Learning Objectives
1. Define and identify the purposes of a nursing diagnosis. Differentiate the legal, licensing, and appropriateness of an RN initiating a nursing diagnosis for the nursing care plan.
2. Differentiate a nursing diagnosis from a medical diagnosis.
3. Discuss the rationale for use of the accepted NANDA-I-approved nursing diagnoses.
4. Identify the three segments of a diagnostic statement and give examples of a comprehensive diagnostic statement.
5. Discuss the following components of planning nursing care: setting priorities, establishing outcomes, and implementing nursing interventions.
6. Define and discuss the rationale for using both short term goals and long-term goals in the development of a nursing care plan.
7. Discuss the uses for each method of care plan development and how all of these methods can be used collaboratively to plan nursing care of a client.
8. Demonstrate examples of written or electronic nursing care plans using the computer printout method, standardized care plan, and a formal written, individualized care plan.
|
IMPORTANT TERMINOLOGY |
|
|
collaborative problem long-term objective |
planning |
|
expected outcome medical diagnosis |
prognosis |
|
Kardex nursing diagnosis |
short-term objective |
|
Acronyms |
|
|
AEB |
NANDA-I |
|
NANDA |
R/T |
The first step of the nursing process is data collection, or the nursing assessment. Standing alone, the data gathered are useless until you determine what they mean. The second step of the nursing process is identifying the nursing care problem—otherwise called the nursing diagnosis—based on your analysis of the data. Only then can you move on to the third step of the nursing process, which is planning client care based on the problems or diagnoses you have identified.
NURSING DIAGNOSIS
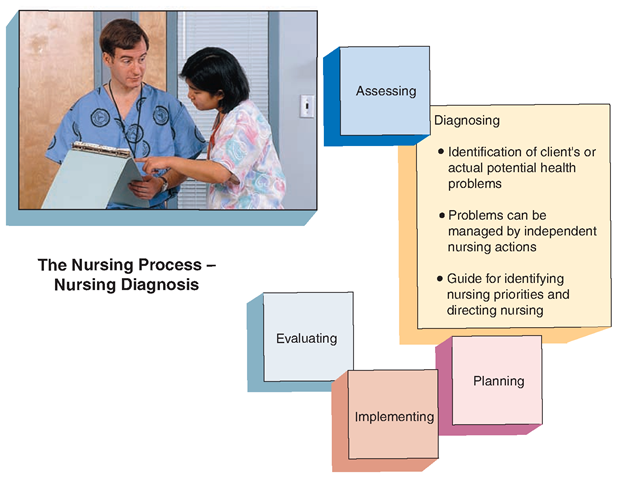
A nursing diagnosis is a statement about the actual or potential health concerns of the client that can be managed through independent nursing interventions (Fig. 35-1). Nursing diagnoses are concise, clear, client-centered, and client-specific statements.
In some areas, practical/vocational nurses do not make nursing diagnoses; it is considered the duty of the RN. Keep in mind that a nursing diagnosis is an approved label that identifies the client’s problems in nursing terminology. Whether or not you make a nursing diagnosis yourself or this step is considered the providence of the RN, all nurses must understand the meaning of a nursing diagnosis and how it is used to plan and to implement nursing care.
HISTORY OF NURSING DIAGNOSES
Since 1973, a group of nurse researchers and educators formulated plans to standardize communication and categories of nursing care. Before this standardization, descriptions of nursing care differed both between hospitals and also within one hospital because nurses literally invented their own descriptions of nursing-related concerns for clients. In 1982, with members from Canada and the United States, the group became known as the organization North American Nursing Diagnosis Association (NANDA). In 2002, the organization was revised and became NANDA-I International (NANDA-I) using an updated model of health called Taxonomy II.
FIGURE 35-1 · In the second step of the nursing process, nursing diagnoses are developed based on analysis of the data collected during nursing assessment.
Standardization of nursing terminology has become a highly effective nursing tool for communication of clients’ problems and concerns. The nomenclature, criteria, and categories developed by NANDA are commonly referred to as nursing diagnoses. In the past decades, NANDA has provided updated terminology and revised categories every 2 years. Subjective and objective data, which nurses collect to communicate effective nursing care for all types of clients, became more understandable as it was adapted by all nursing units at the various types of clinical facilities. NANDA-I’s terminology is now the basis for accepted nursing diagnoses and is a required facet of nursing care by multiple accrediting agencies.
The words, phrases, and/or terms of NANDA-I’s nursing diagnoses are actually the diagnostic labels or categories on which an evidence-based, client-oriented nursing diagnosis statement is built. The wording of the phrases is divided into three specific components. These components start with a general concept and add clarification of the concept to individualize the total phrase. The result is standardized, generalized communication, which also becomes a unique description of a client’s problem or concern. The nursing process uses these nursing diagnoses as part of the fundamental steps involved in the concepts of critical thinking.
Most healthcare facilities have their specific version of the current NANDA-I list posted in a central location or in the medical information system for all nurses to use. Again, please refer to the 2010 NCLEX-I list. The list is updated every few years, but remains a basic foundation of nursing diagnoses.
