Z-Track or Zig-Zag
Method Certain medications, such as iron preparations and steroids, irritate the skin’s dermal and subcutaneous layers. These medications must be injected deeply into muscle tissue. The
TABLE 64-1. Choosing Sites for Intramuscular Injections
|
SITE |
AGE GROUP |
AMOUNT OF SOLUTION PER INJECTION |
|
Deltoid (upper arm) |
Children age 4-15 years Children > 15 years and adults |
0.5 mL 0.5-2.0 mL |
|
Rectus femoris (anterior thigh) |
Infants and toddlers Preschoolers |
0.5-1.0 mL up to 1.5 mL |
|
Ventrogluteal (side hip) |
Toddlers >3 years Preschoolers School-age children Older children and adults |
1.0 mL up to 1.5 mL up to 2.0 mL up to 2.5 mL |
|
Dorsogluteal (back of hip) |
Children 3-6 years 6-15 years > 15 years |
up to 1.5 mL up to 2.0 mL 2.0-2.5 mL |
|
Vastus lateralis (side thigh) |
Infants and toddlers Adults |
up to 2.0 mL up to 3.0 mL |
FIGURE 64-9 · Z-track ("zig-zag”) injection. (A) The tissue is tensed laterally at the injection site. This pulls the skin, subcutaneous tissue, and fat planes into a "Z” formation. (B) The needle is inserted. (C) After the injection, the tissues are slowly released while the needle is withdrawn. As each tissue plane slides by the other, the track is sealed.
Z-track method (“zig-zag” method) is recommended for administering these or any other medications that irritate skin and other body tissues (Fig. 64-9).
The Z-track method helps prevent medication from leaking back onto the skin. Use the Z-track method only in the gluteal muscles. To administer a medication by Z-track, pull the skin of the injection site to one side. Insert the needle, aspirate, and inject the medication. Keep the skin taut and pulled to one side; wait a few seconds before withdrawing the needle. Allow the skin to return to its original position slowly, while removing the needle. As the tissues slide past each other, they close the needle track. Do not massage the injection site when using the Z-track administration method.
INTRAVENOUS ADMINISTRATION
Fluids are administered via the circulatory system to correct or prevent fluid and electrolyte imbalance in the client. For example, the client who is given nothing by mouth (NPO) for surgery often receives IV fluids postoperatively. IV access is also used to administer medications. Peripherally placed catheters are used for short-term administration of fluids and nutrients. Central lines are used for longer-term administration and for certain products that cannot be administered through a peripheral line.
In some states and provinces, an LPN/LVN does not work with intravenous lines. However, it is becoming more common for these nurses to monitor IVs and, in some cases, to administer medications via IV. This is particularly true if the home care client is receiving IV therapy. In this case, caregivers are taught by the nurse to manage the IV and the nurse assists and teaches them.
NCLEX Alert The NCLEX can use situations that include equipment for administering medications. You will need to know the concepts of administration by injection or IV such as the gauge of the needle, the size of a syringe, the type of IV pump, and the best injection site. Your response may also need to consider the setting of administration such as acute care, hospice, or home.
Key Concept Nursing assistants do not work with IVs, except to report problems.
The IV infusion may be run as a primary infusion, one IV line running continuously. An IV may also be run in tandem, that is, a primary infusion plus a smaller bag. The smaller bag is connected at the same level as the primary bag. In this case, both the primary and the tandem bag infuse in at the same time. The IV infusion may also be run as a piggyback infusion, which will be discussed later in this topic.
Key Concept In nearly all cases, IV solutions are supplied in plastic bags. Glass bottles are used only if the IV solution would be unstable in a plastic bag. The glass bottle must be vented to facilitate the flow of the fluid (see In Practice: Nursing Care Guidelines 64-2).
Nursing Alert If the tandem bag is not clamped off immediately when the medication is infused, the fluid from the primary infusion will back up into the tandem line.
Intravenous injections and infusions allow the introduction of fluid solutions of electrolytes, nutrients, vitamins, and medications directly into the bloodstream. Medications are absorbed more rapidly via the IV route than any other commonly used route. Large quantities of a solution may be given IV by way of an infusion. A solution flows at a constant, continuous rate into the client’s vein with the aid of gravity or an infusion pump or controller. IV infusions are commonly given for fluid replacement caused by dehydration or excessive blood loss, electrolyte replacement, antibiotic therapy, chemotherapy, or nutrition. If blood or blood products are administered IV, the procedure is referred to as a transfusion.
