Fractures, Sprains, and Dislocations
When a person has been involved in an MVA or a fall, look for these possible problems:
• Fracture: broken bone
• Sprain: twisting of a joint with rupture of ligaments and other possible damage
• Strain: twisting or stretching that damages a muscle or tendon
• Dislocation: displacement of a bone from a joint
Sometimes, determining whether a sprain or a fracture has occurred is difficult. If in doubt about the extent of an injury, assume that a fracture has occurred and treat the person accordingly until a definite diagnosis is made. Use ice as treatment for a fracture or sprain until medical assistance is available. Usually the person will have pain on movement or weight-bearing after sustaining a fracture. Do not have the person stand or walk on a suspected fracture to check for pain; doing so is likely to aggravate the injury.
The cardinal rule of emergency care is do not move the person. Get emergency help. Question the person if he or she is conscious. Observe for obviously deformed limbs; cover them with a blanket until you can obtain adequate help. If the person must be moved, the injury should be immobilized.
Never attempt to replace the ends of bones in a fracture, whether or not the skin is broken. (If the fractured ends of the bone protrude through the skin, this is called a compound fracture. If the skin is not broken, this is called a simple fracture.) Cover any open wounds with a sterile dressing and control excessive bleeding by direct or indirect pressure.
Remember the acronym RICE in emergency procedures for sprains and strains:
R = Rest I = Ice
C = Compression (such as with a roller bandage)
E = Elevation (keep the part above the level of the heart, if possible)
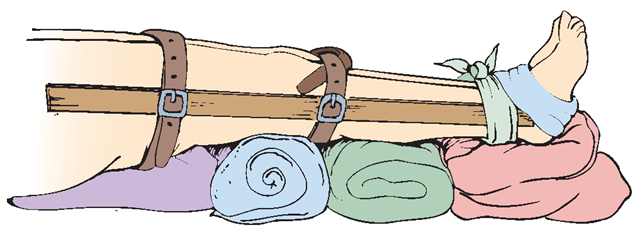
Splinting
A splint is a device applied to immobilize a fracture or sprain. You can use any hard, straight item. However, do not attempt to splint a fracture if emergency medical assistance is available. A good emergency splint for an arm is a magazine wrapped around the arm and tied. Any long, straight item can be used as a temporary splint for a leg (Fig. 43-10). Be careful not to tie the splint so tightly as to cut off circulation to the limb. Numerous commercial splints also are available. Traction splints are best for most major leg fractures and should be applied only by specially trained members of the EMS team. Inflatable splints may also be used.
If a fracture of a wrist, knee, or elbow is suspected, splint the joint in its existing position. Rationale: Because of the joints close proximity to arteries, veins, and nerves, straightening the joint can put pressure on blood vessels, cutting off circulation or sensation to the extremity’s distal portion. An effective splint for a fractured toe is the adjacent toe; tape the digits together (“buddy taping”). The same is true for fingers. An ice cream stick or tongue blade is a handy item to use for a finger splint.
FIGURE 43-10 · An emergency leg splint immobilizes the injured leg to the uninjured leg. The makeshift splint can be made of any rigid item, such as a board, broom handle, or golf club, and tied with neckties or belts. The legs are kept elevated.
Nursing Alert When splinting a fracture, check the person’s distal pulse before and after splinting. An absent pulse is a medical emergency Obtain medical attention immediately.
Dressing a Wound
If emergency assistance is unavailable, it may be necessary to apply a dressing to an open wound, such as that which accompanies a compound fracture. Although many articles can be used as a dressing in an emergency, use a sterile dressing whenever possible. Sterile dressings are available in many sizes and thicknesses. If a sterile dressing is unavailable, use the cleanest material at hand. A clean handkerchief or ironed dishtowel is suitable. Fresh newspaper also can be used, because it is clean. Remember to wear gloves, if at all possible.
Using Bandages
A bandage is a piece of material used to hold a dressing or splint in place, to give support, or to apply pressure. When applying a bandage in an emergency, follow these guidelines:
• Apply the bandage firmly but not so tightly that circulation is restricted. Watch for evidence of tightness: blanching of skin, loss of sensation, and absent pulse. Loosen the bandage if necessary.
• If a knot is used, always tie a square knot because it will not slip and can be easily untied.
• If possible, leave the tips of the person’s toes and fingers exposed. Rationale: Checking for impaired circulation is necessary to ensure adequate tissue perfusion. Assess for pallor, lack of pulse, pain on passive motion, paresthesia (burning, tingling), or paralysis. (This assessment is known as CMS: color, motion, and sensitivity or sensation.).
