Lesions of the Spinal Cord
Spinal Cord Transection
A complete transection of the spinal cord results in loss of muscle tone, motor function, reflex activity, visceral sensation, and somatic sensation below the level of the transection. Immediately after the spinal cord damage, there is a period during which all spinal reflexes below the level of transection are attenuated or absent. This condition is called spinal shock and results from a sudden interruption of descending excitatory influences on the spinal cord. Bladder and bowel function are also impaired because of the disruption of autonomic reflexes of these organs. In humans, spinal shock lasts for about 1 to 6 weeks. Then, slow recovery of neural function occurs: First, minimal reflex activity with a Babinski sign appears; next, flexor spasms are observed, which are then followed by alternate flexor and extensor spasms and the appearance of predominant extensor spasms.
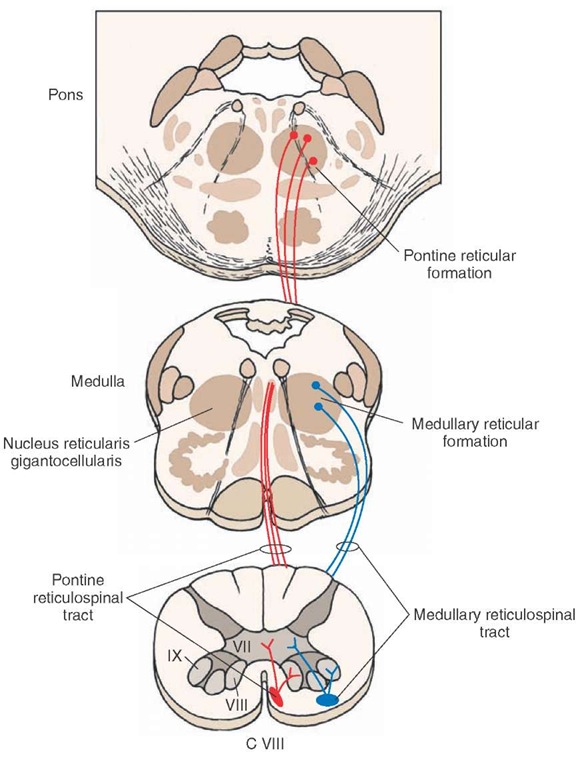
FIGURE 9-15 Reticulospinal tracts. The medullary (lateral) reticulospinal tract (shown in blue) arises from the nucleus gigantocellularis and projects bilaterally to all levels of the spinal cord (only ipsilat-eral projections are shown). The pontine (medial) reticulospinal tract (shown in red) arises from the pons and projects ipsilaterally to the entire extent of the spinal cord. C = cervical.
Brown-Sequard Syndrome
Brown-Sequard syndrome involves a hemisection of the spinal cord. The primary characteristic is the dissociation of function between conscious proprioception and pain and temperature sensations. Loss of conscious proprioception and two-point discrimination occurs below the level of the lesion on the ipsilateral side, and loss of pain and temperature sensation occurs one or two segments below the level of the lesion on the contralateral side as well as bilaterally.
There is also an upper motor neuron paralysis below the level of the lesion on the ipsilateral side and a lower motor neuron paralysis at the level of the lesion on the ipsilateral side. This kind of incomplete transection may occur by fracture dislocation of vertebrae, tumor, or missile wounds.
Amyotrophic Lateral Sclerosis (Lou Gehrig’s Disease)
Amyotrophic lateral sclerosis (ALS) is a progressive degenerative disease in which the corticospinal tracts (upper motor neuron) and ventral horn cells (lower motor neuron) degenerate, often beginning with the lower limbs and later involving the upper limbs. Degeneration of the ventral horn cells in the cervical spinal cord results in weakness and, ultimately, in loss of control in muscles of the hand, trunk, and lower limbs. Involuntary twitching of muscle fascicles (fas-ciculations) occurs in these muscles. Bladder and bowel functions are also impaired due to the loss of descending autonomic pathways. The cause of this disease is not known.
Syringomyelia
This disease is due to a developmental or acquired abnormality and is characterized by an expansion of the central canal of the spinal cord.Such expansion produces proliferation of glial cells in this region, especially at the levels of the lower cervical and upper thoracic cord. In this condition, there is a segmental loss of pain and thermal sensation because there is an interruption of crossing fibers of the spinothalamic tracts in the same and adjoining segments at the level of the lesion. Because tactile sensation is largely preserved, while pain and thermal sensation is lost, it is another example of "dissociated sensory loss."
