Primary Motor Cortex
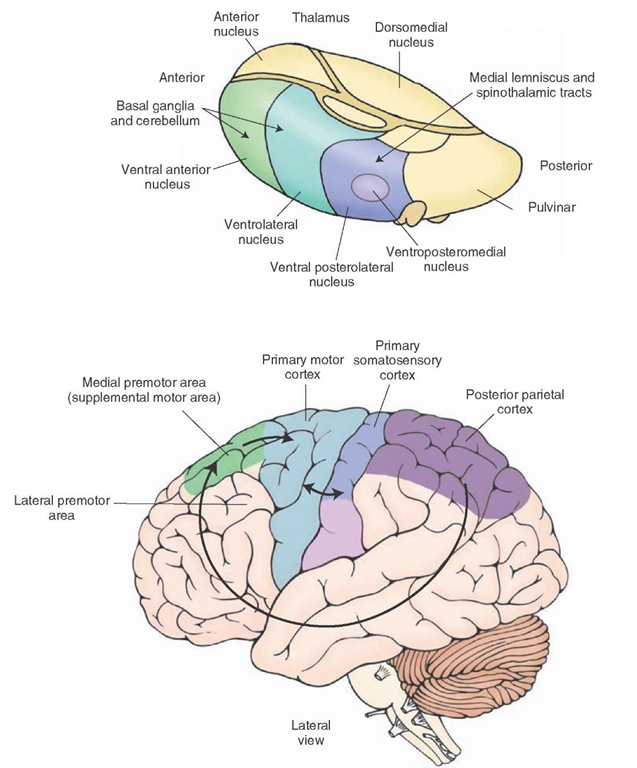
The primary motor cortex receives indirect inputs from several important regions that are known to regulate motor activity. These include the cerebellum and globus pallidus. Each of these regions projects to the primary motor cortex via a relay in the ventrolateral nucleus (VL) of the thalamus (Fig. 19-6). These inputs do not converge upon the same cells within the VL, but instead project to different parts of the nucleus. Thus, the integration of all of these inputs occurs within the primary motor cortex rather than in the thalamus. Other studies conducted in monkeys have shown that a purposeful movement is preceded by the discharge of neurons within the basal ganglia and cerebellum, which occurs prior to neuronal discharges in the motor cortex. The neuronal discharges in the motor cortex also precede the motor response. These kinds of observations suggest that the cerebellar and basal ganglia inputs provide the motor cortex with a planning mechanism for the initiation and regulation of a given response pattern.
The primary motor cortex also receives somatosensory afferents. The somatosensory inputs are organized in such a manner that enables a given region of motor cortex to receive proprioceptive and tactile inputs that relate to the specific muscle groups or body parts to which the neurons in that region of motor cortex relate functionally. For example, a group of cells in the motor cortex that relate to movement of specific muscle groups of the leg will, in turn, receive proprioceptive and tactile inputs from that part of the leg. Such inputs to a specific site within the primary motor cortex likely come indirectly from a thalamic relay nucleus, such as the ventral posterolateral nucleus (VPL), which is somatotopically organized, through a region of the primary somatosensory cortex that represents the same part of the body as the region of motor cortex to which it projects. This anatomical arrangement thus provides the basis for a second property of MI neurons, namely, that they discharge in response to movement. Moreover, the neurons in the cortex that respond to the action of a given muscle group are located in slightly different regions and lie close to neurons that relate to other muscle groups. Nevertheless, the neurons all generally lie within the region associated with that part of the body. Therefore, it is likely that the cortical neuronal discharge patterns indicate that the cells are responding to the synergistic actions of groups of muscles rather than to isolated muscle contractions of an individual muscle. Thus, when viewed collectively, the combination of signals from the basal ganglia, cerebellum, and sensory pathways provides the necessary inputs by which MI can produce a precise response of the appropriate force.