IN PRACTICE :NURSING CARE GUIDELINES 64-2
CARING FOR THE CLIENT RECEIVING INTRAVENOUS (IV) THERAPY
• It is important to prepare the client properly for IV therapy. The client must understand the reasons for this therapy, as well as the specifics of the procedure, the pump, and so on. The client must know what to expect and what is expected of him or her Rationale: If the client is prepared, he or she will be more comfortable and accepting of the process.
• Universal Precautions are followed when dealing with infusions or transfusions. Rationale: The IV is in direct contact with the client’s blood.
• Monitor the IV site for swelling, coolness, fluid leaking, and pain. Lower the bag below the level of the insertion site to determine if blood returns. Visually inspect the insertion site. Rationale:
Swelling, coolness, and leaking fluid are signs of infiltration. If blood returns when the bag is lowered, the infusion is most likely in the vein, but may still be leaking into the tissues.
Inspecting the IV site. Note that it is covered with a transparent dressing, for easy viewing. The date of application is written on the dressing. Make sure the slide clamp (white) is open when the IV is running. Gloves are worn if the IV is to be discontinued or tubing or dressing changed.
• It is helpful if the client (or family) also know what to watch for Rationale: If the client knows how the infusion should operate, he or she can report signs of infiltration, an emptying bag, pump alarm, or other concerns to the staff. Thus, any problems can be dealt with immediately. It is important that the client realize that these situations are not life threatening and can usually be easily rectified.
• If signs of infiltration exist, stop the infusion and report the situation immediately. The provider will determine if the infusion should continue or be discontinued. Rationale: The primary provider will usually order an infiltrated infusion to be discontinued, unless the situation can be quickly corrected. Tissue damage may result if major infiltration is allowed to continue.
• Check the IV fluid (IVF) to make sure there is no cloudiness or sediment. Rationale: If the fluid is not perfect, it could be dangerous for the client.
• The IV is not irrigated to determine patency Rationale: If a clogged or stopped IV has caused a blood clot in the vein, the clot could be dislodged, which would be life threatening.
• Monitor the infusion site for redness or hardness that follows the vein. Rationale: This is a sign of phlebitis, which can also be life threatening.
• The rate of flow and amount and type of solution present are carefully monitored. The pump or controller is frequently checked. Most IV tubing is continuous, so loose connections between parts of the tubing are not a concern, unless old-style tubing is being used. However, it is important to make sure the bag spike and the connection to the venous access device are firmly in place. Remember that correct programming of the pump is one of the "7 Rights” of medication administration. Rationale: It is important to ensure that all settings are correct and that the fluid is flowing properly.
• A pump alarm must be investigated immediately. Rationale: This is reassuring to the client and any difficulty can be quickly corrected.
• Do not write on an IV bag with a felt tip marker or pen. To label a bag, use a preprinted sticker or a piece of tape. Rationale: The ink may penetrate the plastic bag and contaminate the IV fluid. The tip of a pen could also pierce the bag.
• It is important for the designated nurse to replace IV bags before they become totally empty Rationale: It is hazardous for the client if air has collected in the tubing. In addition to removing the air from the tubing, the pump controller also must be reset if the bag has been allowed to empty completely. The venous blood may also clot if the bag runs dry; this can be a very dangerous situation.
• The infusion site is carefully protected. It is important for nurses to be aware of the tubing and pump during transfers, ambulation, or other activities. Remember the IV controller works on the principle of gravity Rationale: If the tubing gets in the way, the client could trip and fall or dislodge the tubing from the bag or the insertion site. If the bag of solution is too low, blood will flow up the tubing and may cause complications.
• All clamps and connections are double-checked when changing tubing, adding medications, or removing IV tubing from a pump or controller Rationale: If the flow rate is not regulated properly, the client could receive a bolus of medication that may cause overdose. In addition, the client may not receive the required amount of fluids or fluid may be lost if tubing is not properly clamped.
• Prevent the IV site from getting wet or soiled. Rationale: This helps reduce the possibility of infection. Moisture is a route of transmission for pathogens.
• If the client will be away from the nursing unit for tests or procedures, nursing staff must make sure there is adequate solution to be infused while he or she is gone. A pump or controller usually has a backup battery so the client can be transported from place to place. It is important to make sure the battery is charged. Rationale: This allows the client to receive the infusion without interruption. The backup battery also is important in the event of a power failure.
