INFLAMMATORY DISORDERS
Vulvitis
Vulvitis, inflammation of the vulva, may result from trauma caused by scratching, improper cleansing, birth control pills, or irritating vaginal discharge. Most often, its cause is some type of infection. Common signs and symptoms include severe itching and burning; pain during urination, defecation, or intercourse; and swelling and redness. The goal of treatment is to determine and eliminate the cause.
Vaginitis
Vaginitis is inflammation of the vagina. Normally, vaginal secretions protect against infection. However, two organisms often cause vaginal infection: Trichomonas vaginalis or trichomoniasis and Candida albicans or candidiasis (formerly known as monilia; commonly known as yeast infection). Trichomoniasis, which is caused by protozoa, is likely to be transmitted sexually, whereas candidiasis, which is caused by fungus, is more easily spread in other ways. However, both are considered sexually transmitted infections (STIs). Many STIs cause inflammation.
IN PRACTICE :IMPORTANT MEDICATIONS 91-2
FOR VAGINAL INFECTIONS
Trichomonas and Bacterial Vaginosis
• metronidazole (Flagyl)
Candidiasis
• nystatin (Mycostatin, Nilstat)
• miconazole nitrate (Monistat, Micatin)
The most prominent symptom of vaginitis is a whitish vaginal discharge called leukorrhea. The discharge is odorous and profuse (more so in trichomoniasis), causing burning and itching in the perineum, vagina, and urethral area. In trichomoniasis the discharge is foul-smelling, and greenish-yellow or gray. With candidiasis, the discharge is white and cottage cheese-like. The sexual partner must be treated at the same time so that the infection will not be spread back and forth (see In Practice: Important Medications 91-2). Circumcision of the male may be necessary to help control a recurring infection.
Vaginitis can be difficult to cure. It can be extremely irritating and persist for a long time. Recurrence is fairly common. Early and persistent treatment is the only way to prevent this disorder from becoming chronic. The client may find that wearing sanitary napkins is necessary to absorb the profuse drainage. Frequent napkin replacement, perineal care, and sitz baths will help prevent odor and irritation. Sometimes, mild antianxiety agents or analgesics lessen the effects of pruritus (itching).
Nursing Alert If a pregnant woman contracts trichomoniasis, treatment is necessary although it can be postponed until the second or third trimester because of the unknown effects of the drug on the developing fetus. Untreated trichomoniasis can lead to a fragile cervix that will be unable to maintain pregnancy or withstand delivery
Nursing Considerations
Frequent bathing provides temporary relief from irritation and itching. Over-the-counter medications, such as nystatin (Mycostatin, Nilstat) and miconazole nitrate (Monistat, Micatin), are available. These medications are supplied in various systems of delivery, including creams with several different types of applicators, tablets that dissolve inside the body, and suppositories. A combination pack containing suppositories and cream is available to treat internal and external symptoms.
Teaching is particularly important because many women will treat their own infections at home and may not see a healthcare provider. Instructions are basically the same in all treatment systems (see In Practice: Educating the Client 91-4).
Women who are treating a vaginal infection should consult their primary care provider when there is:
• No sign of improvement after 3 days of treatment
• Worsening of symptoms within 3 days
IN PRACTICE: EDUCATING THE CLIENT 91-4
SELF-CARE WITH A YEAST INFECTION
• Read and follow the instructions on the medication package carefully.
• Insert the full dosage of medication.
• Use cream during the day to control external itching.
• Use the treatment for specified consecutive days.
• Do not skip treatment during menses.
• Refrain from sexual intercourse during treatment and for at least 3 days after treatment is completed.
• Remember that a condom or diaphragm used during treatment will not be effective to prevent pregnancy because the medication weakens latex.
• Use only unscented sanitary napkins during treatment.
• Do not use tampons during treatment because they absorb some medication, reducing the dosage, and can be irritating.
• No relief of symptoms after 7 days of treatment
• Return of symptoms within 2 months
The latter cases indicate the presence of an infection or condition other than candidiasis.