The fibers of the primary motor cortex project to the ventral horn at all levels of the cord but project most prominently to the lumbar and cervical levels. The corti-cospinal neurons make synaptic contact mainly with short interneurons that synapse upon alpha and gamma motor neurons in that region. Thus, activation of descending fibers of the primary motor cortex can directly produce muscle contractions of individual muscles as well as control the spindle mechanism associated with the tone of those muscles.
Primary Somatosensory Cortex
The key inputs to the primary somatosensory cortex are from the VPL of the thalamus, which receives its afferent supply from the dorsal column-medial lemniscal system and spinothalamic pathways (Fig. 19-6). These inputs involve conscious proprioception, position sense, pain, and tactile information. However, as noted earlier, descending pyramidal tract fibers originating from somatosensory cortex project to sensory regions and not to motor neurons. The primary projection targets include the cells of the dorsal horn of the spinal cord and the dorsal column nuclei of the lower medulla.1
FIGURE 19-6 Principal afferent projections to the motor cortex. Note that the cerebellum and basal ganglia gain entry into the motor and premotor cortices via connections with the ventrolateral and ventral anterior thalamic nuclei. This diagram also illustrates several key corticocortical connections that are essential for motor functions of the cerebral cortex. These include connections from the posterior parietal cortex (areas 5 and 7) to the premotor and supplementary motor cortices, connections from area 6 (supplementary and premotor cortices) to the primary motor cortex (area 4), and connections from the primary somatosensory cortex (areas 3, 1, and 2) to the primary motor cortex.
What is the significance of these descending fibers? The answer to this question resides in the fact that sequences of movements require the transmission of "positive" sensory feedback to the regions of motor cortex associated with those movements. What do these signals signify? Basically, they are involved in the regulation of sensory transmission through the nuclei of the dorsal columns and may respond to one or more of the following aspects of movement: (1) alteration of the position of the limb, (2) rate of change of the position of the limb, (3) magnitude of the muscular contraction in relation to the force exerted upon an object, and (4) a combination of force as well as rate of change.
Consider for a moment what the effect would be if, while attempting to walk, there was a loss of sensation concerning the position of either foot at any point in time. Under these circumstances, there would be a significant loss of precision to those movements. They would become awkward and ataxic. This, indeed, does occur with lesions involving the dorsal columns.The important point to remember here is that transmission of appropriate positive (sensory) feedback signals to the region of motor cortex associated with that movement requires the simultaneous filtering of other irrelevant sensory signals. Such filtering takes place at the levels of the dorsal column nuclei and dorsal horn by the inhibitory actions of the descending corticospinal fibers that arise from somato-sensory cortex. Loss of this inhibitory feedback mechanism would deprive the cortical motor neurons in question from responding appropriately to the positive feedback signals.
Supplementary and Premotor Area Cortices
Area 6, which contributes 30% of the fibers to the corti-cospinal tract, consists of two secondary motor regions: the SMA and the PMC. There are several highly significant inputs to these regions that should be noted. The first input is from the basal ganglia, which is directed mainly to the SMA. The primary route for this input to the cortex is through the thalamic nuclei (Fig. 19-6). Although some of the data obtained from various studies remains in conflict, the overall patterns seem to indicate that portions of both the VL and ventral anterior (VA) nuclei of thalamus, which receive inputs from the basal ganglia, project to area 6. Another source of inputs into area 6 includes the cerebellum. Here, cerebellar efferent fibers first synapse upon relay neurons in the VL, which then relay these signals primarily onto the PMC. A third source of inputs is the posterior parietal cortex (PPC). This region of cortex provides integrated somatosensory and visual information to area 6, which is necessary for the programming of motor sequences. Details concerning the posterior parietal cortex are described in the next section.
The most significant functional aspect of the SMA is its role in coordinating voluntary movements. It governs postural adjustments, and the associated deficits that occur after damage to this region are further evidence of its role in motor functions. Electrical stimulation of the supplemental (as well as premotor) cortex requires higher currents for the elicitation of motor responses. The motor responses are of a more complex pattern than those elicited from the primary motor cortex. Motor cortex stimulation frequently produces discrete twitching of one or several muscle groups. In contrast, stimulation of the supplementary and premotor cortices can elicit postural adjustments, body orientation, or closing or opening of the hands. The responses may be unilateral or bilateral.
