Abstract
It is paradoxical that, although several major technological discoveries such as Magnetic Resonance Imaging and Nuclear Medicine and Digital Radiology, which facilitate improvement in patient care, have been satisfactorily embraced by the medical community, this has not been the case with Healthcare Informatics. Thus, it can be argued that issues such as Data Management, Data Modeling, and Knowledge Management have a long way to go before reaching the maturity level that other technologies have achieved in the medical sector. This topic proposes to explore trends and best practices regarding knowledge management from the viewpoint of performance management, based upon the use of Key Performance Indicators in healthcare systems. By assessing both balanced scorecards and quality assurance techniques in healthcare, it is possible to foresee an electronic healthcare record centered approach which drives information flow at all levels of the day-to-day process of delivering effective and managed care, and which finally moves towards information assessment and knowledge discovery.
Introduction
The advantages of the introduction of Information and Communication Technologies (ICT) in the complex Healthcare sector have already been depicted and analyzed in the Healthcare Informatics bibliography (Eder, 2000; Englebardt & Nelson, 2002; Harmoni, 2002; Norris, Fuller, Goldberg, & Tarczy-Hornoch, 2002; Shortliffe, Perreault, Wiederhold, & Fagan, 2001; Stegwee & Spil, 2001). It is nevertheless paradoxical that, although several major technological discoveries such as Magnetic Resonance Imaging, Nuclear Medicine and Digital Radiology, which facilitate improvement in patient care, have been satisfactorily embraced by the medical community, this has not been the case with Healthcare Informatics. Thus, it can be argued that issues such as Data Management, Data Modeling, and Knowledge Management have a long way to go before reaching the maturity level that other technologies have achieved in the medical sector.
A variety of reasons could be proposed for this issue, though with a short analysis it becomes rather clear that modern ICT present integration problems within the healthcare sector because of the way the latter is organized. Healthcare is a strongly people-centered sector in which ICT has been considered more as an intruder, as a “spy” to the healthcare professionals’ way of doing things and as a competitor to this people-centered model. Thus, if ICT intend to prove its advantages towards establishing an information society, or even more a knowledge society, it has to focus on providing service-oriented solutions. In other words, it has to focus on people and this has not been the case in most of the circumstances. It is common knowledge that in order to install any type of information system in healthcare, especially if it involves knowledge management, six main groups of issues have to be dealt with (Iakovidis, 1998, 2000):
1. The organizational and cultural matters related to healthcare. This issue is rather important, regardless of any information system, since organizational models and culture do not endorse the continuity of care or any type of structured data collection.
Issues such as mistrust between different specialists, between the different healthcare structures or between doctors and nurses prevent in many cases the effective sharing of information. Health reforms are currently under way in many countries stressing the will to deal with this problem.
2. The technological gap between healthcare professionals and information science experts. Doctors are often reluctant to use information systems that they believe are not designed for them. From another point of view, Healthcare Informatics have been introduced in healthcare institutions mostly on pilot-based projects aiming at addressing specific issues and have proposed solutions addressing a small number of healthcare practitioners, resulting in establishing a complex map of information niches. This approach is the consequence of applying information technology to procedures that where not designed for it, thus creating a panspermia of information models which are neither compatible nor interoperable, even within a single institution’s environment. Efforts in creating interoperability standards and protocols such as HL7 are proposing solutions to address this issue, thus enabling data manipulation and knowledge management.
3. The legal requirements on the confidentiality of personal and patient related data and on data privacy. It is clear that if this issue is not addressed at a managerial and procedural level by imposing suitable policies to meet these requirements, there is little chance that medical data will be kept digitally in a structured manner (thus allowing the transition from digital islands of clinical data towards a structured electronic healthcare record). The implementation of an information system, where the electronic healthcare record is considered to be the core of the system (patient-centered model), is the only way to drive data management towards creating new knowledge. The complexity of the problem can be explained if one just observes the course of implementation of both the Health Information Privacy and Accountability Act (HIPAA) in the US and Directive 95/46/EC in the EU. The issues seem to have been dealt with at the strategic level, but still a lot has to be done in the implementation and setup of those strategies.
4. The industrial and market position of Healthcare Informatics. In general, the healthcare market is seen by the industry as large in size but not highly profitable, mainly due to the lack of standards in implementing and interoperating healthcare informatics products. As a consequence, the industry has focused on creating mostly small-scale products (i.e., Laboratory Information Systems, Radiology Information Systems, Clinical Information Systems) and not on evangelizing the production of information system that are dealing with healthcare as a whole. The lack of end-to-end solutions is dealt with by interconnecting heterogeneous information systems (a rather complex task with constant change management issues) and by introducing solutions from other business sectors (i.e., ERP, SCM, CRM) that have often been rejected by “key users” as non-compliant with their job description. Nevertheless, the new Web technology approaches (Web services, XML, etc.) and the new information technology strategies (i.e., service oriented architecture) could be the drivers towards merging information technology and healthcare services and thus enabling the establishment of knowledge management products.