Applying Cravat Bandages and Slings
A triangular or handkerchief bandage can be made from a square of cloth and secured without tape or pins, if necessary. Fold the cloth several times to make a strip or cravat bandage. A triangular bandage also may be used to make a sling for arm support. The steps for applying a sling are described at In Practice: Nursing Procedure 43-1.
Dental Injuries and Missing Teeth
Teeth may be displaced or knocked out accidentally. A tooth that is pushed up into the socket is called an intrusion injury. A tooth that is knocked out is called an avulsion injury. In either event, immediate dental care is necessary.
In an avulsion injury, the dentist may be able to reimplant and reposition the tooth. An avulsed tooth that is reimplanted within 30 minutes has a 90% chance of being saved. It may be saved if reimplanted within 2 hours. First aid for avulsed teeth is outlined at In Practice: Nursing Care Guidelines 43-3.
IN PRACTICE: NURSING CARE GUIDELINES 43-3
GIVING FIRST AID FOR AN EVULSED TOOTH
• Ask bystanders to look for the missing tooth. Instruct them to pick it up with a sterile piece of gauze by the crown and not to touch the root. Rationale: Touching the root may damage important structures.
• Call a dentist immediately The person must see a dentist or go to an emergency department as soon as possible. Rationale: The sooner a tooth is repositioned, the more likely it is to be saved.
• Clean the person’s mouth with gauze. Using sterile gauze, have the client gently bite down. Rationale: Doing so will restrict bleeding and reduce pain.
• Instruct the person not to put pressure on adjacent teeth. Rationale: The accident may have loosened adjacent teeth.
• If possible, have the person bite gently on a dry tea bag. Rationale: Tannin in tea acts as a natural coagulant and helps to stop bleeding.
• Do not allow the client to suck on a straw or smoke. Rationale: The sucking action may loosen a blood clot and cause more bleeding.
• Place the tooth on sterile gauze. You may clean it by dipping it in milk, while holding the crown. Keep the tooth under the person’s tongue or in milk until arriving at the dentist. Rationale: Using water or any solution other than milk or the person’s own saliva may damage the root.
Key Concept If the person can cooperate,have him or her hold an evulsed tooth under the tongue en route to the dentist. Otherwise, place the evulsed tooth in milk. Rationale: The client’s own saliva or the milk will help to preserve the integrity and viability of the tooth’s root system.
Foreign Objects
Aforeign object is any abnormal object or substance lodged in a body orifice or structure.
Foreign Objects in the Eyes
Foreign objects in the eye can be particles of dust or soot or an eyelash resting on the eyelid’s lining. Particles also can become embedded in the eyeball. Anything that lodges on the cornea irritates it, especially when the eyelid opens and closes. A foreign object can scratch or permanently damage the cornea. Foreign objects have a scratchy effect and cause tears to flow. This is a natural body defense mechanism. Often, the tears will wash out the foreign object and no treatment is needed.
Caustic substances are those that burn or destroy flesh. A caustic substance in the eye is extremely irritating and very dangerous. Sometimes in an industrial accident, chemicals enter a person’s eye. Quick action must be taken to flush the eye with water. In Practice: Nursing Care Guidelines 43-4 summarizes skills in the emergency care of eye injuries. If any question exists about the injury’s severity, seek medical assistance as soon as possible.
Most contact lenses used today can remain in the person’s eyes for several hours without incident. If lenses are left in place following an accident, the medical team must be aware of this fact. The person’s corneas can become ulcerated if he or she does not blink. Hard or gas-permeable contact lenses are more likely to cause corneal ulcers than soft lenses. In some cases, removal of contact lenses at the scene of an accident is necessary. A special suction cup is available for this purpose.
Foreign Objects in the Nose or Ears
Children often insert small objects into their noses or ears. To remove an object from a child’s nose, have the child blow the nose gently with both nostrils open. Unless the object is clearly visible and at the edge of the nostril, do not attempt to remove it with a finger or instrument. Call for medical assistance. If a foreign object lodges in a person’s ear, do not attempt to remove it. Instead, transport the person to a healthcare facility.
Nursing Alert Be aware that an object such as a bean or a dried pea will swell when moistened. This makes these objects very difficult to remove, especially from the nose.
Airway Obstruction
Foreign objects often become lodged in the throat. If the foreign object is not visible but the victim is able to breathe adequately, call for emergency medical assistance or take the person to an ED. If the person is not exchanging air and shows signs of respiratory distress, call 911 and use appropriate obstructed-airway techniques if you have been properly trained. (All nursing students should receive CPR training and should renew this certification on a regular basis.) An airway obstructed by a foreign body will quickly cause respiratory arrest. Anytime a person (particularly a child) becomes cyanotic, stops breathing, and collapses for no apparent reason, suspect an obstructed airway.