Atrophic (Senile) Vaginitis. Atrophic vaginitis often occurs in postmenopausal women. It is caused by atrophy of the vaginal mucous membranes and decreased mucus and other vaginal secretions, resulting from lowered estrogen production.
Atrophic vaginitis is treated by using a water-soluble lubricant (e.g., K-Y jelly) during intercourse. An estrogen-based cream also may be helpful.
Cervicitis
Several organisms cause cervicitis (inflammation of the cervix), notably Staphylococcus, Streptococcus, and Gonococcus. Cervicitis is often diagnosed after childbirth because of trauma to, and sometimes tearing of, the cervix. It also can be related to frequent douching, STIs, or a forgotten tampon. Cervicitis also may result from continued use of contraceptive foams or jellies. The main symptoms are leukorrhea and bleeding. Pain on sexual intercourse also may occur.
Unless cervicitis is treated promptly, it may be difficult to cure. Periodic vaginal examinations help in diagnosis. Antibiotics are the mainstay of treatment. Sometimes the cervix must be cauterized. After cauterization, a watery discharge appears, which may become foul smelling. It takes about 6 to 8 weeks for the area to heal after cauterization. Some precautions taken to prevent vaginal infection also help prevent cervical infection.
Endometriosis
Normally, endometrial tissue is confined to the inside of the uterus. In endometriosis, tissue resembling endometrial tissue appears in various places in the pelvic cavity, such as on the ovaries, oviducts, bladder, intestine, rectum, or pelvic wall. The cause of endometriosis is unknown, but it usually affects women between the ages of 25 and 45 years. There is
IN PRACTICE :IMPORTANT MEDICATIONS 91-3
FOR ENDOMETRIOSIS
• Combination (estrogen-progestin) oral contraceptives
• Progestins
• Synthetic estrogen, danazol (Danocrine, Cyclomen)
• Gonadotropin-releasing hormone agonists (cause lowered estrogen levels):
• leuprolide (Lupron)
• nafarelin acetate (Synarel)
Note: Medications used to treat endometriosis can cause any or all of the following side effects: abdominal swelling, breast tenderness, breakthrough bleeding, atrophic vaginitis, weight gain, edema, hot flashes, emotional lability an especially high incidence in women who have never experienced childbirth.
The client experiences pelvic pain, abnormal uterine or rectal bleeding, symptoms of pelvic pressure, and dysmenorrhea. She also experiences dyspareunia and may possibly be infertile.
Treatment is directed toward symptom relief. Healthcare providers often recommend pregnancy for two reasons. First, endometriosis may eventually result in sterility; and second, because endometriosis is influenced by hormonal changes, symptoms often improve after pregnancy.
If pregnancy is undesirable, medications may shrink the endometrial tissue, thereby decreasing the symptoms (In Practice: Important Medications 91-3). Sometimes, endometriosis recurs when medication is stopped. Extensive and chronic endometriosis may require drastic surgical treatment, such as hysterectomy, salpingectomy (removal of oviducts), and oophorectomy. A woman experiencing endometriosis will require a great deal of emotional support.
Pelvic Inflammatory Disease (PID)
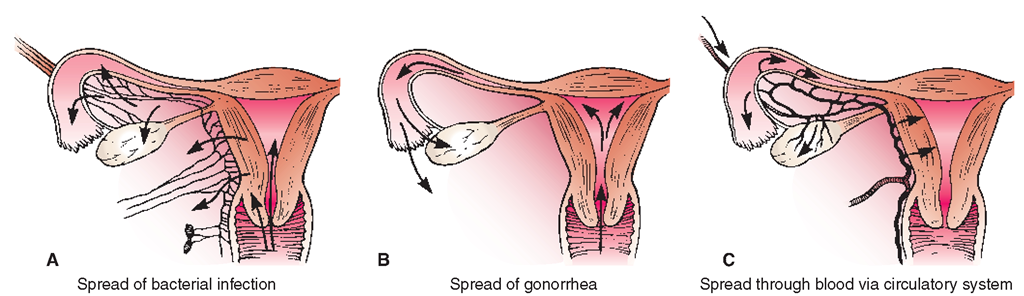
Pelvic inflammatory disease, an infection of the ovaries (oophoritis), oviducts (salpingitis), uterus, or pelvic cavity, enters the body through the vagina, peritoneum, lymphatic system, or bloodstream. Two STIs are the most common cause of PID: Chlamydia trachomatis and Neisseria gonorrhea. Many other STIs and the bacterial strain of Streptococcus may also cause PID. The microorganisms most often pass up through the reproductive tract via the vagina and uterus (Fig. 91-4), which may occur following intercourse, a therapeutic or spontaneous abortion, the insertion of an IUD, douching, or inadequate hygiene during menstruation, especially when tampons or pads are not applied hygienically or are used for lengthy periods of time. The woman who has frequent sexual partners has a higher risk of developing STIs and PID.
