Caudal Basal Pontine Syndrome
Occlusion of paramedian pontine arteries and long circumferential arteries causes caudal basal pontine syndrome. It is characterized by contralateral upper motor neuron paralysis (due to involvement of the corticospinal tract), ipsilateral facial weakness (due to damage to the facial nucleus), and ipsilateral gaze paresis (due to damage to the pontine gaze center and abducens nucleus.
Locked-in Syndrome
A lesion of the ventral half of the pons due to occlusion of paramedian and short circumferential branches of basilar artery may cause locked-in syndrome. It is characterized by paralysis of all motor activity due to damage to the cor-ticospinal tract in the ventral pons and loss of voice (aphonia) due to damage to the corticobulbar fibers passing through the basal pons. These patients can communicate with vertical gaze and blinking of eyes as these functions are spared.
Medial Tegmental Pontine Syndrome
In medial tegmental pontine syndrome the structures damaged are the abducense nucleus and nerve (cranial nerve [CN] VI), genu of facial nerve, and medial lemnis-cus. Occlusion of the paramedian branches of the basilar artery are likely to affect these areas (Fig. 27-9). The syndrome is characterized by ipsilateral paralysis of CN VI, lateral gaze paralysis, ipsilateral facial paralysis, and con-tralateral loss of kinesthetic and discriminative touch senses.
Caudal Tegmental Pontine Syndrome
In caudal tegmental pontine syndrome there are lesions in the caudal pons. The structures affected are the corti-cospinal tract, causing contralateral hemiparesis; the abducens nucleus, causing conjugate gaze palsy; and the facial nucleus or nerve fibers, causing facial muscle weakness. Occlusion of the paramedian branches of the basi-lar artery supplying these structures in the caudal pons cause these symptoms.
One-and-a-Half Syndrome
The lesions in one-and-a-half syndrome are generally caused by occlusion of paramedian branches of the basilar artery that supply the dorsal paramedian pontine tegmentum (Fig. 27-9). Ipsilateral gaze paralysis occurs due to damage to the abducens nucleus. Damage to the medial longitudinal fasciculus (MLF) results in internuclear ophthalmoplegia, which involves paralysis of adduction of the eye ipsilateral to the lesion and nystagmus of the abducting eye.
FIGURE 27-9 Arterial supply of the pons (schematic representation). Important structures are shown on the left and the pattern of arterial blood supply is shown on the right side of each diagram. CSp = corticospinal fibers; CTT = central tegmental tract; MCP = Middle cerebral peduncle; ML = medial lemniscus; MLF = medial longitudinal fasciculus; RB = restiform body (inferior cerebellar peduncle); RetF = reticular formation; SCP = superior cerebellar peduncle.
Rostral Basal Pontine Syndrome
Interruption of blood flow in the long circumferential branches of the basilar artery and AICA may cause lesions in the rostral pons, involving the trigeminal nerve. Rostral basal pontine syndrome is characterized by ipsi-lateral trigeminal sensory and motor symptoms and contralateral hemiplegia of the upper motor neuron.
Dorsolateral Tegmental Pontine Syndrome
Dorsolateral tegmental pontine syndrome is characterized by lesions of the dorsolateral pontine tegmentum on one side and dorsolateral medulla on the contralat-eral side. It is characterized by dissociated sensory loss (i.e., loss of pain and temperature sense but preservation of vibration and position sense) of the entire body. Dissociated sensory loss can be attributed to bilateral damage to the trigeminal and spinothalamic tracts but sparing of the medial lemniscus. Damage to the fibers destined for the cerebellum and passing in the tegmen-tum may cause ataxia of the limbs and trunk. The syndrome is generally caused by occlusions of AICA on one side, and posterior inferior cerebellar artery (PICA) on the contralateral side.