Nursing Diagnosis Versus Medical Diagnosis
Nursing diagnosis is not to be confused with medical diagnosis. You are probably more familiar with medical diagnoses. Remember these facts about a medical diagnosis:
• It identifies the disease a person has or is believed to have.
• Physicians arrive at a medical diagnosis by studying the physiologic manifestations of the illness and establishing its cause and nature.
• A medical diagnosis provides a basis for prognosis (projected client outcome) and medical treatment decisions.
Medicine clearly emphasizes the disease process. Hypertension, pneumonia, diabetes mellitus, and renal failure are examples of medical diagnoses. Nursing, however, focuses on the person—the individual’s response to his or her health. Nursing asks how a disease or illness influences an individual’s functioning and how his or her needs can be met.
Her medical diagnosis is pneumonia. When you look at the data that have been obtained about the client, you are concerned about how she is functioning and what you can do to help her to improve or to adapt. From the assessment data, you determine that the client has abnormal breath sounds, a cough with thick yellow sputum, increased respirations, difficulty breathing, fever, and fatigue. After analyzing the data, problems involving the client’s airway (respiratory tract) and activity emerge as the priorities.
Purposes of the Nursing Diagnosis
The nursing diagnosis serves the following purposes:
• Identifies nursing priorities
• Directs nursing interventions to meet the client’s high-priority needs
• Provides a common language and forms a basis for communication and understanding between nursing professionals and the healthcare team
• Guides the formulation of expected outcomes for quality assurance requirements of third-party payers
• Provides a basis of evaluation to determine if nursing care was beneficial to the client and cost effective
• Is of help when making staff assignments
The Diagnostic Statement
This section provides an overall look at two ways of writing the diagnostic statement. A more detailed description of each component follows. During the assessment/data collection component of the nursing process, it is likely to find that the client may present with more than one problem. Therefore, the nursing care plan may be made up of multiple diagnostic statements. Each diagnostic statement has two or three parts. The formal NANDA-I definitions for each part of the statement/nursing diagnosis can be fairly lengthy and beyond the purpose of this topic.Therefore, this topic provides an abbreviated description of each component.
The three-part nursing diagnostic statement consists of the following components:
• Problem: general label (e.g., airway clearance, ineffective)
• Etiology: specific, related factors such as excessive mucus or foreign body obstruction
• Signs and symptoms: specific, defining characteristics, such as shortness of breath on exertion or abnormal lung sounds (crackles, wheezes, rhonchi), or ineffective cough
Sample Nursing Diagnostic Statement. Airway clearance is ineffective related to excessive mucus production as manifested by shortness of breath on exertion.
A two-part diagnostic statement consists of the problem and signs and symptoms.
Sample Nursing Diagnostic Statement. Airway clearance is ineffective manifested by shortness of breath on exertion.
Problem
The problem portion of a statement describes—clearly and concisely—a health problem a client is having. Use one of the NANDA-I-approved nursing diagnostic labels to state the problem.
Recall the example from Nursing Care Plan 33-1.After assessing the client and taking the steps leading up to the diagnostic statement, you determine that one of the client’s problems is difficulty breathing because her airway is filled with mucus. Following the NANDA-I guidelines and stating the problem concisely, you state “Ineffective Airway Clearance.” This diagnostic label of a problem is the first part of the diagnostic statement. (For alphabetical purposes, the diagnosis may be seen and written as “airway clearance, ineffective.”)
Key Concept Writing nursing care plans is a process that continually evolves. It is important that the contemporary nurse document according to his or her licensure limitations and within the guidelines of the employing institution.
Etiology
The etiology part of the diagnostic statement is the cause of the problem. Etiology may be physiologic, pathophysiologic, psychological, sociologic, spiritual, or environmental. For the woman with pneumonia, the etiology for the problem “Ineffective Airway Clearance” consists of the physiologic effects of pneumonia. As a nurse, you will know the pathophysiology, that is, the disease process, of pneumonia.
Signs and Symptoms
Data collected during the nursing assessment point to the nursing diagnosis. The third part of the diagnostic statement summarizes these data. You may need to include several signs and symptoms (remember the clusters). For instance, the client with pneumonia had cough with thick sputum, abnormal breath sounds, increased respirations (tachypnea), and difficulty breathing (dyspnea). For her, the third part of the statement would be “increased sputum, coughing, abnormal breath sounds, tachypnea, and dyspnea.” Refer to In Practice, the Nursing Care Plan, 33-1.
Key Concept A nursing diagnosis has three components:
P—problem (diagnostic label) E—etiology (cause)
S—signs and symptoms
Writing the Diagnostic Statement
The diagnostic statement connects problem, etiology, and signs and symptoms. The first two parts of the statement are linked by “related to,” sometimes abbreviated R/T. The last two parts are linked by “as evidenced by,” sometimes abbreviated AEB. Therefore, the statement for the client with pneumonia described in Nursing Care Plan 33-1:
Ineffective Airway Clearance related to physiologic effects of pneumonia as evidenced by increased sputum, coughing, abnormal breath sounds, tachypnea, and dyspnea.