Symptoms may be vague, mild, or severe, or the woman can be completely asymptomatic. Commonly, initially noticed symptoms include a foul-smelling vaginal discharge. The client also complains of backache, severe abdominal or pelvic pain, fever, chills, malaise, nausea, and vomiting. Painful urination, painful intercourse, and irregular menstrual bleeding may be noticed. Long-term consequences of PID include chronic pelvic pain, infertility, ectopic pregnancies, abscess formation, sepsis, and death. The reproductive tract, especially the fallopian tubes, can be permanently scarred, leading to chronic PID infections and permanent infertility.
Treatment includes combinations of clinical observations and antibiotics. PID can be caused by more than one organism; thus, combination antibiotic therapy is common. PID caused by the herpes virus is not affected by antibiotics. The sexual partner is also examined and treated, if necessary. Sexual intercourse is discouraged as long as the woman has any trace of infection. The longer the time that PID is not treated, the greater the likelihood of chronic pain and sterility, because of the increasing formation of scar tissue that blocks the oviducts. Pelvic ultrasound or a laparoscopy may be used to confirm diagnosis. No laboratory test can specifically identify PID, but a white blood count is typically elevated in acute infections. Serum pregnancy testing may be ordered (which will not differentiate between normal or ectopic pregnancies).
FIGURE 91-4 · Pathways by which microorganisms enter the pelvis. (A) Bacteria enter through the vagina into the uterus and through the lymph system. (B) Gonorrhea spreads from the vagina into the uterus and into the tubes and ovaries. (C) Bacterial infection may enter the reproductive organs through the bloodstream.
Nursing Alert A woman who has had PID is more likely to have an ectopic pregnancy (a fertilized egg that implants in the fallopian tubes rather than the uterus). An ectopic pregnancy is likely to cause rupture of the fallopian tubes, which results in life-threatening hemorrhage. Treatment of sudden, spontaneous abdominal pain in a reproductive-aged female is an emergency
Nursing Considerations
Antibiotics and pain relief are important nursing concerns. The client hospitalized with PID is commonly placed in the Fowler’s position. Rationale: This position helps encourage pelvic drainage and relief of abdominal pain. Mild heat to the abdomen or sitz baths may be ordered. Rationale: They help relieve pain and promote drainage. Follow Standard Precautions with the disposal of soiled pads and dressings. The healthcare provider may order perineal care for the client after removing the pad and after the client uses the bedpan. Sometimes, an abdominal or perineal abscess forms, and the surgeon institutes drainage through an incision.
During the active disease process, the client should avoid douches and sexual intercourse. Prevention of PID is by sexual abstinence or having a long-term monogamous relationship with an uninfected partner. Correct and consistent use of male latex condoms reduces the transmission of chlamydia and gonorrhea. Teaching and the cooperation of the sexual partner are vital in the treatment of pId.