• Plug the unit back in if the client will be waiting for any period of time. Rationale: This recharges the battery.
• IV dressings are changed according to the facility’s policy For example, dressings over Hickman catheters often are changed every 72 hours. In addition, the dressing is changed if it becomes wet or contaminated with drainage. It is standard practice to use clear dressings over the IV site. Rationale: Each time the dressing is changed, there is a chance of contamination or dislodging the catheter. However, dressings must be changed at appropriate intervals, to allow staff to inspect the site and to prevent infection. Clear dressings provide an opportunity to observe the site without removal of the dressing each time.
NURSING CARE GUIDELINES 64-2 continued
• IV tubing is changed, as per agency protocol. Most facilities require the nurse changing IV tubing to have special inservice education or a procedure test-out. He or she must attach the preprinted sticker date, and initial it when changing tubing. It may be necessary to change IV tubing before the scheduled time (see Nursing Procedure 64-5). Rationale: The label allows other staff to know when tubing was last changed. New tubing is required if the tubing seems to be in danger of becoming clogged, if it becomes severely kinked, and in other circumstances.
• Gloves are worn at all times when starting or discontinuing an IV and often when adding medications. Rationale: An IV site presents direct exposure to the client’s body fluids, particularly blood. Gloves also help protect the client from risk of infection.
• The less the nurse handles dressings and connections to the bag or IV catheter; the lower the client’s risk of infection.
• If the client is receiving total parenteral nutrition (TPN), it is run through a filter (see Nursing Care Guidelines 64-3). Other instances in which a filter is used include the administration of blood or blood products,during pediatric IV administration (in most cases), and sometimes if the client is at high risk for infection. Lipids (fats) are not to be run through a filter;
Nursing Alert Remember to watch for the following complications when working with IVs:
• Infiltration
• Phlebitis
• Embolism (thrombus)
• Infection (sepsis)
Infusions
Healthcare facilities, as well as home care agencies and clinics, commonly use IV infusions. Although the LPN/LVN may or may not be responsible for initiating an IV infusion, he or she is often responsible for monitoring it. Careful monitoring of IV infusions is a must. Monitor the IV site for patency (openness), inflammation, infection, or infiltration (the flowing of fluid into tissues instead of the vein). In Practice: Nursing Care Guideline 64-2 presents information regarding the monitoring of a client with an IV. It is important to note the rate of administration and type of fluid being administered. Healthcare facilities use a flow sheet on which nurses enter hourly documentation concerning site condition, infusion rate, and specific medications or fluids being given.
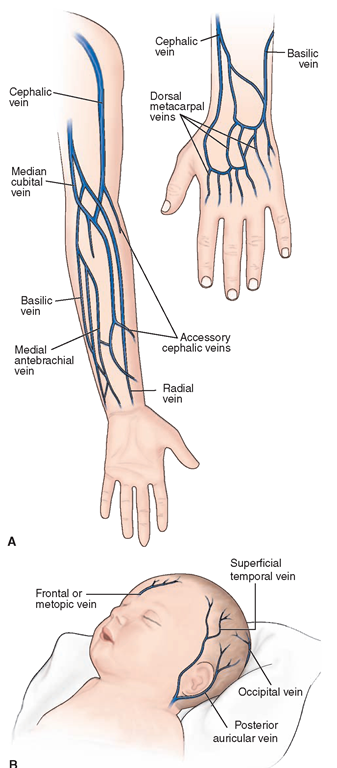
Over-the-needle or inside-the-needle catheters are nearly always used to initiate IV infusions. The initial IV is often started in the hand. If this IV infiltrates, the IV may be restarted in the outer aspect of the forearm. The wrist and inner aspect of the forearm may also be used, but they are more painful when started (Fig. 64-10). Veins located over bony prominences or joints are poor insertion choices, because these sites often cause occlusion of the vein, interfering with the infusion’s delivery (Box 64-1). After the needle has been inserted into the vein and the catheter placed, the needle is withdrawn, leaving only a flexible plastic catheter in the vein. A length of IV tubing is attached to the catheter hub, which is in turn attached to the plastic bag that contains the prescribed solution. If a pump or controller is not used, a roller clamp on the tubing regulates the flow rate. If the clamp is completely closed, the flow is occluded and stops completely (Fig. 64-11).
BOX 64-1. Considerations in Determining Venous Access Sites
• Peripheral veins vary in size. Choose a vein by considering its size for the purpose, length of time the vein will be accessed, mobility requirements, and comfort for the client.
