Learning Objectives
1. Explain how the Controlled Substances Act regulates the storage of, and accountability for, specific medications. Describe the proper procedure for monitoring schedule drugs in the healthcare facility.
2. Identify the specific rights of clients as related to prescribed medications.
3. List sources of drug information for nurses, both in print and online.
4. Define what is meant by chemical, generic, official, and trade or brand names when referring to medications. State which of these are most commonly used.
5. Describe the formats for oral medications.
6. List and describe the different routes of medication administration.
7. Discuss the factors that influence the dosage of any specific medication.
8. Differentiate between prescribed and over-the-counter medications.
9. List the required components of a prescription.
|
IMPORTANT TERMINOLOGY |
||
|
agonist |
injectable |
prescription |
|
antagonist |
interaction |
sublingual |
|
brand name |
legend drug |
synergistic |
|
caplet |
medication |
tablet |
|
capsule |
official name |
topical |
|
chemical name |
oral |
trade name |
|
dosage |
paradoxical |
transdermal |
|
enteric-coated |
pharmacokinetics |
translingual |
|
generic name |
pharmacology |
transmucosal |
|
inhalant |
potentiating |
troche |
|
Acronyms |
|
|
DEA |
PHARM D |
|
DR |
RPh |
|
ER |
SR |
|
FDA |
TD |
|
IR |
TORB |
|
MDI |
USD |
|
NF |
USP |
|
ODT |
VORB |
|
OTC |
XR |
|
PDR |
|
A medication is a medicinal agent that modifies body functions. A medicine or drug is any substance(s) used to prevent disease or pregnancy, aid in the diagnosis and treatment of disease, and restore or maintain bodily functions. Pharmacology is the science that deals with the origin, nature, chemistry, effects, and uses of medications.
A Doctor of Pharmacy (Pharm D) or Registered Pharmacist (RPh) are healthcare professional who is licensed to prepare and dispense medications on the order of a licensed practitioner of medicine. Medication orders can legally be written by a physician (Doctor of Medicine [MD] or Doctor of Osteopathy [DO]), a dentist (Doctor of Dental Surgery [DDS] or Doctor of Medical Dentistry [DMD]), or a veterinarian (Doctor of Veterinary Medicine [DVM]), and, in many states, by a physician’s assistant (PA). Specialized nurses can also legally write prescriptions in many states. These include an advanced practice nurse or nurse practitioner (NP), certified registered nurse anesthetist (CRNA), or certified nurse midwife (CNM). This topic provides an introduction to the basics of pharmacology. It presents general information concerning medications that is important throughout a nurse’s career.
The primary nursing obligation is to “do no harm,” especially when administering medications. Thus, a general knowledge of pharmacology is essential. Because in the current healthcare delivery system, clients must take more responsibility for their own healthcare, nurses often bear most of the responsibility for teaching them about their medications. Teaching should include the desired effects, methods of administration, actions, and possible adverse reactions or side effects of the client’s medications.
Key Concept An important part of nursing practice is teaching clients about the desired effect and possible side effects of medications prescribed for them. Documentation of teaching and the client’s response to instruction verifies that teaching did, in fact, take place and that the client understands his or her medication regimen.
NCLEX Alert It will be important for you to understand the nurses responsibility for teaching clients about their medications because this information may be integrated into NCLEX examination questions.
LEGAL ASPECTS
Federal Drug Standards
The U.S. Food and Drug Administration (FDA) operates under the enforcement of the U.S. Department of Health and Human Services. Its Canadian counterpart is Health Canada (Santé Canada), which is a part of the Health Products and Food Branch (HPFB) of the government. These agencies ensure that medications and therapeutic agents are safe and effective for public use before they are released on the market. Standards of strength and purity are essential to protect the public against the dangers of impure, inferior, or misused substances. For example, in 1998, terfenadine (Seldane), a histamine antagonist, was removed from the market, and, in 2000, troglitazone (Rezulin), an oral antihy-perglycemic agent, was removed. In 2004, rofecoxib (Vioxx), a medication used to treat osteoarthritis pain, was removed. Although these medications seemed to be effective, their side effects were so serious that they were deemed unsafe for use. (In some cases, a drug that is not marketed in the United States is still marketed in other parts of the world.) The FDA and Health Canada are constantly doing research to ensure the efficacy and safety of medications on the market.
Nursing Alert In some cases, it is dangerous to obtain medications from other countries, because some countries do not have the stringent safety precautions of the United States and Canada.
National publications in the United States that define standards for medication approval are the United States Pharmacopeia (USP) and the National Formulary (NF). These publications are used primarily by pharmacists and primary care providers. Other countries have similar publications.