Vulvodynia
Vulvodynia is chronic vulvar pain. The vulva (or pudendum) consists of the external female genitals, including the labia majora, labia minora, clitoris, the Bartholin’s glands, the vaginal opening, and the vestibule of the vagina. The pain is unexplainable by any known vulvar or vaginal disorder or infection (e.g., PID or STIs). Specific etiology is unknown, but the condition may occur in women who have had chronic moniliasis or who have been on long-term antibiotic therapy. Other factors may include nerve injury or irritation, muscle spasms, allergies, frequent sexual intercourse, oxalates in the urine, or hormonal changes. It can occur in women of any age and of any ethnic background.
Symptoms
Symptoms typically begin suddenly and they include burning (most universal), aching, itching, stinging, irritation, sharp or severe pain when the vulva area is touched, or in the presence of pressure, such as attempted sexual intercourse, sitting, bike riding, or when tampons are inserted. Vulvodynia lasts at least 3 months and can last for years. The pain can be constant, intermittent or happen only when the vulva is touched. On examination, the healthcare provider may find localized erythema and swelling of the vestibule. The emotional impact can be overwhelming because the disorder can severely impair sexual relationships, social interactions, exercise, and employment.
Treatment
Treatment should include a thorough physical examination and emotional history by a healthcare provider who is experienced in women’s healthcare issues. Medications that are most helpful tend to have anti-inflammatory effects, such as NSAIDS. Local application of lidocaine creams may be helpful. Because of the intense impact the disorder has on everyday life, the woman may need to be treated for depression. Additionally, biofeedback and relaxation techniques can reduce the woman’s feeling that things are “out of control.” At home the woman needs to avoid using products that contain chemical irritants, such as scented toilet paper, body soaps, hot tubs, or detergents and fabric softeners. Underwear should be 100% cotton. The client should be taught to cleanse the vulva area with cool water after sex and after urinating, and to avoid activities that put direct pressure on the painful areas (e.g., use pressure-reducing pillows, lie on her side, or lie prone whenever possible). A cool or tepid water sitz bath can be helpful. Either cool packs or warm packs applied to the affected area can be helpful. Over-the-counter lubricants used daily or before sex can be helpful, but some types can contribute to yeast infections. Combinations of treatments tend to have the best results.
Nursing Considerations
The nurse needs to use active listening communication techniques. The client may have the feeling that there is nothing that can be done or that the pain is psychosomatic in origin. The nurse can help the woman review home-based treatments suggested above because the use of many commercial products (e.g., scented tissues or bubble baths) has become so habitual that consequences of their use are not at all considered. Numerous self-help aids are found in In Practice: Educating the Client 91-1.
TRAUMA
Many women are victims of trauma, including battering, automobile accidents, and falls. Many times, this trauma involves the reproductive organs.
Most rape victims are women. Rape may cause physical disorders, including vaginal, cervical, or anal bruising or tearing; tampon impaction; or STIs.
Other trauma can cause various types of injuries to the reproductive organs. These injuries are diagnosed and treated symptomatically, depending on the nature of the injury.
NEOPLASMS
Tumors of the Ovary
Benign Ovarian Tumors
Also known as cysts, these benign growths may form from fluid retained in the ovary or from other causes. Although they usually do not cause any trouble, cysts may enlarge and press on other abdominal organs and cause pain if they rupture or twist.
Malignant Ovarian Tumors
Women who have a personal or family history of cancer have a higher t an average chance of developing ovarian cancer. Cancers that seem the most predictive of ovarian cancer include those of the breast, uterus, colon, and ovary.
If a woman has had a tubal ligation, her chances of ovarian cancer seem to decrease to one third the risk of other women. Some researchers believe this is because carcinogens travel up the oviducts to the ovaries. Vaginal ultrasound and the CA125 blood test can make the diagnosis. Cancer of the ovary often displays no early symptoms and usually is detected only after metastasis has occurred. Ovarian cancer is a fairly frequent cause of death in young women because it is often not discovered in time to provide a long-term cure. Cancer of the ovary is treated surgically. The procedure involves a total abdominal hysterectomy and removal of both tubes and both ovaries. Hormones are not given because they seem to nourish this particular type of cancer cell. Radiation therapy and chemotherapy are usually prescribed after the surgery.
Table 91-1 provides an overview of the major cancers of the female reproductive system.