5. The lack of vision and leadership of healthcare managers and health authorities, and the lack of willingness to re-engineer healthcare processes for the benefits of efficiency and quality of care delivery. Some countries are in the process of introducing or implementing such Business Process Reengineering projects in order to address healthcare delivery in a more information flow conformant way. This is a key point in reaching knowledge management, knowledge re-use and sharing, and finally proposing a solution for the knowledge-based society of tomorrow. This issue should be dealt with by proposing strategies that focus on processes and by establishing key performance indicators, balanced scorecards, or other metrics that are the upper level of a structured information flow-based model. 6. User acceptability and usability of the proposed information systems. This issue is the one most strongly related to the problem of dealing with the people-centered approach of the healthcare sector. This issue deals with information systems’ user friendliness, with usability issues such as the time to reach a data entry point, the speed of information retrieval, the quality of information retrieval, the complex security procedures, and so on. In order to implement information systems and knowledge management systems, education and training must be addressed with high priority since user acceptability is strongly related to them. Service oriented models and patient-centered information systems have a higher chance of passing the user acceptability test. A system that is not accepted by the user is often a system with poor data quality (or no data at all) and knowledge management, business intelligence or data warehousing solutions are consequently inoperable and unsuccessful.
Taking all of the above issues into consideration, this topic proposes to explore trends and best practices regarding knowledge management from the viewpoint of performance management, based upon the use of Key Performance Indicators (KPI) in healthcare systems. By assessing both balanced scorecards (Kaplan/Norton) and quality assurance techniques in healthcare (Donabedian), it is possible to foresee an electronic healthcare record centered approach which drives information flow at all levels of the day-to-day process of delivering effective and managed care, and which finally moves towards information assessment and knowledge discovery (both with administrative and medical data). KPIs should be regarded as the strategic assessment tool, for both the executives and the clinical decision-makers, that will lead healthcare delivery to excellence and to knowledge discovery and assessment.
background
Knowledge Management as a Transformation Driver in Healthcare
Today, Knowledge Management (KM) is on everyone’s mind. Healthcare organizations are no exception and are accepting the challenge to more effectively share knowledge both internally and externally (Strawser, 2000). The growth of KM projects (i.e., decision support systems, data mining tools, business intelligence solutions) signals a growing conviction that managing institutional knowledge is crucial to business success and possibly business survival. When the hype and confusion are stripped away, it is apparent that KM initiatives can profoundly change a healthcare enterprise for the better, and bring numerous advantages to Healthcare Information Management (HIM) professionals. For HIM professionals, KM is worthy of special attention because it informs them not only on how to do things, but also on how they might do them better. In order for this to happen, data should be provided in specific patterns and should be based upon a strategy that will empower a healthcare system by gaining knowledge of its processes, its outcomes, and its structures.
Despite the obvious advantages, many healthcare decision makers view the idea of a KM initiative with scepticism, possibly because of an incomplete or incorrect understanding of the tools needed to achieve it. Many of the tools and strategies associated with implementing KM are not new; what is new is a cohesive approach to KM design and implementation. Certainly there are pitfalls and limitations in using information technology for KM—trying to force fluid knowledge into rigid data structures, for example, or focusing too much on the tools and not enough on the content. But networks and computers, with their ability to connect people and store and retrieve virtually unlimited amounts of information, can dramatically improve departmental efficiencies. Some examples of knowledge management applications are listed below:
• Data Mining tools enable decision makers to search and analyze large sets of data by using specific querying methods and tools (Standard Query Language, Rough Data set, On Line Analytical Processing).
• Document and Content Management systems are widely used to store and archive files of any type (text, images, video, etc.) and correlated them with keywords that have a business meaning to the end user.
• Knowledge Maps are graphical or other representations of how and by whom a specific set of information is created, distributed and assessed. Knowledge Maps are very important tools in Total Quality Management projects.
• Intelligent Agents use a combination of profiling techniques, search tools, and recognition algorithms to provide up to date specific information to the end user. For example, intelligent agents could be used to forward completed test results to the corresponding physicians of a patient.
• Web Browsers are the most commonly used tools for searching information in an intranet or the Internet. As such, Web browsers are increasingly becoming the most common graphical user interface, even for specific software products such as financial accounting and patient order entry systems.
• Business Intelligence tools and Data Warehouses enable the decision maker to have predefined access to specific information of interest regardless of the physical location of the data. Such systems are ideal for performance management and executive reporting and serve as the technological base for supporting the idea of a digital dashboard of indicators.
• Workflow applications play a very important role in KM since knowledge is created during the process-based operations that take place in a healthcare institution. A computerised patient order entry system is a classic example of a process-based operation in healthcare that requires the constant monitoring of the workflow status.
• E-learning and collaboration tools are part of the knowledge distribution process, which is extremely important in healthcare, since continuous education is a key factor in effective practice of care.
The essence of effective knowledge management does not rely on the use of one or more existing or forthcoming information technology tools. It is mostly about people, about processes and about capturing the results of people following processes, about transforming information into knowledge (explicit or tacit) and reusing it within a healthcare framework.
Performance Management: Monitor and manage Healthcare
In order to persuade healthcare decision makers to assess the added value of KM tools, the latter should initially be used to propose new performance measurement and performance management techniques at all levels of a healthcare system (Hurst & Jee-Hughes, 2001). In that sense, performance management has long been considered as a tool for controlling spending and for increasing the efficiency of healthcare systems (Oxley & MacFarlan, 1994). There are three broad goals that governments generally pursue in the healthcare area:
• Equity: where citizens should have access to some incompressible minimum level of healthcare and treatment based on the need for care rather that solely on income.