Tabes Dorsalis
Tabes dorsalis represents late consequences of syphilitic infection of the nervous system and is also referred to as tertiary syphilis or neurosyphilis. In this syndrome, the large diameter central processes of the dorsal root ganglion neurons (primary afferent sensors) degenerate, especially in the lower thoracic and lumbosacral segments. Therefore, the fibers in the fasciculus gracilis degenerate, and there is a loss of vibration sensation, two-point discrimination, and conscious proprioception. The loss of conscious proprioception results in ataxia (uncoordinated muscular movements) because the patient is now deprived of the "conscious" sensory feedback of signals that detect the position of the lower limbs at any given point in time.
Multiple Sclerosis
Combined Systems Disease
Combined systems disease results from a deficiency of enzymes necessary for vitamin B12 absorption. Deficiency of vitamin B12 results in pernicious anemia as well as degenerative changes in the dorsal and lateral funiculi of the spinal cord. These patients have defects in both sensory and motor function. The symptoms of sensory loss include tingling and the loss of senses of vibration and position. Disturbance in motor function includes upper motor neuron dysfunction. This may include a weakness of the lower limbs and an ataxic gait.
Lesions of the Dorsal Root
Section of three consecutive dorsal roots causes abolition of all sensory function in a particular dermatome (anesthesia of the dermatome); section of one dorsal root does not cause much sensory loss because of overlap between der-matomes that are associated with intact dorsal roots and those that are damaged. With muscle tone also dependent on segmental reflexes, interruption of the afferent limb of these reflexes caused by the section of a dorsal root results in loss of muscle tone innervated by the affected segment.
Lesions of the Ventral Root
These lesions abolish motor functions of the muscles innervated by the affected segment. For example, section of the ventral root of C8 will result in paralysis of the muscles of the hand. Similarly, section of thoracic ventral roots will result in disturbances in the function of visceral organs innervated by them.
Spinal Reflexes
A spinal reflex involves discharge of an efferent motor neuron in response to afferent stimulation of sufficient intensity. Spinal reflexes are modulated by supraspinal mechanisms. However, when continuity of supraspinal pathways is interrupted (e.g., by damage to the spinal cord), the spinal reflexes remain intact below the level of the lesion and are often exaggerated. Clinically, symptoms of motor dysfunctions can be readily identified by testing the integrity of spinal reflexes. The neural mechanisms involved in different important spinal reflexes are summarized in the following sections.
Myotatic Reflex
Receptors
The myotatic reflex (also called stretch or deep tendon reflex or knee-jerk response) is the basis of the knee-jerk response routinely tested in neurologic examinations. The primary receptor involved in the initiation of the myotatic reflex is the muscle spindle. Muscle spindles are present in all skeletal muscles with a few exceptions (e.g., the muscles in the middle ear). Each spindle consists of a connective tissue capsule in which there are 8 to 10 specialized muscle fibers called intrafusal fibers.The intrafusal fibers and the connective tissue capsule in which they are located are oriented parallel to the surrounding larger skeletal muscle fibers called extrafusal fibers, which are involved in the movement of the limb. In larger intrafusal muscle fibers, the nuclei are located in the center of the fiber. These fibers are called the nuclear bag fibers. In other intrafusal fibers, the nuclei are arranged in a single file. These fibers are called nuclear chain fibers. Fast-conducting, large myelinated axons (called Group Ia afferents) encircle the middle of both types of intrafusal fibers, and these axon terminals constitute the primary sensory ending of the spindle. Group II afferent axons provide the secondary sensory innervation to the intrafusal fibers. The intrafusal fibers contract when gamma motor neurons are activated because these fibers are innervated by the spinal gamma motor neurons.
Circuitry and Mechanisms
A schematic representation of the circuitry involved in the myotatic reflex is shown in Figure 9-16. The mechanism of muscle contraction in response to its stretching is summarized as follows using the quadriceps muscle (extensor) as an example. When a quick tap is delivered to the patellar tendon, the quadriceps muscle is stretched briefly, the intrafusal fibers in the muscle spindle are deformed briefly, and action potentials are initiated by activating mechanically gated ion channels in the afferent axons coiled around the intrafusal fibers, resulting in a volley of discharge in group Ia afferent fibers emerging from the spindle.These fast-conducting afferent fibers synapse directly on alpha motor neurons in the spinal cord, which innervate extrafusal muscle fibers of the same muscle in which the muscle spindle is located (homonymous muscle). The impulses conducted through the Ia afferent fibers result in excitation of alpha motor neurons, which, in turn, elicit contraction of the homonymous muscle (quadriceps in this case) causing extension of the leg. Thus, the myotatic reflex is monosynaptic and involves a two-neuronal arc consisting of the Ia fiber from the stimulated muscle spindle and the alpha motor neuron that innervates the homonymous muscle. Note that this reflex is of short duration because of the inhibitory action of the Renshaw cell on the alpha motor neuron (see Fig. 9-4B).