Rostral Tegmental Pontine Syndrome
Rostral tegmental pontine syndrome is characterized by lesions in the rostral pons, and the structures affected are the medial lemniscus, MLF, spinothalamic and corticospi-nal tracts, and cerebellar fibers. Although the corticospi-nal tract is not located in the tegmentum proper, some damage to the dorsal part of this tract may occur because the lesions are not circumscribed. The symptoms consist of ophthalmoplegia due to damage to the MLF, contralat-eral hemiparesis due to damage to the corticospinal tract, hemisensory loss due to damage to the spinothalamic tract and medial lemniscus, and ipsilateral ataxia due to damage to cerebellar fibers. Occlusion of the superior cerebellar artery and paramedian branches of the basilar artery supplying the rostral pons cause this syndrome.
Medullary Vascular Syndromes
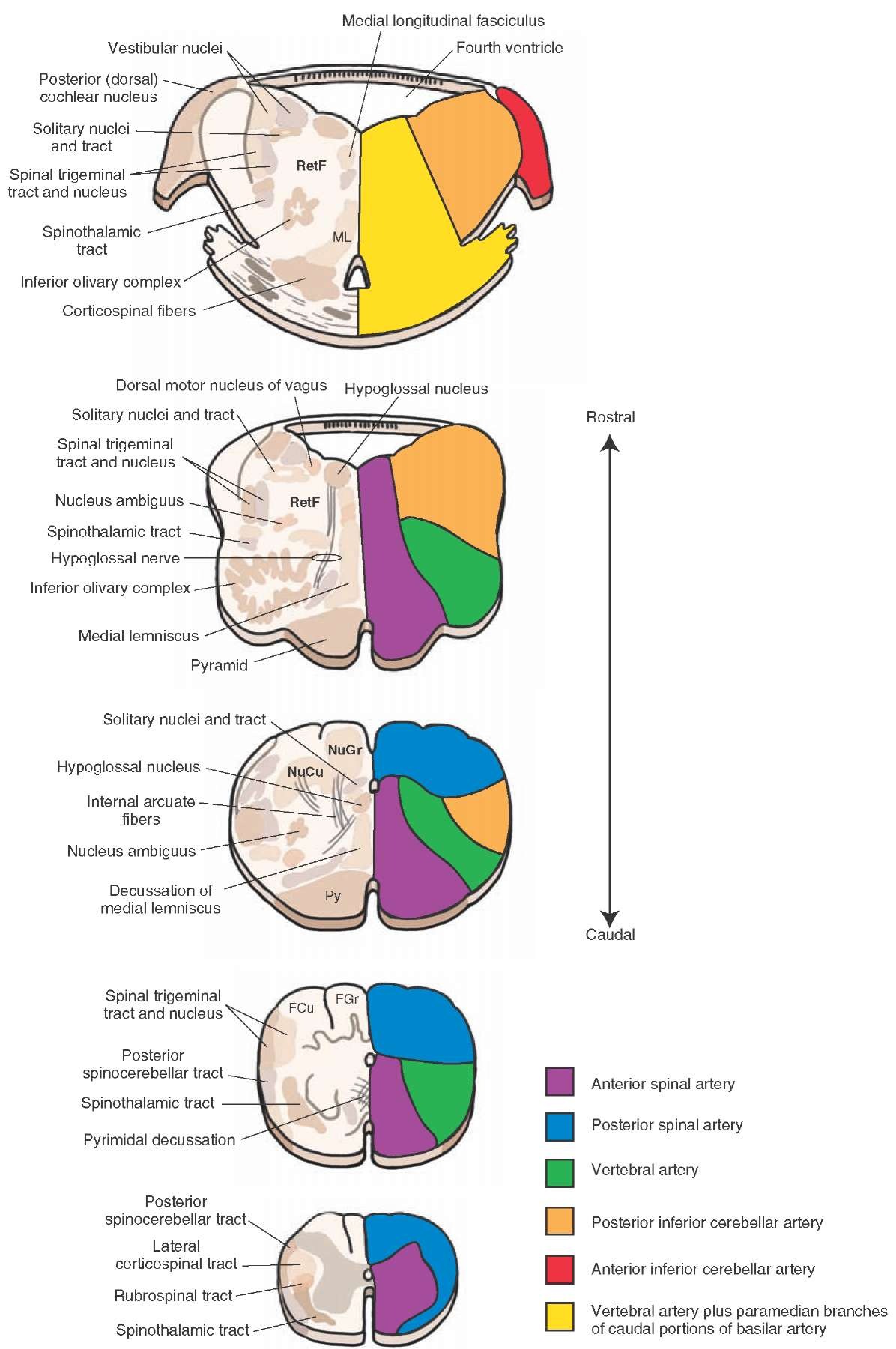
The blood supply at different levels of the medulla is shown in Figure 27-10. Occlusion of one or more of the arteries supplying the medulla causes the following syndromes.