The SMA can affect both the axial and the distal musculature through at least two important projections. This region of cortex controls the distal musculature by virtue of its projections upon primary motor neurons of area 4 (primary motor cortex). Its influence upon the axial musculature is by descending axons of neurons of the SMA found in the corticospinal tract that affect (through an interneuron) motor horn cells located in the ventromedial aspect of ventral gray of the spinal cord.
Patients who have lesions of the SMA display apraxia. Apraxia refers to the inability to initiate specific, purposeful movements, even though the sensory and motor pathways for the execution of the movement remain intact. There are several different types of apraxia. One type of apraxia is called ideomotor apraxia. It refers to the inability to execute a movement upon request. An example is the failure of a patient to be able to brush his or her hair or tie his or her shoelaces. Ideational apraxia is the inability to conceptualize the movements, and the patient is unable to identify the sequences of movements that are necessary for carrying out the response in question. Commonly, the apraxia becomes evident when the patient is asked to perform, simultaneously, different movements of both arms. On the other hand, if asked to perform the same sequence of movements with both arms simultaneously, the patient is often successful.
In a manner similar to that described earlier for the SMA, neurons of the PMC can activate, both directly and indirectly, spinal cord neurons that supply the axial and distal musculature. Corticospinal fibers arising from the PMC innervate medial and lateral ventral horn cells, directly or indirectly, by descending fibers that supply reticulospinal fibers.Recall that those neurons located medially in the ventral horn of the spinal cord innervate the axial musculature, and neurons located laterally innervate the distal musculature.
The premotor area plays an important role in movements that require visual guidance. Here, the inputs from the PPC are essential. Lesions of the PMC in humans can produce apraxia (similar to the apraxia described in the next section with lesions of the PPC). With lesions of the PMC, the patient is unable to coordinate the movement of both arms at the same time. In addition, the patient may also have loss of strength in the proximal muscles of the contralateral arm or leg and have difficulty in raising or abducting that limb.
Role of the Posterior Parietal Cortex
As indicated earlier, an important source of inputs to area 6 is derived from the PPC (areas 5 and 7 [Figs. 19-2 and 19-6]). Somatosensory inputs from the postcentral gyrus as well as vestibular inputs are directed to area 5, whereas area 7 is concerned with visual signals. In addition, area 7 receives inputs from area 5, thus indicating that this region of the cortex integrates both somatosensory as well as visual signals.
Different groups of neurons located in the PPC discharge in response to exploratory hand movements or in preparation for a goal-directed response such as reaching out to grab an object. Appropriate movements used for a given motor task require that an individual pay attention to the spatial arrangements of the objects in his or her visual field and to integrate that information with proprio-ceptive and other somatosensory signals. It is generally believed that the posterior parietal area carries out this function.
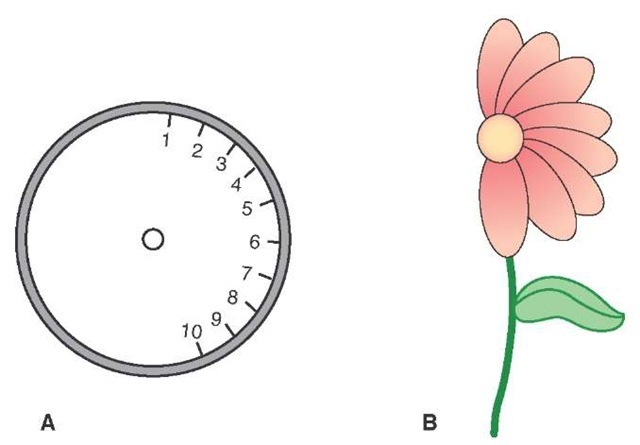
Perhaps the most interesting findings concerning functions of the posterior parietal area come from the clinical literature. Patients with lesions of the right PPC show two types of disorders. The first is apraxia. The second type of disorder is called sensory neglect (or anosognosia). In this disorder, the patient denies the disease condition or is unaware of it. For example, a patient with a right hemispheric lesion may deny or ignore the fact that he or she cannot move his or her left leg. Moreover, if this patient is asked to draw the numbers on a clock, he or she will draw them all on the right-hand side of the clock, while ignoring the left-hand side (Fig. 19-7).