• Micro-economic efficiency: where quality of care and consumer satisfaction should be maximized at minimum cost.
• Macroeconomic cost control: where the healthcare sector should consume an “appropriate” share of GDP.
In addition, healthcare systems are often facing factors that put pressure on the system. As a consequence, an effective performance management framework is the only solution towards controlling factors such as:
• Population aging
• Increased income and higher demand for healthcare services;
• Increased access to healthcare services; and
• Increase of high technology usage which in turn increases the healthcare services usage creating sometime unnecessary demand (from a medical point of view).
Most existing policies for controlling the performance of healthcare systems were based upon financial assessment of past results (mac-roeconomic control of spending and micro-efficiency improvements) by giving incentives to payers and providers of a healthcare system. By its very nature the financial measurements are not forward looking and are exclusionary to non-financial measures. In addition, the emergence of the Information Society in the late 90s rendered many of the fundamental performance management assumptions obsolete. Information Society has brought a new set of assumptions that institutions have to include into their strategy. Amongst others we could refer to:
• The cross functional aspects of processes based upon specialisation, increased skills and high technology
• The integration of processes in the healthcare sector from the suppliers to the patient and the ability to manage and monitor materials upon requests and needs
• The ability to offer specific services to patients in accordance to their needs while being able to constraint costs of this customised care. In fact this is the essence of managed care: providing satisfactory and high quality of care at a reasonable cost.
• The global scale of healthcare: This sector is no exception to any other global marketplace, thus making healthcare delivery more comparable at a national or regional level and within accepted standards (e.g., clinical procedure guidelines)
• Innovation, which has been a key driver towards quality of care and quality of life for many years in the healthcare sector
• Knowledge workers: the increasing complexity of medicine and technology has created a need for highly skilled personnel at every level of a healthcare institution. Employee empowerment is driven by knowledge as it is created in the daily process of delivering healthcare services.
Nowadays, performance measurement is moving towards the adoption of a set of objectives for a healthcare system. To our knowledge, there is no complete agreement on what is meant by “performance” of health systems and many sets of objectives are generally proposed. The use of Key Performance Indicators (KPI) helps to establish this set of objectives more thoroughly by focusing on the real needs.
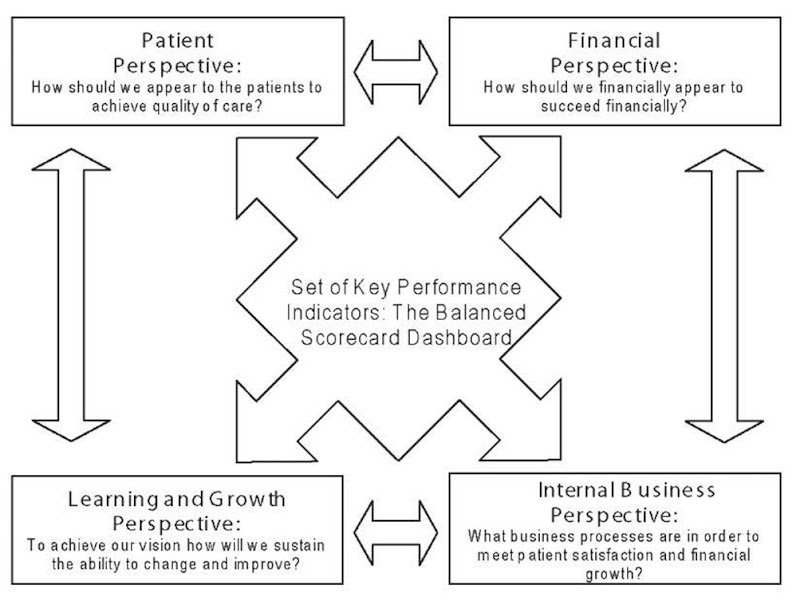
using Balanced scorecards
In order to address the issue of creating a set of KPIs , the Balanced Scorecard (BSC) framework (Kaplan, 2001; Norton & Kaplan, 1996) initially proposed by Kaplan and Norton for the strategic management of financial organizations in the mid 1990s, is one of the most suited approaches in that direction. This model has now proven its value and since it is a generic framework it is applicable to the healthcare sector. The BSC concept involves creating a set of measurements and objectives for four strategic perspectives:
• Financial: financial performance measures typically indicate whether a proposed strategy implementation and execution is contributing to bottom line improvements, based upon an accurate summary of economic consequences of actions already taken.
• Customer (i.e., the Patient): this perspective is a set of objectives that focuses on identifying the patient’s needs, the targeted market (this could be the case of a specialised institution) and on measuring the performance of each specific business unit (i.e., a department) that has some influence on how the patient sees the healthcare organization.
• Internal Business Process. This perspective should gather all objectives related to processes and the way these are monitored and fine-tuned in order to achieve both excellence in financial accomplishments and patient satisfaction. In that sense, the BSC approach is a constant business process reengineering process based upon specific goals to meet and not on improving de facto established processes.
• Learning and Growth (innovation and vision). This is an important perspective of a BSC implementation because it focuses on the objectives and goals to achieve the incorporation of business innovation (e.g., installing a Positron Emission Tomography Device) and the continuous education of medical and administrative staff. In that sense, this perspective identifies measurable tasks in order to build long-term growth and improvement. In the healthcare sector, improvement is also measured by assessing the outcome of treatment and care.