Children may put coins or buttons in their mouths. Bits of food or bones can lodge in a child’s throat or esophagus. In an adult, foreign body obstruction is usually caused by a large piece of food becoming lodged in the airway. Meat is the most common cause. Poorly fitting dentures and alcohol ingestion also are associated with obstructed airways. Certain medical conditions, including a neuromuscular disease such as Huntington’s, or strokes, cleft palate, brain injury, seizure disorders, heavy sedation, decreased saliva production, or a diminished or absent cough or gag reflex, can increase the risk for choking. Older adults who cannot chew food well are also at risk for choking.
Airway obstruction often occurs in restaurants. The person is embarrassed by the incident and suddenly leaves the table. Suspect an obstructed airway when you see a person coughing and gasping, who looks frightened and suddenly leaves the table. Follow the person, and ask if he or she is choking. If this person goes off alone, he or she may die. This common occurrence is called a café coronary. The person leaves the table, goes to the restroom, and may be found not breathing and without a heartbeat (an apparent heart attack victim).
IN PRACTICE: NURSING CARE GUIDELINES 43-4
GIVING FIRST AID FOR EYE INJURIES
First Aid for Foreign Objects in the Eye
♦ Instruct the person not to rub his or her eye. Have the person keep the eye closed and avoid blinking. Rationale: Rubbing or blinking may drive a foreign object deeper into the eye.
♦ Never use an instrument, toothpick, or match to remove a foreign object. Rationale: These items are unsterile and may introduce pathogens into the eye and scratch the cornea.
♦ Never attempt to remove a foreign object if the slightest possibility exists that it is embedded in the cornea. Rationale: You could drive the object deeper into the eye and cause more serious damage.
♦ Remove contact lenses. Rationale: Contact lenses can contribute to further aggravation and injury.
♦ Treat both eyes even if only one is injured. Rationale: A sympathetic injury can occur.
When the Object Is not Embedded
♦ Pull down the person’s lower eyelid to see whether the object is on the eyelid membrane. Rationale: If the object is on the inside of the eyelid, you may be able to lift it off by touching it gently with the corner of a clean handkerchief or with a cotton-tipped applicator moistened in water.
♦ Always moisten the cotton tip of an applicator before touching it to the eye. Rationale: Small particles of dry cotton can become lodged in the eye.
♦ If the object is under the person’s upper eyelid, grasp the lashes of the upper eyelid with your forefinger and thumb; ask the person to look upward; gently pull the lid forward and downward over the lower eyelid. Rationale: Usually the eyelash movement dislodges the foreign body and tears wash it away.
♦ Flush the eye with plain water Rationale: Sometimes the pressure of the water will flush an object out of the eye.
First Aid for Caustic Materials in the Eye
♦ Flush the eye with large amounts of water or normal saline solution. Rationale: Eyes are sensitive to chemical or thermal burns. It is vital to use a large amount of water to cleanse the eye. You can use a sterile medicine dropper or a small sterile bulb syringe. Do not use an unsterile eye cup. Rationale: Eye cups may introduce pathogens into the eye.
♦ Use an eyewash sink or shower if possible. Have the person stand over the sink, with the eyes close to the jets. Encourage the person to keep the eyes open as much as possible. When the water is turned on, the jets direct a continuous stream of water into the eyes. Rationale: Large amounts of water are necessary, which are easily provided with an eyewash sink.
If any caustic material splashes into the eye, immediately flush the eye with large amounts of water.
♦ Do not instill another substance into the eye in an attempt to neutralize a caustic substance. Rationale: Putting another substance into the eye could do more damage.
♦ Have the person see a physician immediately Rationale: Prompt action is necessary to prevent permanent eye damage.
The person who has a partially obstructed airway with good air exchange will cough forcefully. Wheezing may be present, but air exchange is obvious. Encourage the person to cough. Do not interfere with attempts to expel the obstruction, and do not leave the person. Offer encouragement and continue to monitor him or her. If the person’s condition does not rapidly improve, activate the EMS. Poor air exchange may be identified by ineffective coughing and sometimes by high-pitched wheezing sounds called stridor. The person often experiences increasing respiratory difficulty and may become cyanotic.
In a complete airway obstruction, the person is unable to talk, breathe, or cough. The person may even indicate the condition by using the universal signal for choking, which is clutching the neck between the fingers and thumbs of both hands (Fig. 43-11). In complete airway obstruction, no oxygen enters the lungs. The person will soon become unconscious unless the obstruction is removed. Use the Heimlich maneuver, also called abdominal thrusts, in the case of complete airway obstruction. (The Heimlich maneuver is not described in this topic.) Enroll in a specialized class to learn the basics of this life-saving skill. All nurses should be able to perform this skill.
