Approval and Accreditation of Nursing Programs
Approved Nursing Programs
Nursing programs are very different from general college courses, such as history, mathematics, or English. Nursing schools must maintain specific educational standards that are defined by legislating bodies. As such, nursing programs must have approval from a specific state agency or nursing authority, which is usually a state, provincial, or territorial Board of Nursing. The approval agency visits the school and determines whether the students are receiving an appropriate education. Reapproval of the nursing program may be required on a regular schedule as determined by the agency.
The purpose of approval of a school’s educational criteria is to protect the consumers of healthcare against unqualified nurses. A minimal standard of education is required. Approval is mandatory (required), meaning that a school must be approved or its graduates cannot be licensed.
The word approved tells you the following about a school:
• It teaches specific things a nurse must know.
• It has stated objectives and teaches to those objectives.
• It provides experience with the types of individuals the nurse will care for when practicing nursing.
• It employs qualified instructors to teach and to supervise the students’ practice in the classroom and in the healthcare facility.
• It prepares graduates eligible for examination and licensure as LPNs, LVNs, or RNs.
• It has courses of the required minimum length.
Accredited Nursing Programs
Accreditation is voluntary and does not specifically concern licensure of graduates. A program can be approved without being accredited, but it cannot be accredited without first being approved by the state’s Board of Nursing.
Accreditation is not a matter of law. The accreditation of a school means that an agency other than the state has reviewed the nursing program in detail. If a nursing program has been accredited, the program has met criteria established by that agency. Application for accreditation is voluntary on the part of the program; accreditation is not given to all programs. That a school is accredited gives further evidence of its excellence because the program must undergo a detailed evaluation to become accredited. A program need not be accredited for its graduates to become licensed. The National League for Nursing (NLN) has established standards of accreditation for nursing education for both RNs and LPNs.
As a nursing student, you must understand that a difference exists between approval and accreditation of a nursing program. Each state has a legislated Nurse Practice Act that defines the approval process. Nurse Practice Acts delineate the educational requirements, roles and functions, and disciplinary actions of a nurse.
Many nursing programs have entrance requirements. Most programs require entrants to be high school graduates. Nursing programs may also require their entrants to have taken certain courses, such as anatomy, physiology, nutrition, or pharmacology. Nursing students may also be required to be immunized against several diseases, such as hepatitis B. Drug testing, alcohol testing, and criminal background checks also can be mandated. Requirements are established to maintain client safety and may be required by the educational program or the clinical facilities in which the training occurs. Programs must consider applicants for admission without regard to gender, age, marital status, sexual preference, race, or religion. To graduate from a nursing program, a student nurse must meet the minimal standards of the approved nursing program.
NCLEX Alert NCLEX clinical scenarios include situations that will need you to select the appropriate healthcare individual (MD, RN, LP/LVN or assistive personnel). For example, who is responsible for the care of the client during the time of the clinical scenario? You must know the major legal differences and responsibilities for the levels of healthcare personnel.
LICENSURE OF NURSES
Licensing laws, often referred to as Nurse Practice Acts, protect the public from unqualified workers and establish standards for the profession or occupation. Licensing laws establish a minimal level of requirements for competence and practice. Obtaining licensure helps the public determine the difference between a qualified and an unqualified worker.
The first licensure laws for nursing were passed in 1903 in North Carolina, New York, Virginia, and New Jersey. The first LPN law was passed in Mississippi in 1914. In 1940, fewer than 10 states had LPN laws, but by 1955 all states had LPN laws. Every state and the District of Columbia, Puerto Rico, Guam, American Samoa, the Virgin Islands, the Canadian provinces, and the North Mariana Islands now have licensing laws for both RNs and LPNs.
Any student who has graduated from an approved nursing program is eligible to take an examination provided by the National Council of State Boards of Nursing. The examination is called the National Council Licensure Examination (NCLEX). The NCLEX-RN is the licensing examination for registered nurses. The NCLEX-PN is for licensed practical/ vocational nurses. After candidates have successfully completed the NCLEX and before they receive licenses, they may be required by the state Board of Nursing to pay licensing fees and submit fingerprints and documentation from nursing programs.