These four perspectives comprise a framework, meaning that they must be assessed and populated in accordance to each business case. In order to achieve this, one has to set for each category a list of objectives that can be feasibly measured. To each objective, a specific target should be set and the initiative to reach that target well described.
The BSC approach retains the “traditional” financial perspective, which mostly focuses on reporting about past events. Financial figures, even if prospected in the future by statistical means, are inadequate for guiding and evaluating the journey that healthcare institutions must make to create future value through innovation, knowledge, patient satisfaction, employee empowerment, process refinement, technology assessment and material management. In that sense, the three other cited perspectives are completing the puzzle in order to create a more valid and future-oriented performance management strategy. In recent years, there have been some implementations of BSC frameworks in the healthcare sector mostly on a single institution base (i.e., a hospital, a clinic, an information technology component). Readers are encouraged to read and assess the best practices, cited as references to this topic (Aidermark, 2001; Castaneda-Mendez, Mangan, & Lavery, 1998; Forgione, 1997; Freeman, 2002; Gordon & Geiger, 1999; Inamdar, Kaplan, & Bower, 2002; Oliveira J, 2001; Pink, Mc Killop, Schraa, Preyra, Montgomery, & Baker, 2001; Tarantino, 2003; Weber, 1999)
The model in Figure 1 enables decision makers to also value how the latter three perspectives have worked and thus it enables the measurement of intangible aspects of a system. The measurements focus on a single strategy that can be easily broken down to the various levels of depth, depending of the organization type. Thus, by using BSC one can create a top-to-bottom design of a system, starting up from the needed strategy (what is the market, who are the customers, what are the critical processes, what is required by the stakeholders) going down to design metrics, processes, structures and finally the needed technical and functional specification to create an information system and a knowledge management framework capable of producing the right data and serve the strategy.
Figure 1. A healthcare oriented BSC framework
Quality assurance in healthcare and the role of information technology
Known problems and Issues of the Healthcare sector
It is rather of common knowledge that the healthcare sector is not a sector without problems. Especially in Europe, the great majority of healthcare organizations are state funded. This means that institutions have in some cases very restricted budgets to satisfy their needs thus making performance management a critical issue in their daily routine. Other common problems are increased bed coverage (some institutions are almost at 100 percent), long length of stay, increased waiting lists, poor facilities, and so on. Taking all this into account and adding the life-related processes, one can clearly see that healthcare organizations are difficult to manage even for experienced managers of other sectors. One could list some of the major issues that healthcare stakeholders are confronted with:
• Diversity of cases
• Need of high technology medical devices
• Public Policy Restrictions (e.g., payment by per day quotas that do not cover the inpatient treatment costs)
• High lengths of stay
• Increased waiting times
• Obsolete facilities
• Restricted funds for training
• Restricted funds for maintenance
• Increased number of medical errors (sometimes fatal)
• Erroneous drug prescription and intake (sometime fatal)
• Geographical issues (too many patients, too few nurses and medical staff)
• Large lists of materials to be managed (more than 3000 on average)
• Excessive waste management (10 m3 per day on average)
Quality Assurance and performance Management
The application of a BSC framework will not by itself solve any of the aforementioned problems and issues. One could even say that BSC projects often fail as a consequence of misunderstanding or of not using a BSC strategy. BSC projects also fail because the variables of the scorecard are incorrectly identified as the primary drivers and because the improvement goals (the targeted objectives) are negotiated across an institution instead of being based upon stakeholders’ requirements, fundamental processes and improvement process capabilities. They also fail because there is no deployment system installed to disseminate, maintain and promote the BSC framework, or because some very important KPIs are not used, or metrics are poorly defined.
Furthermore in order to create a structure that can be monitored the KPIs should not be more that 10 for each perspective, while non financial metrics should overcome the financial metrics by approximately six to one (Schneiderman, 1999). In order to support any BSC framework, a deployment and maintenance system based upon quality assurance specially designed for Healthcare should be established. Traditionally in healthcare, Quality Assurance (QA) has been meant to apply predominantly to healthcare itself as provided directly to patients by legitimate healthcare practitioners. We also include other services that directly affect the ability of practitioners to perform well, meaning services such as radiology, pharmaceutical, laboratory, and patient admission. The basic quality assurance terms (Donabedian, 2003) are:
• Efficacy: the ability of the science and technology of healthcare to bring about improvements in health when used under the most favorable circumstances.
• Effectiveness: the degree to which attainable improvements in health are in fact attained.
• Efficiency: the ability to lower the cost of care without diminishing attainable improvements in health.
• Optimality: the balancing of improvements in health against the costs of such improvements.
• Acceptability: conformity to wishes, desires, and expectations of patients and their families.
• Legitimacy: Conformity to social preferences as expressed in ethical principles, values, norms, mores, laws, and regulations.
• Equity: Conformity to a principle that determines what is just and fair in the distribution of healthcare and its benefits among the members of the population.
One can clearly see the benefit of applying quality assurance components in the development of a BSC strategy. A BSC framework that meets quality assurance in healthcare is most probable that will meet patient needs, practitioners’ feelings, patient-practitioner relationship, amenities of care (e.g., confidentiality, privacy, comfort, cleanliness, convenience), as well as financial and organizational aspects required.