Collectively, the physiological and clinical findings suggest the PPC executes an important function in motor activities. This function is to generate integrated somato-sensory and visual inputs to area 6, which provides the programming mechanism for the execution of complex motor responses.
Summary of the Components and Functions of the Corticospinal Tract
There are three principal components of the corticospinal tract. The first includes those fiber bundles that arise from the primary motor cortex (area 4). This pathway is responsible for voluntary control over precise movements that affect primarily (but not exclusively) the distal musculature. The actions of this fiber system are upon the ventral horn cells (via short interneurons) at all levels of the spinal cord. Appropriate neuronal responses in the primary motor cortex are heavily dependent on feedback signals from several regions. These include ascending inputs that signal the position of the distal musculature related to the movements associated with the primary motor cortical regions in question as well as other messages from the basal ganglia and cerebellum.
FIGURE 19-7 Drawings made by a patient with a lesion of the right posterior parietal cortex, indicating sensory neglect on the left side. The patient was asked to fill in numbers on the face of the clock (A) and to draw a flower (B).
The second component involves fiber pathways that arise from the primary somatosensory cortex (areas 3, 1, and 2) that project to the dorsal column nuclei and dorsal horn of the spinal cord. The purpose of this component is to serve as a sensory filtering mechanism. This mechanism allows specific sensory signals, such as the position of a limb or digit of the hand and the force of contraction of a muscle or group of muscles, to reach the relevant regions of the primary motor cortex while preventing sensory signals irrelevant to the movement in question from reaching the cortical neurons critical for that response sequence. This mechanism likely operates by providing excitatory foci and inhibitory surrounds (analogous to the visual system) with respect to different motor neurons within area 4.