When formulating a nursing diagnosis, make sure that it is something the nursing staff and the client can treat without orders from the physician. Such actions are called independent nursing actions. If treatment requires something you cannot do, such as prescribe medication for the cough, the problem is a collaborative problem. A collaborative problem means that you will work together with the physician or other healthcare providers. For instance, the physician will prescribe the medication, but the nurse will decide whether or not to administer a PRN (as needed) medication at bedtime.
Key Concept The nursing diagnosis is a statement about the client’s actual or potential health concerns that can be managed through independent nursing interventions. It contains the following steps:
• Establishing significant data
• Writing a two- or three-part diagnostic statement
PLANNING CARE
After identifying the nursing diagnoses, you begin planning nursing care. Planning is the development of goals to prevent, reduce, or eliminate problems and to identify nursing interventions that will assist clients in meeting these goals. Setting priorities, establishing expected outcomes, and selecting nursing interventions result in a plan of nursing care (Fig. 35-2).
NCLEX Alert Nursing priorities on NCLEX questions are written keeping the form of the diagnostic statement (i.e., problem, etiology, and signs and symptoms). LPN/LVNs and RNs must be aware of these concepts as they are used throughout their nursing careers.
Setting Priorities
Because some diagnoses have a higher priority than others, they are more important. Nursing diagnoses are ranked in order of importance. Survival needs or imminent life-threatening problems take the highest priority.For example, the needs for air, water, and food are survival needs. Nursing diagnostic categories that reflect these high-priority needs include Ineffective Airway Clearance and Deficient Fluid Volume. Safety needs are the next priority, with nursing diagnostic categories such as Risk for Injury or Risk for Suffocation. At a lower level of priority are the social and psychological needs for love, self-esteem, companionship, and fulfillment; some possible nursing diagnostic categories are Ineffective Role Performance, Anxiety, and Social Isolation.
The reason for the client’s admission to your facility is the most important concern; however, it may not be a priority nursing concern at any given moment. The client may have a number of nursing diagnoses that are unrelated to the primary care problem. Attempts to treat them may be unsuccessful because the client has more urgent, immediate needs. These other problems can be deferred until a later time.
In addition, materials and human resources availability, as well as time limitations, affect the order of priority. Equipment, supplies, and staff must be available. Keep in mind that you cannot treat every nursing diagnosis that a client may have.
The client also determines the priority of health concerns. For example, a smoker may be fully aware of the health risks of smoking, but may choose to continue. In this case, plans to help the client quit smoking will fail, even though the need for oxygen is a requirement for survival, and thus, is a high priority.
Establishing Expected Outcomes
You are familiar with learning objectives or behavioral objectives in your nursing program. A similar type of objective or outcome is established for the client. An expected outcome is a measurable client behavior that indicates whether the person has achieved the expected benefit of nursing care. It may also be called a goal or objective. An expected outcome has the following characteristics:
Client-oriented: The client, not the nurse, is expected to meet this outcome. For instance, “the client will walk around the room at least once per shift.”
FIGURE 35-2 · During planning, the third step of the nursing process, goals are established and interventions are identified to assist the client in meeting the goals.
BOX 35-1. Examples of Verbs Used in Expected Outcome Statements
|
cough |
perform |
|
demonstrate |
relate |
|
describe |
share |
|
discuss |
sit |
|
express |
stand |
|
has a decrease in |
state |
|
has an absence of |
use |
|
has an increase in |
verbalize |
|
identify |
walk |
|
list |
Specific: Everyone, including the client, knows what is to occur. For instance, “the client will walk up and down the hall for 5 minutes.”
Reasonable: The outcome should be within the client’s capacity and abilities, considering the confines of his or her condition. For example, if the client is having trouble breathing, walking may be limited to trips to the bathroom. Measurable: The behavior can be observed and measured. For example, nursing staff can observe a client walking, or the client can state that he or she walked for 5 minutes.
Working together, you and the client should determine outcomes. Box 35-1 gives examples of some verbs commonly used in expected outcome statements.
Expect clients to achieve outcomes in varying lengths of time. A short-term objective is an expected outcome or goal that a client can reasonably meet in a matter of hours or a few days (e.g., “The client will walk for 20 minutes longer each day for the first 3 postoperative days”). A long-term objective is an outcome that the client ultimately hopes to achieve, but which requires a longer period of time to accomplish. Sometimes, the longer period means that the client will not still be in the healthcare facility when the objective is achieved. You can help the client put this objective in writing. Then, while working toward self-care, the client can probably identify the desired long-term goal or objective. He or she can learn how to measure the progress toward achieving the objective. For example, the client’s long-term goal may be “to return to college” after self-care is achieved.
Key Concept Expected outcomes are client oriented, specific, reasonable, and measurable.
NCLEX Alert The correct response on a NCLEX multiple choice question may relate to the ability to know which option is the most specific, measurable, and realistic for the given clinical scenario.