The most popular quality assurance model in healthcare is based, to the best of our knowledge, upon the Donadebian approach (Donabedian, 1980, 1982, 1985, 1993, 2003) where a healthcare organization (i.e., a hospital) is a system formed by the interaction of structures, processes, and outcomes. Structures are used to establish processes in order to create healthcare outcomes that have an effect on structures that need to change or adjust processes to meet the required outcomes. Strongly believing that healthcare outcomes are more important than financial outcomes in a healthcare system, we are confronted with a model where intangible assets are more important than tangible assets. This last statement makes a healthcare system very difficult to manage and a straightforward strategy hard to define.
The Need for a Specific Implementation plan
In order to implement a viable performance management strategy (i.e., a BSC framework) the steps one needs to take include:
• Determining what to monitor
• Determining priorities in monitoring
• Selecting an approach to assessing performance
• Formulating criteria and standards (i.e., Key Performance Indicators)
• Obtaining the necessary information
• Determining how and when to monitor
• Constructing a monitoring system
• Managing changes and improvements
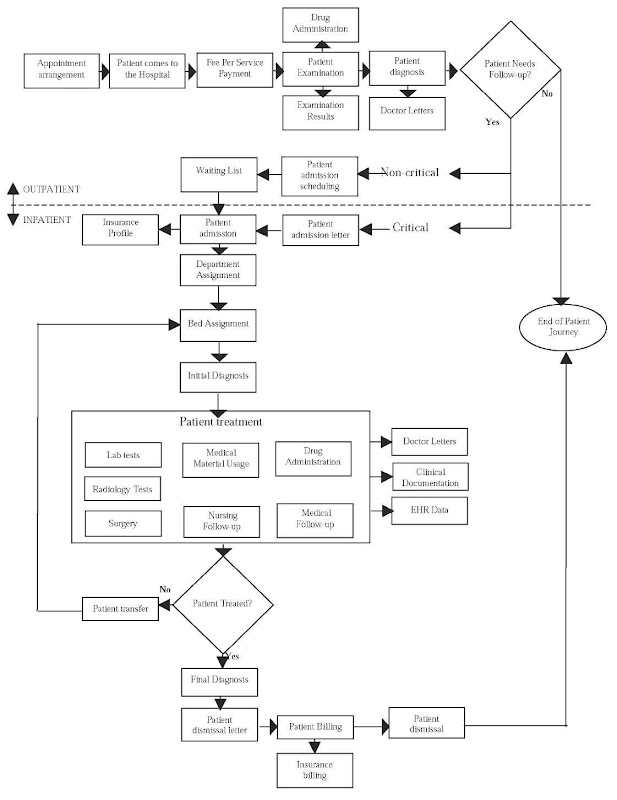
Building a patient-centered Healthcare Model
Finally, the proposed KPIs are directly or indirectly driven from healthcare processes. As an example, we propose to analyze a standard patient journey of a citizen in a healthcare institution. Figure 2 shows how the patient journey for a hospital is conceived (the patient journey in a primary care setting may be simpler). This workflow is the heart of the healthcare system and a prerequisite for any patient-centered information system to properly manage the information flow. This workflow is nowadays extended to include new processes such as emergency pre-hospital care and home care monitoring in order to create the hospital without walls of the 21st century.
Figure 2. The patient journey centered model for a hospital institution
Based on Figure 2 one can create a table where quality assurance and balanced scorecard features are confronted, analyzed, assessed and finally set. Table 1 is an example (non exhaustive) of the initial process.
From the above, it becomes apparent that the design and proposal of KPIs is not an easy task. KPI selection can vary upon specific measurement needs, upon goal set, and so on. In order to manage and validate the proposed KPIs by each BSC strategy, a set of KPI dashboards for each management entity, department or any other region of interest should be created.
use case: regional healthcare authorities in greece
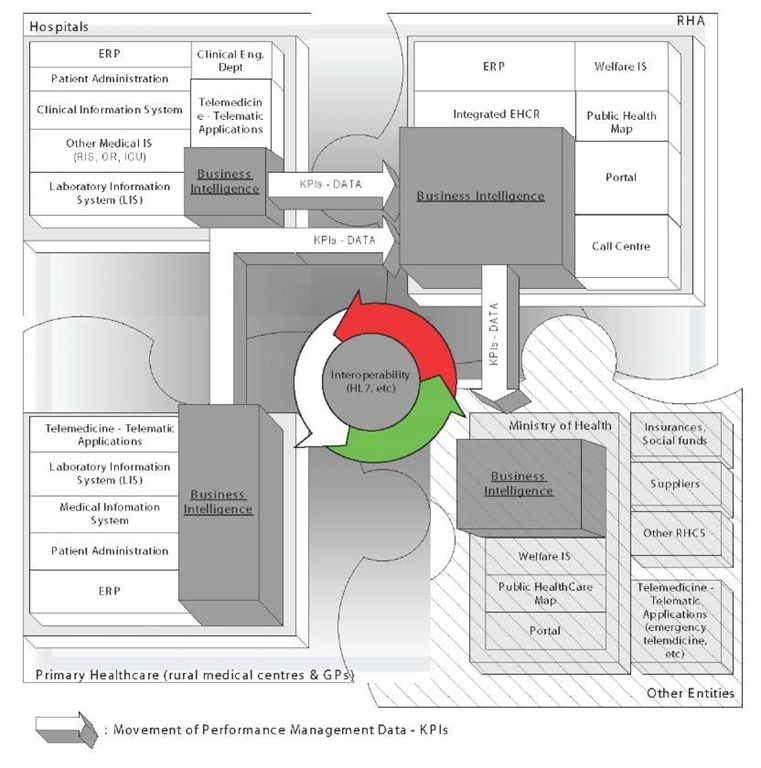
In 2001, a reform of the Greek National Healthcare System was introduced in order to enhance the performance and control of healthcare provision in Greece (Greek National Healthcare System Reform Act, 2001; Vagelatos & Sarivougioukas, 2003). One of the main changes was the division of the country in 17 autonomous healthcare regions where the Regional Healthcare Authority (RHA) is responsible for the regional healthcare strategy. This reform introduced the need to establish a three-level decision-making and performance management mechanism as described in Figure 3.
