-1 shows the uterus. The fundus is the round upper surface; the oviducts enter here. The body (corpus) is the broad, large central portion. The cylindrical or conical cervix is the narrow lower end, which opens into the vagina at the external cervical os (mouth of the cervix). The normal size of the cervical os is about the diameter of the graphite in a pencil. The non-pregnant cervix feels like the end of your nose. About half of the cervix can be visualized during vaginal examination. (The combining form relating to uterus is hystero-. Removal of the uterus is called hysterectomy.)
The uterus has three layers: serous, muscular, and mucous. The serous (outer) layer is called the perimetrium and is a fold of the peritoneum. The muscular layer is called the myometrium; it is the smooth muscle that increases in size during pregnancy and contracts during labor and delivery. The mucous layer is the endometrium, which forms the maternal portion of the placenta during pregnancy.
The uterus receives the fertilized ovum and provides housing and nourishment for a fetus. At the end of gestation, the uterus expels the fetus (delivery). Pregnancy, labor, and delivery are discussed in Unit 10. In some cases, a couple has difficulty conceiving a child.
Vagina
The cervix projects into a fibromuscular canal, which is about 4 inches (10 cm) long and is called the vagina (see Fig. 29-1). The vagina is attached to the uterus through the cervix and meets the external organs at the vulva. The vagina’s superior, domed portion has deep recesses, called the fornices (singular: fornix), around the portion of the cervix extending into the vagina. Glandular secretions from Bartholin’s glands (greater vestibular glands) and the mucous membrane lining its walls moisten the vagina. The mucus is acidic and retards microbial growth. (The alkaline semen can temporarily neutralize the vagina’s acidic environment.) Rugae are expandable folds within the vaginal walls that accommodate insertion of the penis and passage of the fetus during childbirth. The vagina’s functions are to receive sperm, to provide an exit for menstrual flow, and to serve as the birth canal.
The hymen is a thin membrane over the vaginal opening. It may close the vaginal orifice completely, or it may be absent from birth. More commonly, it has one or more perforations. A woman can injure the hymen in various ways (e.g., during normal exercise, or horseback riding, by using tampons, or during the first sexual intercourse). The presence or absence of a hymen is not a reliable indicator of a woman’s virginity.
External Genitalia
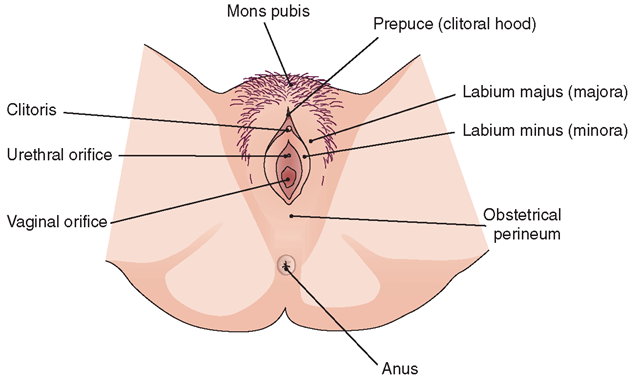
The external genitalia are collectively called the vulva (pudendum). The vulva includes the vestibule and its surrounding structures. The vestibule contains the openings of the urethra, the vagina, and the Bartholin’s glands (see Fig. 29-1). The external structures also include the mons pubis, labia majora, labia minora, clitoris, and prepuce (Fig. 29-3).
The mons pubis is a fatty pad over the symphysis pubis (see Fig. 29-3). Posterior to the mons pubis extend two rounded folds of skin called the labia majora (labium majus). After puberty, the mons pubis and the labia majora are covered with coarse pubic hair. A thin pair of skin folds medial to the labia majora are the labia minora (labium minus), which unite just above and with the clitoris to form the prepuce of the clitoris or clitoral hood. The labia minora skin folds enclose the vaginal opening and can be spread apart or “opened” to expose the vestibule floor. The vestibule floor contains Bartholin’s glands (greater vestibular glands), which lubricate the vagina. If the openings of these glands become obstructed, Bartholin’s cysts can result.
The clitoris is a small erectile structure that responds to sexual stimulation. The structure of the clitoris is similar to the structure of the penis. Both become engorged with blood as a result of sexual excitement, and stimulation of either structure often leads to orgasm.
The female (obstetrical) perineum is the space between the vaginal orifice and the anus. It is made up of strong muscles that act as sling-like supports for pelvic organs.
Key Concept During childbirth, the skin and muscles of the perineal area may be torn.To prevent such tearing, an incision called an episiotomy is often made. (A clean, straight incision heals better than an irregular skin and muscle tear) Slow stretching of the perineum during delivery may prevent tearing and make an episiotomy unnecessary
BREASTS
The breasts are not involved in gestation; however, they are hormonally influenced and are directly linked to the reproductive process, providing nutrition for babies following childbirth. Before puberty, breast structure in boys and girls is similar. Both have rudimentary glandular systems. With the onset of puberty, estrogens and progesterone in girls lead to breast enlargement. Both boys and girls may have some breast sensitivity in early puberty. Boys may develop slight swellings as well, but this is usually temporary.
Within the breasts are mammary glands. They are modified sweat glands (Fig. 29-4) and are located anterior to the pec-toralis major muscles. Hormones (prolactin and oxytocin) stimulate them to produce and release milk after childbirth. Each breast is divided into 15-20 lobes of glandular tissue, covered by adipose (fat) tissue, which gives the breast its shape. The lobes are made up of lobules, which consist of milk-secreting cells in glandular alveoli. From the alveoli, small lactiferous ducts converge toward each nipple like the spokes of a wheel. Each lactiferous duct forms a small reservoir for milk.
The structures of the breast include the nipple, the areola, and the areolar glands. The nipple is a circular projection containing some erectile tissue. It is surrounded by the pigmented areola. Areolar glands, which are close to the skin’s surface, make the areola appear rough. The secretions of the areolar glands keep the nipples from drying out, particularly during lactation (milk production). Hormonal release of estrogen and progesterone during pregnancy causes the breasts to enlarge. The areolae become more heavily pigmented and do not totally return to their previous color after pregnancy.
FIGURE 29-3 · The external female genitalia, seen from below. The area lying between the orifice of the vagina and the anus is the obstetrical perineum. Note the location of the urethral (urinary) orifice (meatus, opening).
FIGURE 29-4 · The breast, showing the glandular tissue and ducts of the mammary glands.
NCLEX Alert NCLEX questions may require knowledge of the terminology of the structures and functions of the female reproductive system. Be sure you can differentiate between appropriate and inappropriate nursing care, laboratory results, or diagnostic procedures.