• If the client is dehydrated, the peripheral veins may be partially collapsed and it may be difficult to locate a vein.
• It may be difficult to locate a vein in an obese client. A longer needle may be needed.
• Small children and infants have smaller veins. Different venipuncture sites and different needles and tubing are often used. Special techniques may be required.
• Older adults may be dehydrated, may be debilitated, and often have friable skin. Access may be difficult.
• A client who is very ill may have poor circulation. Access may be difficult.
• If there is any doubt, seek assistance.
Initiating the Intravenous Infusion
In some areas of the country, an LPN/LVN is allowed to initiate IV infusions. In this case, supervised practice and a procedural test-out are often required. The nurse must carefully follow the provider’s orders regarding the type of venous access device to use, the amount and type of IV solution, and the rate at which the infusion is to be administered.
IV Solutions
The most commonly used IV solutions include normal saline (0.9% NS or 0 .9% NaCl), 5% dextrose in normal saline (D5NS), 5% dextrose in sterile water (D5W), and 5% dextrose in 0.45% normal saline (half-normal saline; D5!4NS). The primary provider specifies the type of IV solution to use, in addition to the rate at which to infuse the solution. Follow the same safety precautions when administering IV solutions as for administering any medication. Always observe the "7 Rights” of administration (including accurate programming of pumps) and sterile technique very carefully (Nursing Procedure 64-5).
FIGURE 64-10 · Commonly used infusion sites. (A) Ventral and dorsal aspects of arm and hand. (B) Scalp veins (usually only used for infants.
Infiltration of the IV
If the IV fluid is not flowing into the client’s vein, but into surrounding tissues, this is known as infiltration. This can be a dangerous and painful situation and must be corrected as soon as possible.
FIGURE 64-11 · The roller clamp is used to control or stop the flow of intravenous (IV) fluid. When the roller is moved down to the narrower part of the clamp, the flow is stopped. When it is moved up to the larger part, the fluid is allowed to flow.
Key Concept Signs of infiltration include:
• Swelling or puffiness
• Coolness
• Pain at the insertion site (sometimes).
• Feeling of hardness in the area and possible leaking of fluid evident around the catheter
Rationale: The area feels cool, because IV solutions are typically at room temperature, which is cooler than body temperature. The symptoms listed indicate that the IV fluid is flowing not into the vein, but into the surrounding tissues. The fluid may be leaking around the site, even though the catheter is in the vein; this can indicate that the flow of fluid is too fast.
Nursing Alert Another complication is phlebitis, inflammation of a vein. In this case, there may be redness and a cordlike mass, which follow the vein. Other symptoms of phlebitis include pain and tenderness, swelling, and warmth in the area. This can be a dangerous situation if a blood clot forms.
Pumps and Controllers
Infusion pumps incorporate the use of positive pressure to deliver a preset fluid volume (see In Practice: Nursing Procedure 64-5). The disadvantage of the pumps is that, in some cases, they continue to pump fluids even though the catheter may have been displaced from the vein. It is important that the nurse watch for adverse reactions. All IV sites should be checked at least hourly.
Electronic infusion controllers are most often used in the nonacute setting. They use gravity to maintain the flow of IV fluids at a preset rate. The height of the IV bag must be sufficient to allow for the force of gravity. Controllers sense the number of drops infusing and control the rate and amount of IV fluid. The controller sounds an alarm if air is in the tubing, the bag is empty, or the flow is obstructed. It is important to inspect the infusion site frequently, to make sure it is not infiltrated.
Programming an infusion pump or electronic controller varies with the manufacturer; however, both units can be programmed to deliver a preset fluid amount at a preset infusion rate. In addition, both units are equipped with memory systems that continuously total the volume of fluids infused. The nurse must have access to the instruction manual or receive specific inservice education in the local facility before programming pumps or controllers and otherwise working with IVs. Safety features are built into each machine to avoid erroneous programming. When a client at home is receiving fluids using an infusion pump or controller, instruction is vital. The client and family must understand the pump and its safety features, especially the sounding of an alarm if the tubing becomes obstructed or the IV bag becomes empty. Tell the client and family members not to shut off the alarm until the situation has been corrected.
Nursing Alert Because IVs are considered to be medications, it is important to remember that correct programming of controllers and pumps is the "seventh right” in the guidelines for administration of medications. Many facilities require that two nurses double-check pump programming.