The proposed methodology was used to reach an initial set of KPIs by assessing existing knowledge and future needs (Decision No 1400/97/EC, 1997; McKee & Healy, 2002; Polyzos, 1999). Those KPIs were processed especially to serve the new strategy introduced in Greece.
As described in Figure 3, the regional healthcare system is comprised of a series of information systems covering the whole structures existing at any level, the processes required to meet the administrative and medical needs and finally, the outcomes that must come out from the implementation of such a complex interpolation of informatics infrastructure. The above information model was introduced to establish a community of networked healthcare organizations (hospitals, primary care) that are interoperating in order to support and implement the new healthcare strategy: to provide integrated and high quality healthcare services to the citizens based upon equal access to the resources (Information Society SA, 2003). In order to achieve this goal, two main issues were raised:
• How and when will information systems interoperate?
• What is the minimum required dataset to achieve the proposed strategy?
The first issue can be answered by using standards and protocols such as HL7 to meet with interoperability issues in healthcare (Spyrou, Berler & Bamidis, 2003). The second issue is partially addressed by the proposed initial set of KPIs presented below. The proposed KPIs are forming a complete set of metrics that enable the performance management of a regional healthcare system. In addition, the performance framework established is technically applied by the use of state-of-the art knowledge management tools such as data warehouses and business intelligence information systems.
The proposed KPIs are categorised into the four perspective stated by Norton & Kaplan, having also taken into account the raised quality assurance issues stated earlier. The performance indicators in a regional healthcare setting are depicted in Table 2.
Table 1. Defining KPIs from processes, an example
|
Workflow process |
BSC Perspective |
KPI |
QA approach |
Source of information |
|
Appointment arrangement |
Patient |
Appointments/day |
Process |
Hospital Information System (HIS), Scheduling S/W |
|
Patient comes to the Hospital |
Process |
Number of outpatients |
Process |
Hospital Information System |
|
Fee Per Service Payment |
Financial |
Mean cost per examination |
Process |
Billing, ERP S/W |
|
Drug Administration |
Process |
Number of prescription/ drug |
Outcome |
Patient Order Entry S/W, HIS |
|
Patient Examination |
Patient |
Patient satisfaction |
Process |
HIS, surveys |
|
Examination Results |
Growth |
Number of patient with re-examination |
Outcome |
HIS, Electronic Healthcare Record (EHR) |
|
Doctor Letters |
Process |
Number examinations/practitioner |
Outcome |
HIS, Electronic Healthcare Record (EHR) |
|
Patient diagnosis |
Growth |
Visits/ICD codes |
Outcome |
HIS, Electronic Healthcare Record (EHR) |
|
Patient Needs Follow-up? |
Process |
Number of inpatient from outpatient clinic |
Process |
HIS |
|
Waiting List |
Patient |
Waiting time in days |
Structure |
Hospital Information System (HIS), Scheduling S/W |
|
Patient admission scheduling |
Patient |
Equity of delivered care |
Process |
Hospital Information System (HIS), Scheduling S/W |
|
Patient admission letter |
Process |
Number of emergency cases/day |
Process |
HIS |
|
Patient admission |
Process |
Number of inpatients |
Process |
HIS |
|
Insurance Profile |
Financial |
Net cash flow per insurance company |
Process |
HIS, ERP |
|
Department Assignment |
Financial |
Mean operational cost per department |
Structure |
HIS |
|
Bed Assignment |
Process |
Bed coverage rate |
Structure |
HIS |
|
Initial Diagnosis |
Process |
Admission per case type (ICD 10) |
Outcome |
HIS, Electronic Healthcare Record (EHR) |
|
Lab tests |
Process |
Mean value of lab test per doctor, per patient |
Outcome |
Laboratory Information System (LIS) |
|
Radiology Tests |
Process |
Mean value of radiology test per doctor, per patient |
Outcome |
Radiology Information System (RIS) |
|
Surgery |
Financial |