Lateral Medullary Syndrome
Lateral medullary syndrome is also called Wallenberg’s syndrome.It is caused by occlusion of posterior inferior cerebellar artery (PICA). This syndrome is characterized by the following symptoms: (1) dysphagia (lack of coordination in speech), dysarthria (disturbance of articulation), and difficulty in swallowing (all of these symptoms are a result of the paralysis of the laryngeal muscles caused by the damage to the nucleus ambiguus, which innervates the laryngeal muscles); (2) analgesia and thermoanesthesia on the ipsilateral side of the face due to damage to the nucleus and spinal tract of the trigeminal nerve; (3) contralateral loss of pain and temperature (of the body) due to damage to the spinothalamic tract; (4) vertigo, nausea, vomiting, and nystagmus due to damage to portions of the vestibular nuclei; (5) ipsilateral Horner’s syndrome due to damage to hypothalamospinal fibers descending through the lateral medulla; and (6) ipsilateral gait and limb ataxia due to damage to the cerebellum.
Medial Medullary Syndrome
Medial medullary syndrome is also called Dejerine’s syndrome . In this syndrome there are lesions in the pyramid, medial lemniscus, and hypoglossal nerve fibers. The symptoms include loss of conscious proprioception, touch and pressure sensations from the contralateral side of the body, upper motor neuron paralysis on the con-tralateral side of the body, paralysis of the ipsilateral side of the tongue, and deviation of the tongue to the side ipsilateral to the lesion upon protrusion. The syndrome is caused by occlusion of the anterior spinal artery or paramedian branches of the vertebral arteries.
Dorsal Medullary Syndrome
In dorsal medullary syndrome the lesions are in the inferior cerebellar peduncle and vestibular nuclei. The symptoms include nystagmus, vertigo, vomiting (due to damage to the vestibular nuclei), and atxia (due to damage to the afferent fibers arising in the spinal cord and brainstem regions). The syndrome is caused by the occlusion of medial branch of PICA.
Stroke
Diseases involving the blood vessels that supply the brain can cause stroke, which is characterized by an acute onset of neurologic deficit lasting for at least 24 hours. A stroke can be caused by blockage of blood vessels (occlusive stroke) or by bleeding from vessels (hemorrhagic stroke). Occlusive strokes are generally caused by atherosclerotic lesions or thrombosis in blood vessels supplying the brain. Neurologic deficits that result from occlusion of different arteries have already been described in this topic. Hemorrhagic strokes are generally caused by long-standing high blood pressure or aneurysms in the vessels supplying the brain. When bleeding occurs at the surface of the brain, it is called an extraparenchymal hemorrhage. For example, some individuals are congenitally prone to have aneu-rysms at the circle of Willis that can rupture and cause subarachnoid hemorrhage. A blood clot (hematoma) is formed within the brain tissue when bleeding occurs intraparenchymally. The hematoma can obstruct blood flow to the adjacent brain tissue.