The third component includes area 6, the supplementary and premotor cortices, which serve to provide the programming mechanism for the sequencing of response patterns that are essential for producing movements, such as lacing up one’s shoes and walking. These regions of area 6 project directly to the spinal cord and send signals to the primary motor cortex. In this way, the actions of the descending pathways upon different groups of neurons within the ventral horn of the spinal cord are synchronized with the actions of area 6 neurons upon the primary motor cortex. Finally, the actions of area 6 neurons can only occur if they receive integrated somatosensory and visual signals from the PPC (areas 5 and 7).
The Corticobulbar Tracts
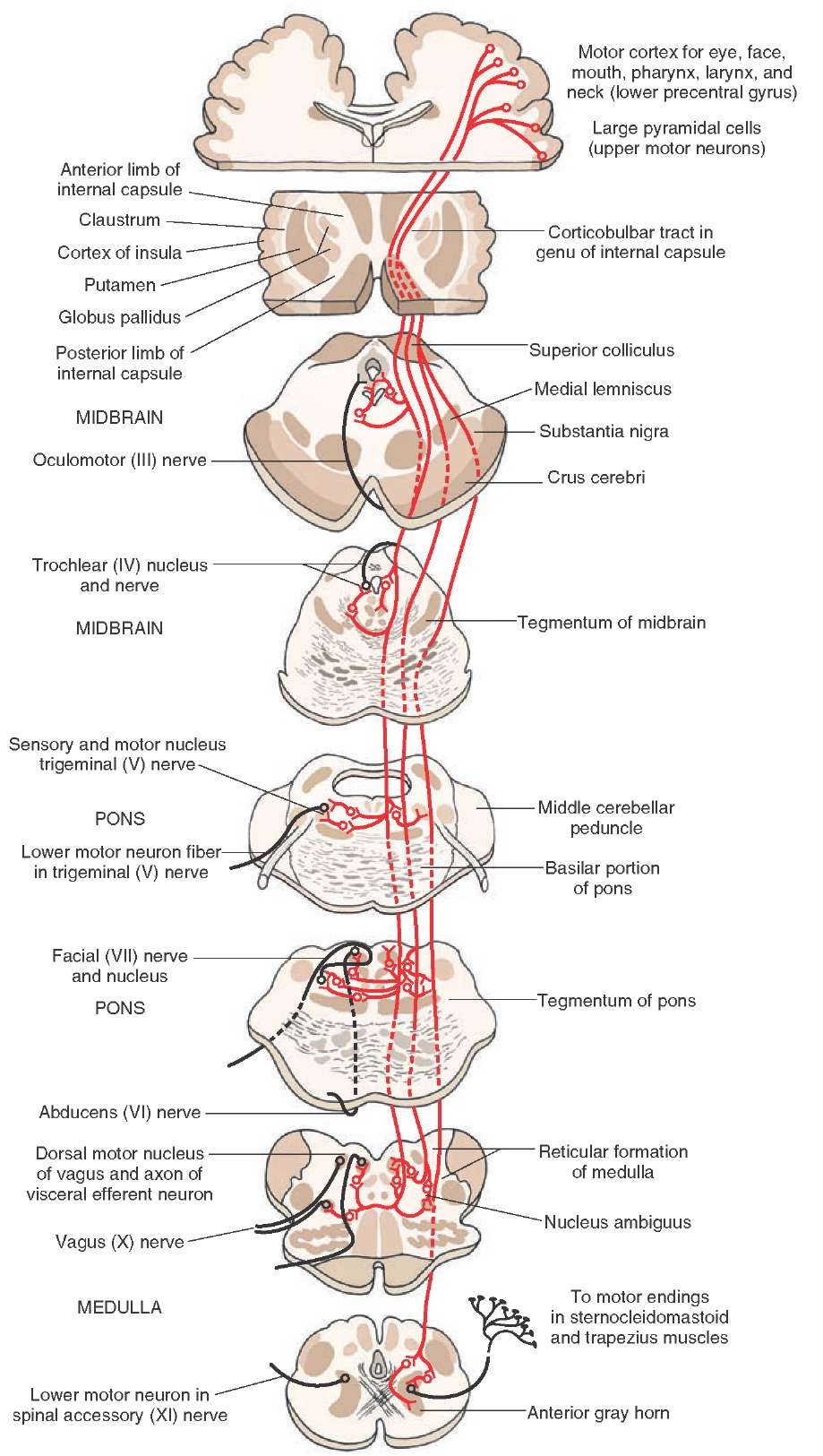
The corticobulbar tracts arise from the lateral aspect of the primary motor cortex (i.e., depicted as the head or face region in Fig. 19-3) and function in a similar manner to the corticospinal tract. Essentially, these descending fibers of the corticobulbar tracts serve as upper motor neurons to the cranial nerve motor nuclei onto which they make syn-aptic contact. They closely follow the descending trajectory of the corticospinal tracts (Fig. 19-8) and make direct or indirect synaptic contact (via interneurons in the retic-ular formation) with all motor cranial nerves (Fig. 19-8). These upper motor neurons thus serve as the anatomical substrate for voluntary control of the muscles of facial expression, eye movements, jaw opening and closing, and movements of the tongue.
However, there are several differences between the corticobulbar and corticospinal tracts that should be noted. The first is that most corticobulbar fibers that are directed toward cranial nerve motor nuclei innervate these neurons bilaterally.The exceptions include contralateral innervation of ventral cell groups of the motor nucleus of cranial nerve (CN) VII, which supply muscles of the lower quadrants of the face (below the eyes), such as the orbicularis oris muscle, and the hypoglossal nucleus (CN XII), which supplies the genioglossus muscle. It is also widely believed that the supranuclear innervation of the neurons of the spinal accessory nerve (CN XI) is mainly contralateral.