Mean cost of surgical procedure |
Structure |
HIS, Electronic Healthcare Record (EHR) |
|
Medical Material Usage |
Financial |
Mean cost of medical material consumption |
Outcome |
HIS, ERP |
|
Nursing Follow-up |
Growth |
Number of Nurses per bed |
Process |
HIS, Electronic Healthcare Record (EHR) |
|
Medical Follow-up |
Growth |
Number of practitioners per bed |
Process |
HIS, Electronic Healthcare Record (EHR) |
|
Clinical Documentation |
Process |
Number of medical procedures per day |
Outcome |
HIS, Electronic Healthcare Record (EHR) |
|
EHR Data |
Patient |
Number of cases with EHR |
Outcome |
HIS, Electronic Healthcare Record (EHR) |
|
Patient transfer |
Process |
Number of patient transfers/ patient or /day |
Process |
HIS |
|
Patient Treated? |
Growth |
Number of patients treated under a specific critical pathway |
Process |
HIS, Electronic Healthcare Record (EHR) |
|
Final Diagnosis |
Growth |
Cases per final diagnosis |
Outcome |
HIS, Electronic Healthcare Record (EHR) |
|
Patient dismissal letter |
Patient |
Inpatient Satisfaction |
Process |
HIS, surveys |
|
Patient Billing |
Financial |
Mean treatment cost per day |
Process |
Billing, ERP S/W |
|
Patient dismissal |
Process |
Mean length of stay /per dept. per ICD code |
Process |
HIS |
|
Insurance billing |
Financial |
Return of Capital Employed (ROCE) |
Process |
Billing, ERP S/W |
Each of the above KPIs is the result of analysis based upon the needs of a standard regional healthcare authority. The proposition of a set of KPIs is nevertheless not the complete solution of the problem. Implementing KPIs is a constant process based upon specific metrics that each regional healthcare authority and each department or institution under its control must periodically assess and reengineer. Assessment should be based upon specific goals met and reengineering is often required due to administrative, demographic or other important changes that must occur. Focusing for example in the KPI marked as “mean treatment cost per day” one should notice that the KPI does not mean much without a metric. In Greece, most ofinpatient treatments are based upon fixed prices per day and do not follow the pay per service model which is financially more viable.
Figure 3. Regional healthcare information systems framework and interoperability
Healthcare financials are part of a national policy aiming at providing high quality healthcare services to all citizens regardless of their income, social status or other characteristic. As a consequence, the use of the fixed price model (per day quotas) in Greece serves that purpose albeit with its advantages and disadvantages. Current treatment cost per day (for an inpatient) has been fixed to about 135 Euros and this value could be used as an initial metric. If this value is exceeded this would mean that the RHA budget will cover the difference or transfer the cost to insurance companies and social welfare. In addition, a regional healthcare authority will then have credible proof that national standards are outdated and require revision in order to support the system. As a result, this KPI has now a specific meaning linked to regional strategy and budgetary needs. Following that example, all financial KPIs are therefore an important perspective of BSC since they are the measurement of the financial viability of the regional healthcare authority. In fact, all KPIs should be associated with adequate metrics in order to be assessed, thus driving the RHA towards the right strategic decisions.
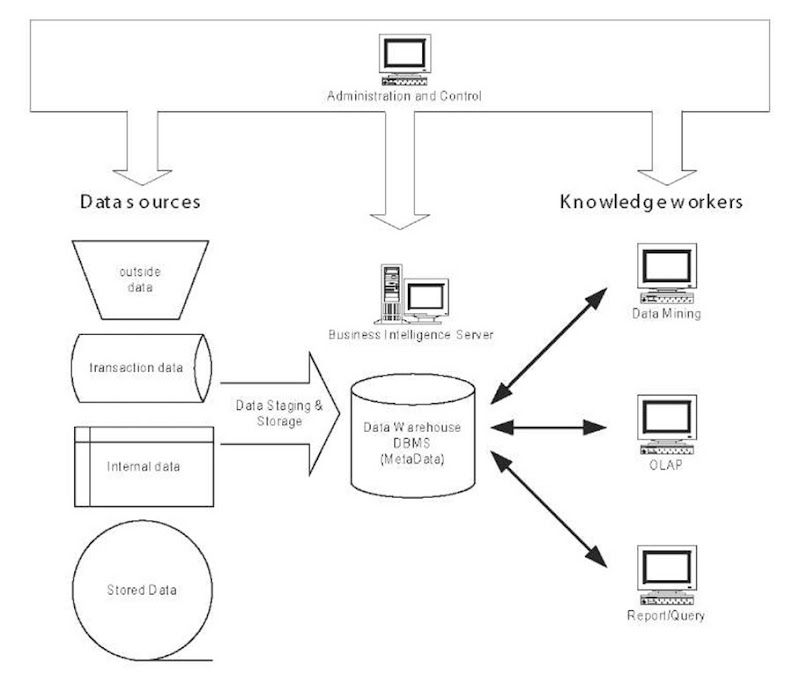
In order to meet and populate the above-mentioned KPIs a regional healthcare authority has to implement a complex information technology system in order to gather up all needed information. Then the information collected through the use of enterprise resource planning software, hospital information systems, clinical information systems, radiology information system, and laboratory information systems has to be processed and interpolated to produce the final metadata set from which the KPIs are driven. In other words, the model is complemented by a business intelligence solution similar to the one depicted in Figure 4.