State licensing laws have individual variations, but all nurse practice laws state that it is illegal for any nurse to practice nursing for pay without a license. Practice acts differentiate between LPN/LVN and RN licenses. This regulation is called mandatory licensure. The mandatory law designates the functions, duties, and responsibilities of the nurse and use of the title “nurse.” Mandatory licensure requires that a nurse cannot perform the functions designated as exclusive to nursing without proper licensure in that state. Healthcare consumers are protected because minimal competence levels are established and enforced by regulatory state agencies (i.e., the State Board[s] of Nursing). Practicing nursing without a license is called permissive licensure, but rarely occurs today.
Often nurses move from one state to another. Regulations provide for the licensed nurse to continue his or her nursing practice in a new state without retaking the licensing examination. Endorsement is a form of agreement between states, particularly state licensing agencies. One state recognizes or endorses the qualifications of another state. However, each state board of nursing has its fees the individual pays for a license in that state. For example, an LVN in California can practice nursing in Minnesota as an LPN without retaking the NCLEX-PN, but the individual will have to apply and pay for the new Minnesota license. Reciprocity is another type of recognition of previous education and experience.
Key Concept Licensure establishes a minimal level of competence for nursing. It ensures that a licensed nurse meets a basic level of excellence in practice and knowledge.
The Nurse’s Pledge
All nurses are expected to practice ethically and conduct themselves appropriately as members of a specific group. As a nurse, you also accept responsibilities within the role delineated by licensure.
Many ethical principles are reflected in the Nurse’s Pledge, which many students recite at graduation. Even if the pledge is not part of your graduation ceremony, it should serve as a guide for nursing practice. RNs recite the Florence Nightingale Pledge, and LPNs recite the Practical Nurse’s Pledge (Box 2-2). The basic philosophy of nursing care espoused in both pledges is the same. Notice the similarity between them.
THEORIES OF NURSING
As a science, nursing is based on the theory of what nursing is, what nurses do, and why. Nursing is a unique discipline and is separate from medicine. It has its own body of knowledge on which delivery of care is based.
Nursing programs usually base their curricula on one or more nursing theories. Such theories provide a skeleton on which to hang knowledge. This theoretical framework gives you and other students a basis for forming a personal philosophy of nursing. It also helps you to develop problem-solving skills systematically. A theoretical framework provides a reason and a purpose for nursing actions. Other factors also involved in nursing actions include ethics, safety, confidentiality, and culture. The theoretical framework on which this topic is based is that of meeting basic human needs.
Throughout this topic, you will learn ways to perform nursing procedures. You will also be presented with rationales, or reasons for these actions. These rationales are based on nursing’s knowledge base. After you graduate and become more experienced, you will realize that more than one correct way exists to perform particular procedures. You must always follow the nursing protocols of the healthcare facility in which you are employed.
Nursing theories are often expressed in relationship to factors such as mind, body, spirit, and emotions. Most theories also include a definition of health. Be sure to consider all these factors when delivering nursing care so that you provide holistic care—care of the whole person. Among the many nursing theories are those of Florence Nightingale, Virginia Henderson, Dorothea Orem, Sister Callista Roy, and Betty Neuman. Table 2-2 outlines the general concepts related to these theories.
BOX 2-2.