FIGURE 19-8 Projections of corticobulbar fibers to motor nuclei of cranial nerves.
Lesions of Corticobulbar Fibers That Supply Nuclei of Cranial Nerves
As indicated earlier, most of the inputs to motor nuclei of cranial nerves from the motor cortex are bilateral. A lesion of the cortex will not produce a paralysis of the muscles of the face and head. Instead, it will produce mild forms of weakness in the affected muscles (referred to as central facial palsy). Weakness in muscles that regulate breathing, swallowing, speech, and chewing is referred to as pseudobulbar palsy. If the lesion involves only the corti-cobulbar fibers and not corticospinal neurons, then there would be no paralysis of the upper or lower extremities. Because the neurons that innervate the muscles of facial expression of the lower quadrants of the face and those that affect protrusion of the tongue receive mainly a con-tralateral input, damage to the upper motor neurons will result in a more marked weakness involving the affected muscles on the side contralateral to the lesion. Such effects are manifested by a deviation of the jaw and tongue (upon protrusion) to the side contralateral to the site of the lesion. Similarly, damage to the corticobulbar fibers projecting to the hypoglossal nucleus will produce a deviation of the tongue to the side opposite the lesion.
Other Projections of the Corticobulbar Tracts
To Sensory Relay Nuclei
As noted earlier, one of the components of the corticospi-nal tract arises from areas 3, 1, and 2 (the primary somatosensory cortex situated on the postcentral gyrus). Many of the fibers project to the dorsal horn, and others project to dorsal column nuclei. Both groups of fibers essentially perform the same functions; namely, they serve to filter the flow of sensory information to the sensorimotor cortex. However, as previously indicated, the projections from areas 3, 1, and 2 to the dorsal column nuclei, strictly speaking, are corticobulbar fibers. Other fibers from somatosen-sory cortex project to the sensory nuclei of the trigeminal system. These fibers also function in a parallel manner to the descending cortical fibers that supply the dorsal horn and dorsal column nuclei. The projection to the sensory trigeminal nuclei serves as a filtering mechanism for sensory inputs associated with the head region.
Corticoreticular Fibers
Considerable quantities of corticoreticular fibers that arise from the sensorimotor cortex (i.e., the precentral, postcentral, and premotor cortices) also project to different regions of the reticular formation of the brainstem. Although these projections are relatively extensive, there are several projections that should be noted. Fibers originating from the precentral gyrus project to neurons of the pons and medulla, which give rise to descending bundles that comprise reticulospinal fibers (i.e., the lateral and medial reticulospinal tracts).Other groups of fibers of the sensorimotor cortex project to the paramedian and reticu-lar nuclei of the reticular formation of the pons and medulla, respectively, which supplies the cerebellum. These projections thus enable the cortex to provide additional influences on motor functions at the levels of both the spinal cord and cerebellum. Still other groups of cortical fibers project to regions of the reticular formation that give rise to long ascending fibers to the forebrain. One of the functions of the long ascending fiber projections of the reticular formation is to produce cortical arousal.The cortical projections to the regions that give rise to these ascending projections may provide the anatomical basis for a feedback mechanism for the regulation of cortical arousal functions.
Cortical Projections to the Red Nucleus
Studies, based mainly on cats, have shown that fibers that arise from the primary and premotor cortices also project ipsilaterally to the red nucleus. This projection is soma-totopically organized. Fibers from the upper limb region of the precentral gyrus project to the dorsal part of the red nucleus, whereas fibers from the lower limb region of the precentral gyrus project to the ventral aspect of the red nucleus. The dorsal and ventral regions of the red nucleus project to the cervical and lumbar regions of the spinal cord. Thus, the projection to the red nucleus represents still another way by which the cerebral cortex can control motor functions of the spinal cord. Functions of this system are described in the "Rubrospinal Tract" section. However, in humans, it is believed that the descending projections of the red nucleus to the spinal cord (i.e., rubrospinal tract) are considerably diminished, with few fibers descending beyond the cervical level.