FIGURE 27-10 Arterial supply of the medulla oblongata (schematic representation). Important structures are shown on the left and the pattern of arterial blood supply is shown on the right side of each diagram. FCu = cuneate nucleus; FGr = gracile fasciculus; ML = medial lemniscus; NuCu = cuneate nucleus; NuGr = gracile nucleus; Py = pyramid; RB = restiform body (inferior cerebellar peduncle); RetF = reticular formation.
Insufficient blood flow to the brain is called brain ischemia; during brain ischemia, oxygen and glucose delivery to the brain tissue is reduced. In addition, toxic metabolites, such as lactic acid, cannot be removed efficiently due to reduced blood flow. Brief loss of consciousness caused by generalized cerebral ischemia due to insufficient flow of oxygenated blood to the brain is called syncope. Prolonged ischemia results in neuronal death, which is called brain infarction. The term "ischemia" should be distinguished from the condition known as "anoxia" in which the tissue is deprived of oxygen delivery. When the symptoms of ischemia last for short periods of time (usually 5-30 min, but less than 24 hours) and the ischemia is focal (as opposed to generalized ischemia), the term transient ischemic attack (TIA) is used. In a majority of cases, TIAs are caused by emboli dislodged from ulcerated atherosclerotic plaques located at the carotid bifurcation. Sometimes, reduction in the blood flow in the internal carotid artery due to atherosclerotic plaques can cause temporary interruption in the blood supply to the ipsilateral retina, which results in transient monocular blindness (fleeting blindness). There is a need for early recognition of TIAs because, if left untreated, 20% to 35% of these patients can develop permanent cerebral infarction.
Drugs that prevent or reduce platelet aggregation (e.g., aspirin) must be used for prophylaxis of stroke in patients with carotid stenosis. A vascular surgical procedure, called carotid endarterectomy, is beneficial in patients in whom marked stenosis (greater than 70%) of the carotid artery is present. In this surgical procedure, the common carotid artery and a portion of the external carotid artery are slit open by a longitudinal cut, and atherosclerotic plaques are removed. However, the procedure carries a risk of causing a stroke postoperatively due to dislodging of thrombi formed at the site where surgery is performed.
Drug treatment for TIAs and stroke include administration of agents that prevent or reduce platelet aggregation (e.g., aspirin, clopidogrel, and tirofiban), anticoagulants (e.g., heparin and warfarin), and thrombolytic agents (e.g., streptokinase, urokinase, and tissue plasminogen activator [t-PA]). The mechanism by which aspirin prevents or inhibits platelet aggregation can be summarized as follows. Normally, arachidonic acid (a 20-carbon fatty acid) is mobilized from membrane phospholipids by phospholi-pases. Arachidonic acid is then oxygenated by the enzyme cyclooxygenase (COX), and the prostaglandin, thromboxane A2, is formed. In pathological situations, thromboxane A2 released from the platelets promotes aggregation of platelets. Aspirin in low doses (81 mg) causes an irreversible acetylation of COX and inhibits thromboxane synthesis in platelets. Reduction of thromboxane synthesis in platelets results in reduced release of this prostaglandin, leading to prevention or reduction of platelet aggregation. Adenosine diphosphate (ADP), another substance released from platelets in pathological situations, is also a platelet aggregator. Drugs like clopidogrel (Plavix) block ADP formation and thus prevent or attenuate platelet aggregation. Glycoprotein (GP) receptors (e.g., GP Ilb/IIIa receptors), which are located on platelet membrane, bind fibrinogen and other molecules and promote clot formation. Activation of these GP receptors promotes platelet aggregation. Recently, drugs that block GP receptors on the platelets have been developed to prevent platelet aggregation. For example, tirofiban (Aggrastat) blocks GP Ilb/IIIa receptors on the platelets and prevents their aggregation. As mentioned earlier, thrombolytic drugs (e.g., streptokinase, urokinase, and t-PA) lyse blood clots (thrombi) and are, therefore, useful in the treatment of stroke.