Nursing Pledges
|
Florence Nightingale Pledge I solemnly pledge myself before God and in the presence of this assembly: To pass my life in purity and to practice my profession faithfully. |
|
I will abstain from whatever is deleterious and mischievous, and will not take or knowingly administer any harmful drug. |
|
I will do all in my power to maintain and elevate the standards of my profession, and will hold in confidence all personal matters committed to my keeping, and all family affairs coming to my knowledge in the practice of my profession. |
|
With loyalty will I endeavor to aid the physician in his work, and devote myself to the welfare of those committed to my care. |
|
The Practical Nurse’s Pledge Before God and those assembled here, I solemnly pledge: |
|
To adhere to the code of ethics of the nursing profession. |
|
To cooperate faithfully with the other members of the nursing team and to carry out faithfully and to the best of my ability the instructions of the physician or the nurse who may be assigned to supervise my work. |
|
I will not do anything evil or malicious and I will not knowingly give any harmful drug or assist in malpractice. |
|
I will not reveal any confidential information that may come to my knowledge in the course of my work. |
|
And I pledge myself to do all in my power to raise the standards and the prestige of practical nursing. |
|
May my life be devoted to service, and to the high ideals of the nursing profession. |
ROLES AND RESPONSIBILITIES OF THE NURSE
Today’s nurse functions in a number of roles. As a nurse, you have a responsibility to maintain your own health. You also will need to project a professional image to your clients, their families, and the general public. Doing so will help others have confidence in your nursing abilities.
Contemporary Nursing Roles
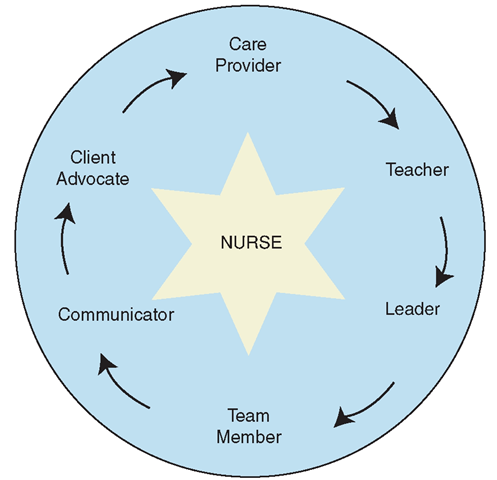
Nurses are respected as a healthcare resource in the community. Examine the following roles of the nurse (Fig. 2-2). As you progress through your nursing program, you may be able to think of other roles that nurses assume in their practice. For example:
The nurse is a care provider. Nurses help each person achieve the maximum level of wellness possible. In some cases, clients will achieve total wellness; in others, compromises must be made.
The nurse is an advocate. Nurses serve this important role by ensuring that clients receive necessary care, and by intervening when necessary. Nurses help clients understand their rights and responsibilities. They explain details about procedures, so clients are able to give informed consent.
TABLE 2-2. Theories of Nursing
|
THEORIST |
MODEL |
CONCEPTS |
|
Florence Nightingale (1859) |
Natural-Healing |
Nature alone cures. Nursing assists the person to an improved condition for nature to take its course. Health is "freedom from disease.” |
|
Virginia Henderson (1955) |
Independent-Functioning |
Mind and body are one. Nursing’s role is to assist clients to perform functions they would perform unaided if they had the necessary strength, will, or knowledge. Functions vital to health are the ability to breathe normally, eat/drink adequately, eliminate wastes, move/position oneself, sleep, dress, maintain body temperature, maintain hygiene, and keep the skin intact. Safety, communication, worship, work, recreation, and learning are individualized. Health is the ability to function independently. |
|
Dorothea Orem (1958) |
Self-Care |
Building on Maslow’s "Hierarchy of Human Needs”, nursing assists clients to meet self-care needs necessary to maintain life, health, and well-being. Health is the ability to meet self-care needs, which are physiologic, psychological, and sociologic. |
|
Sister Callista Roy (1964) |
Adaptation |
An individual’s state of health/illness moves back and forth on a continuum.Nursing focuses on the body, mind, spirit, and emotion and emphasis is on holistic healing, rather than curing. Each person’s health status fluctuates because humans are constantly interacting in a dynamic (changing) environment. |
|
Betty Neuman (1972) |
Systems |
Humans deal with forces in both internal and external environments. The goal of the whole person is stability and harmony. Health is "relative” in terms of psychological, sociocultural, developmental, and physiologic factors. |
FIGURE 2-2 • The roles of the nurse include, but are not limited to, care provider; communicator; teacher; advocate, leader; and team member
The nurse is a communicator. The nurse documents client care and the client’s response. Professional nurses write care plans with input from other healthcare staff mem-bers—much of the staff uses this important plan. Nurses record information in daily flow sheets or nursing notes, record medications and treatments, and communicate with other healthcare team members in daily reports and team meetings to maintain continuity of care.