FIGURE 9-16 Myotatic reflex. When a quick tap is delivered to the patellar tendon, the quadriceps muscle is stretched, and the reflex response is a contraction of the homonymous muscle (quadriceps in this case). In the myotatic reflex, there is reciprocal inhibition of the antagonist muscle (heteronymous muscle).
Reciprocal Inhibition in the Myotatic Reflex
Group Ia fibers from a muscle spindle also make an excitatory synapse with an inhibitory interneuron in the spinal cord, which, in turn, makes an inhibitory synapse with an alpha motor neuron innervating the antagonist (heteronymous) muscle (Fig. 9-16). An antagonist muscle is one that controls the same joint but has an antagonistic mechanical function. For example, an extensor has an antagonistic action to that of a flexor. Thus, activation of group Ia muscle spindle afferents causes contraction of homonymous muscles while producing reciprocal inhibition of antagonist muscles. The end result of this process is to resist the changes in muscle length through a negative feedback loop.
Inverse Myotatic Reflex
A schematic representation of the circuitry involved in the inverse myotatic reflex is shown in Figure 9-17. The Golgi tendon organ is another sensory receptor that plays an important role in regulating the motor unit activity. It is located in the tendon of the muscle.The Golgi tendon organ is a high-threshold receptor that senses tension of the muscle; the muscle spindle, which has a much lower threshold, senses length of the muscle. Contraction of the muscle or stretching of the muscle (e.g., in whole-limb movement) constitutes the sufficient stimulus required for activation of the Golgi tendon organ. Activation of the Golgi tendon organ produces a volley in the associated afferent fiber (Ib fiber). This afferent fiber makes an excitatory synapse with an interneuron that inhibits the alpha motor neuron that innervates the homony-mous muscle group. The net effect is that the period of contraction of the muscle in response to a stretch is reduced. This type of response (i.e., reduction of contraction of homonymous muscle) elicited by stimulation of Golgi tendon organs is referred to as the inverse myotatic reflex.
FIGURE 9-17 Inverse myotatic reflex. Contraction of the muscle or stretching of the muscle (e.g., in whole-limb movement) activates the Golgi tendon organs, and a volley of discharge is produced in the Ib fibers. Inhibitory interneurons are excited and alpha motor neurons innervating the homonymous muscle group are inhibited; the result is a reduction in the period of muscle contraction.
Resetting of the Muscle Spindle Through the Gamma Loop
Gamma motor neurons, located in the ventral horn of the spinal cord and intermingled among alpha motor neurons, constitute lower motor neurons because they innervate skeletal muscle. As stated earlier, gamma motor neurons innervate the polar ends of intrafusal muscle fibers. Their activation produces contraction of the intrafusal muscle fibers at their polar ends, which results in stretching of the muscle spindle in the middle, causing the spindle to discharge. Thus, the primary function of the gamma motor neuron is not to cause the direct contraction of the extrafusal muscle but to reset the spindle mechanism and increase the likelihood of discharge of Ia afferent fibers. In this manner, the gamma motor neurons indirectly lead to contraction of the extrafusal muscle fibers because of their actions upon the spindle mechanism, which results in reflex activation of alpha motor neurons.
Modulation of Muscle Tone by Gamma Motor Neurons
It is also important to point out that the gamma motor neurons are under supraspinal control. Descending motor fibers principally from the reticular formation (i.e., the lateral and medial reticulospinal tracts) but also from other regions, such as the cerebral cortex and lateral vestibular nucleus, can modulate muscle tone by exciting or inhibiting gamma motor neurons. For example, excitation of gamma motor neurons by the medial reticulospinal tract causes an increase in muscle tone and a general facilitation of the stretch reflex. Conversely, activation of the lateral reticulospinal tract causes inhibition of gamma motor neurons and subsequent inhibition of the stretch reflex. In general, the descending motor fibers function in concert in order to constantly regulate muscle tone by providing converging inputs onto gamma motor neurons.