Controlled Substances
The Comprehensive Drug Abuse Prevention and Control Act, passed by the U.S. Congress in May 1970, is commonly referred to as the “Controlled Substances Act.” This federal law, enforced by the Drug Enforcement Agency (DEA), regulates the manufacture, prescription, and distribution of psychoactive medications, including narcotics, depressants, stimulants, and hallucinogens. There are five classifications, or “schedules,” of controlled substances. The degree of control depends on the medication’s classification, which ranges from Schedule I (has a high potential for abuse) to Schedule V (a relatively low potential for abuse) (Box 61-1). A similar schedule has been established in Canada by the National Drug Scheduling Advisory Committee.
BOX 61-1. Schedule of Controlled Substances
Controlled substances (schedule drugs) are classified on the following basis:
♦ Schedule I (C-I): High potential for abuse; no accepted medical use (e.g., heroin, LSD; not kept in healthcare facilities or pharmacies)
♦ Schedule II (C-II): High potential for abuse; severe dependence liability (e.g., narcotics, amphetamines, and some barbiturates)
♦ Schedule III (C-III): Lower potential for abuse than Schedule II drugs; moderate dependence liability (e.g., anabolic steroids, nonbarbiturate sedatives, nonamphetamine stimulants, limited amounts of certain narcotics)
♦ Schedule IV (C-IV): Lower potential for abuse than Schedule III drugs; limited dependence liability (e.g., some sedatives, antianxiety agents, nonnarcotic analgesics)
♦ Schedule V (C-V): Limited potential for abuse; primarily small amounts of narcotics (e.g., codeine) used as antitussives and antidiarrheals.
Protection of Controlled Substances. Controlled substances must be managed carefully, and an accurate inventory and dispensing record must be kept. In a healthcare facility or pharmacy, controlled substances must be kept in a double-locked area. This may be a locked medication room or cart with a separate locked “narcotics cabinet.” The keys must be in a licensed nurse’s possession at all times or access must be controlled electronically. Only licensed nurses are allowed to access schedule drugs. Each healthcare facility incorporates the use of specialized forms or computer documentation for the use of controlled substances. These forms verify the client’s name, medication name, dose, time of administration, and the signature or personal identification number (PIN) of the licensed nurse who administered it. In some cases, the name of the prescribing person is also listed. Schedule drugs must be documented in the client’s record within 5 minutes of administration.
Most acute care facilities use some sort of computerized dispensing unit (Fig. 61-1). This unit dispenses and keeps records of controlled substances and other medications. Medications are accessible only with the entry of a PIN assigned to each individual nurse. In this way, there is a computerized record of each medication removed from the machine, as well as the client for whom it was signed out, the nurse, the time and date, and the amount of medication remaining.
FIGURE 61-1 · A computerized medication dispensing cabinet called the OmniRx One-Cell, with Omni dispenser module. It records information about medications dispensed and counts schedule medications. Discrepancies are resolved/witnessed by two licensed nurses. On the right is a secure container for returning unopened narcotics and other medications. The lower area can be a refrigerator or shelving.
Controlled Drug Count Verification. To ensure that schedule drugs are properly controlled, all counts must correspond with documentation. If there is a locked narcotics cabinet, two licensed nurses, one going off duty and the other coming on duty, review the documentation and count the number of remaining controlled medications. (The oncoming nurse counts; the outgoing nurse records. This assures the oncoming nurse that all the drugs are there.) The documentation must match the number of remaining medications in the controlled substances cabinet. If the count does not agree, no one is allowed to leave the unit until a search is undertaken or the discrepancy is resolved. If narcotics are dispensed by a computerized system, a visual count may be required once a day. This may be done by pharmacy staff and is done during the night or when they refill the machine. Documentation regarding schedule drugs and other drugs in the machine downloads to the pharmacy at least every 24 hours. In addition, pharmacy computers can access the inventories in the machines at any time.
In many cases, even though there is a dispensing machine, a separate narcotics cabinet is in place for unusual medications. In this case, the keys to the narcotics cabinet are locked in the machine and can only be accessed by authorized personnel, using a PIN number. Medications kept in this cabinet are counted each shift.
If there is no medication dispensing machine, the narcotic keys should be in the possession of the nurse to whom they have been assigned. The keys are not to leave the unit at any time. In the event a nurse forgets to give the narcotic keys to the oncoming nurse and takes the keys out of the healthcare facility, he or she must return the keys immediately when realizing the error. In addition, the locks to the narcotic cabinet containing controlled medications may need to be changed and new keys assigned.
Key Concept Nursing students usually do not give schedule medications without direct supervision by the instructor
When additional controlled drugs are brought to the nursing unit, only a licensed nurse or pharmacy representative is allowed to add them to the inventory, whether using a narcotics cabinet or machine. In some facilities, two nurses must perform this procedure. A record is signed by the nurse and verified by the pharmacist to ensure that all the medications were, in fact, added to the unit inventory. If schedule medications are sent to the nursing unit by pneumatic tube, they must be sent in “secure” mode and can be accessed only using special codes.