The nurse is a team member. Nurses work cooperatively with other healthcare professionals to provide the best care possible.
The nurse is a teacher. Professional nurses write teaching plans and assist people in preventing illness and injury before they occur. Other members of the healthcare team assist with teaching as well. Together, the healthcare team teaches clients and families about illness, surgical procedures, performed tests, and home care. Clients learn about medications, when and how to take them, expected side effects, and possible adverse reactions. Many nurses teach prenatal classes and assist with labor and delivery, providing encouragement and support during childbirth. Later, they often teach new mothers important self-care as well as care measures for the baby.
The nurse is a leader. Nurses must work with clients to motivate them to achieve important goals. Leadership is power, and nurses can use their skills to direct that power for improvement, not only in their clients’ health, but also in the facilities in which they work, the community, and for the entire healthcare system.
Key Concept Always practice nursing ethically When you recite your pledge at graduation, you are promising to abide by this code.
BOX 2-3.
Projecting the Image of a Nurse
|
« |
Show respect for others, including your clients, your instructors, and the staff at your clinical sites. |
|
« |
Follow general practices of good grooming and hygiene: bathe/shower daily, use deodorant, brush teeth, avoid bad breath (especially if you smoke). |
|
« |
Keep hair clean, pulled away from the face, and off the neck. |
|
« |
Wear a minimum of jewelry—it can harbor microorganisms and could injure a client. |
|
« |
Clients may act out—protect yourself by keeping your hair short or pinned up, and avoiding large earrings, neckties, and necklaces. |
|
« |
Keep moustaches and beards neatly trimmed. |
|
« |
Avoid aftershave, cologne, and perfume. Clients may be allergic to them. |
|
« |
Use a minimum of makeup. Artificial nails may not be permitted (Centers for Disease Control and Prevention [CDC] recommendation). |
|
« |
Wash hands often. Make sure fingernails are short and clean. Clip hangnails. Nail polish is not recommended. |
|
« |
Cover cuts or open wounds for your protection. |
|
« |
Wear washable clothes/uniforms and sweaters. |
|
« |
Wear pants long enough to reach your shoe tops. |
|
« |
Keep skirts long and loose enough so you can bend and lift without embarrassment. |
|
« |
Wear safe and comfortable shoes. Most facilities do not allow sandals or clogs. |
|
« |
Always wear your nametag—it is part of your uniform. |
|
« |
Follow guidelines for maintaining optimal health. |
|
« |
Follow any additional guidelines specified by your school or clinical facility |
The Nurse’s Image
Today’s society is filled with information about leading a healthier lifestyle. Many people are working to change their behaviors to restore or maintain good health.
As a nursing student and as a nurse, you need to project a professional image. Remember that you represent not only yourself to the public, but also your school, the healthcare facility for which you work, and the entire healthcare system.
Your nursing program will give you specific guidelines to follow regarding style of dress and grooming when you conduct clinical nursing practice. Box 2-3 identifies some general considerations to help you project the image of the nurse. Remember that many of the measures listed in Box 2-3 are important not only to project a professional image, but also to maintain maximal levels of safety, hygiene, and protection for you and your clients.
Today’s Nursing Student
Many of today’s nursing students are returning to school after several years outside education. You may be one of these adult learners, who has entered a nursing program with the additional responsibilities of a home, family, and outside job. Adult learners may need to master new skills in addition to learning their nursing skills. For example, some adult learners have not worked much with computers, email, or the Internet. All students, and especially those with multiple responsibilities, must plan a schedule that provides ample time for classes, household duties, studying, work, family, and personal time. Managing all of these responsibilities will be a challenge, but the rewards can be great.