Cardiovascular Emergencies
Fainting
Fainting (syncope) is caused by an insufficient supply of blood and oxygen to the brain. Extreme hunger, tiredness, heat, or being in an oxygen-deprived environment can cause a person to faint. Fainting can also result from emotional shock. Severe hemorrhage, excruciating pain, and standing in one place for a prolonged period, especially with the knees locked, are other causes.
FIGURE 43-11 · Grasping the throat is the universal sign for choking. Emergency first aid must be instituted immediately.
The symptoms of imminent fainting include dizziness, blackness or spots before the eyes, pallor, and excessive perspiration. The person loses consciousness; the pulse is weak and breathing is shallow. In Practice: Nursing Care Guidelines 43-5 may be used for the person who has fainted or who feels faint.
IN PRACTICE :NURSING CARE GUIDELINES 43-5
ASSISTING THE CLIENT WHO IS FAINTING
• When someone complains of feeling faint, have the person sit or lie down and bend his or her head forward between the knees. Maintain the person in this position. Rationale: When the head is lower than the heart, more blood is carried to the brain.
• Loosen tight clothing. Rationale: Tight clothing can constrict breathing, further reducing the amount of oxygen carried to the brain.
• If the person is unconscious, assess for respirations and pulse. Start CPR if necessary Rationale: A life-threatening condition may be the cause of unconsciousness.
• When the person regains consciousness, help him or her to rise slowly first to a sitting and then to a standing position. Rationale: The person may feel weak and could fall.
• Do not allow the person to move until he or she has fully regained consciousness. Rationale: The person’s altered level of conciousness may be due to a serious condition, such as a skull fracture, concussion, stroke, cerebral hemorrhage, or shock.
Suspected Heart Attack
In an MI, some of the heart’s blood supply is cut off, causing heart muscle tissue to die. This is usually the result of a blockage in a coronary artery (one of the arteries supplying the heart itself). The location and extent of the infarction determines the seriousness of the MI.
The person usually complains of chest pain, which may radiate to the left (or right) arm. Rest usually does not relieve this pain. Other symptoms include pain radiating to the back, neck, jaw, or teeth; the pain may also be mistaken for heartburn or indigestion. Be aware that pain may also occur in other places. The person may have been having symptoms off and on for several days (unstable angina). Other common symptoms of MI include restlessness, panic, and a sense of impending doom; difficulty breathing and other signs of respiratory distress; and changes in pulse quality and rate. The skin is cold and clammy and the person may be cyanotic (indicating lack of oxygen to the tissues). If a person has any of these symptoms, suspect a heart attack and call for help immediately.
Recent research has shown that many more women die of heart attacks each year than was previously believed. Nearly all research has been done on men; the symptoms of heart attack in women may be different. Heart attack (myocardial infarction—MI) symptoms in women often include:
• Shortness of breath, difficulty in catching the breath
• Nausea and flu-like symptoms, chills, cold sweat
• Light-headedness, faintness
• Heart palpitations
• Chest pain perhaps, but not necessarily
• Discomfort in other areas, including the neck, jaw, back, and arms (most often the left arm); a common location of pain is the shoulder blades or between the shoulder blades
• Heartburn and stomach pains
• Extreme fatigue
Prompt action is the most important factor in whether a person lives or dies following an MI. Thrombolytic medications dissolve the clot and clear the blocked blood vessel. Plain aspirin is often given as an immediate emergency first-aid measure to help thin the blood. Aspirin has improved the success rate in saving lives when administered within 1 hour of the attack. In Practice: Nursing Care Guidelines 43-6 presents first aid for the person with a suspected heart attack.
Nursing Alert The most frequent common denominator in heart attack is denial. The person cannot believe that he or she is having a heart attack.
Bleeding
Nosebleed (Epistaxis)
The medical term for nosebleed is epistaxis. In Practice: Nursing Procedure 43-2 gives the basic steps for treating a nosebleed.
Nursing Alert If the person with a nosebleed has a fractured skull, do not attempt to stop the bleeding. Doing so could increase intracranial pressure. In severe hypertension, a nosebleed may be the body’s safety valve against a cerebrovascular accident (stroke).
![tmpd9b293_thumb[2][2][2] tmpd9b293_thumb[2][2][2]](http://what-when-how.com/wp-content/uploads/2012/08/tmpd9b293_thumb222_thumb.png)