NCLEX Alert To administer medications safely you need to be alert to concepts presented in this topic— uses of medications, reasons for establishing medication standards, factors affecting a client’s reaction to a medication, and the rights of clients related to taking medications. During the examination, you may need to demonstrate your knowledge and understanding of these concepts.
Client Rights
Clients have the right to know the name, action, and possible side effects of medications administered to them. They also have the right to refuse to take medications, unless a court order gives healthcare workers the right to administer medications without the client’s consent. (If clients are endangering themselves or others, medications may be given against their will.) Clients also have the right to request the generic form of prescribed medications, if available. Generic forms of medications are often less expensive than their brand name counterparts.
Drug References
Many references that provide detailed information about medications are available to healthcare professionals. These references are valuable tools for learning about the classification, use, abuse, desired actions, recommended dosage, and adverse actions of medications.
The Physician’s Desk Reference (PDR) is published annually in the United States, with quarterly updates. This recognized source contains extensive information concerning therapeutic dosages, expected therapeutic effects, possible side effects, contraindications, drug interactions, and FDA pregnancy categories (levels of danger to a fetus). The PDR contains a number of sections, including the product identification section and the product information section. This reference also contains a list of poison control centers and a guide to managing overdose. A companion handbook for nurses is available, as is an online version. A list of drugs removed from the PDR Nurse’s Drug Handbook is archived on the Internet yearly.
Nursing Alert The emergency telephone number for poison control centers in the United States and U.S. Territories is: 1-800-222-1222. The numbers vary by province in Canada. Note: these telephone numbers are to be used for emergencies only
Facts and Comparisons, another drug reference, lists medications under the following classifications: nutritional products, blood modifiers, hormones, diuretics, cardiovascular drugs, autonomic drugs, central nervous system drugs, gastrointestinal drugs, anti-infectives, and biologicals. This resource, which many pharmacies use, is updated monthly and provides the most current printed medication information available.
The United States Dispensatory (USD) lists official and unofficial names of internationally existing and discontinued medications. The United States Pharmacopeia and the National Formulary identify the official names of medications used in the United States.These sources are designed to meet the needs of nursing students and practicing licensed nurses. They incorporate nursing considerations in addition to mechanisms of action, uses, contraindications, precautions, dosages, preparations, interactions, pharmacokinetics (actions of drugs), side effects, and treatments of overdose. They also emphasize client and family teaching. In addition to the above sources, much information about medications is available at various Internet Websites (see Web Resources on thePoint).
Nursing Considerations
When a client is admitted to a healthcare facility, initial assessment must include a detailed medication history. Information must be obtained from the client and family, as well as from the client’s pharmacy and/or personal healthcare provider. In addition, any medications brought in by the client must be catalogued and kept in a safe location. Each facility has a specific protocol for this.
It is vital to identify and indicate in the client record any client allergies and what adverse reaction is caused by each medication. This information will enable the primary provider to decide which medications are safe and effective for this client. All clients wear an allergy wristband that either identifies allergies or notes the client has no known allergies. This verifies that the allergy assessment has been done.
Nursing Alert Some adverse reactions to medications are not considered true allergies. True allergies are differentiated from other adverse reactions by the primary healthcare provider. A pharmacist is a good source of information if there are any questions about drug interactions or allergic responses. A client usually does not experience an adverse or allergic reaction on first exposure to a medication. Therefore, stay alert for adverse reactions, even if the client has received the medication previously
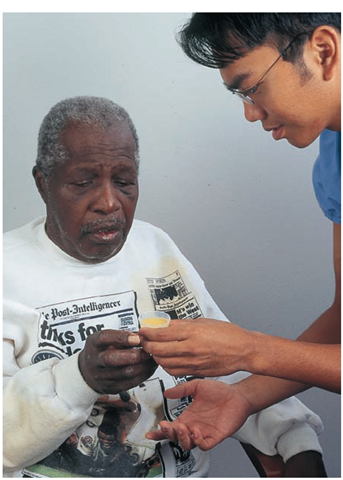
Before administering any medication, the nurse must know about the medication (Fig. 61-2). Before administering a medication, be sure to confirm the client has not had a previous adverse or allergic reaction to it. Failure to do so may jeopardize the client’s well-being and may even be fatal.
Key Concept Nurses are obligated to know the generic and common trade name, classification, use, recommended dosage, desired effects, possible adverse or untoward effects, and route of administration of any medication administered. Should a client experience an adverse reaction that the nurse does not recognize (and thus fails to institute the appropriate action for), a medication error has been committed, just as if the wrong medication had been given.
FIGURE 61-2 · A nursing student or licensed nurse is responsible for knowing vital information about medications the client is receiving.