Table 2. KPIs in a regional healthcare setting
|
No Financial KPI description F1 Mean treatment cost per day F2 Mean cost of medical treatment per patient F3 Mean cost of drugs consumption F4 Mean cost of radiology testing F5 Mean cost of laboratory testing F6 Mean cost of material consumption F7 Mean cost of surgical procedure F8 Mean operational cost per dept./clinic F9 Mean cost of vaccination procedures F10 Mean cost per medical examination F11 Return of capital employed (ROCE) F12 Net Cash flow F13 Income per employee F14 Payroll rate versus operational costs. |
No Process KPI description P1 Length of stay P2 Patient admission rate per medical unit P3 Percentage of bed coverage P4 Vaccination rate P5 Mean value of performed test per patient, per doctor P6 Number of inpatients P7 Number of outpatients P8 Number of drug prescription P9 Number of laboratory tests P10 Number of surgery procedures P11 Number of radiology tests P12 Number of visit in outpatient clinics P13 Number of visits in primary care institutions P14 Number of dental care processes P15 Number of processed emergency cases P16 Number of unprocessed order entries on the same day P17 Number of preventive care visits P18 Number of home care monitored patients P19 Assessment of patient satisfaction |
|
No Customer (patient) KPI description C1 Mortality rate C2 Morbidity rate C3 Number of medical staff per 1000 inhabitants C4 Number of beds per 1000 inhabitants C5 Accessibility of patients to the medical units C6 Time in a waiting list C7 Equity of delivered care C8 Number of readmission per patient C9 Mean length of stay C10 Patient Satisfaction rate |
No Learning and Growth KPI description L1 Medical device usage growth L2 Healthcare professionals training rate L3 Employee Satisfaction rate L4 Number of doctors per bed L5 Number of nurses per bed Lg Number of existing healthcare professionals versus expected job positions L7 Personnel productivity rate L8 Number of medical interventions per doctor L9 Number of patient with re-examinations L10 Visits/ICD codes L11 Admissions per case type (ICD 10) L12 Dismissals per case type (ICD 10) |
Figure 4 shows how data are collected from the various data sources, cleansed and homogenised, and finally redistributed to the knowledge workers and decision makers of the regional healthcare authority (Extraction, Transformation and Load—ETL).
The data collection process is extremely important since it is a basic feature of successfully populating the KPIs. In that sense both organizational and technological issues to achieve data quality should be considered. In the proposed setting, the regional healthcare authority has imposed on its healthcare units the use of specific classifications, codifications and taxonomies such as the 10th edition ofthe International Classification of diseases (ICD10). In addition, the proposed KPIs can be seen as attributes of structure, process or outcome (based upon the Donabedian approach) so that they can be used to draw an inference about quality. As such the KPIs are proposed, designed, tested and assessed by a panel of experts (executive officers of the RHA, practitioners). By implementing this organizational structure the quality level of the proposed KPIs is such that technological issues are greatly reduced.
Figure 4. Regional healthcare authority business intelligence framework
future trends
Up to this point, this topic has mostly dealt with organizational and strategic features of knowledge management in healthcare. In the proposed use case we have shown an ongoing implementation of a Balanced Scorecard Framework in a regional healthcare authority environment. This has been done intentionally wishing to state that the technological part on such an implementation is probably the less important issue. If one regards the future trends in knowledge management, one can see that a multitude of new tools are already proposed for use. This topic will briefly set the focus on the trends that to our knowledge are the most promising and present more opportunities to healthcare organizations in creating effective performance management facilities.
Service Oriented Architecture and Patient-Centered Architecture (Based on the Electronic Health Record)
The term of patient-centered architecture has been already in the literature for some years.
Many techniques have been used in the past such as Corbamed (Object Management Group, 2001) and Distributed Healthcare environment (DHE). The introduction of web technologies such as the Extensible Markup Language (XML), the Simple Object Access Protocol (SOAP), the Web Services Description Language (WDSL), and more precisely the concept of Web Services (Deitel, Deitel, DuWaldt, & Trees, 2003; W3C, 2003) are driving information technologies towards a Service Oriented Architecture (SOA).
A service is a software component that is suitable for cross-application access. A service is never a complete application or transaction. It is always a building block. SOA is the architecture of an application that uses services. Services define reusable business functions; SOA binds services into applications. Logically, services are defined by their interfaces. Technically, services are defined by their implementations (sometimes complex integrated flows, other times a single simple program). SOA is a logical concept, and its design is focused on the definition of service interfaces and interactions between service interfaces. Fundamental to SOA is the loose coupling between its components. At the logical level, this translates to the ability to add a new service for the end-user unobtrusively to the service provider. At the technical level, this translates to the ability of software developers to deploy a new application that calls a service without the need to redeploy or change the service. The use of SOA will allow the creation of process-based components of applications that will manipulate knowledge and information based upon the processes and the required or designed outcomes.
The Semantic Web
The Semantic Web goes beyond the World Wide Web by encoding knowledge using a structured, logically connected representation, and by providing sets of inference rules that can be used to conduct automated reasoning. Whilst the idea of knowledge representation languages is not new, existing languages generally use their own set of ontologies and inference rules to identify and eliminate logical contradictions and inconsistencies. The Resource Description Frame-work—RDF (W3C, 2003) and XML Topic Maps (TopicMaps.Org, 2001) are the most promising tools towards the implementation of the Semantic Web in practice. Nevertheless, a long way towards maturity has still to be covered since issues such as specific metadata frameworks and data quality are not yet solved. In any case, the Semantic Web should enhance the promotion of clinical practice guidelines and evidence based medicine. They can be seen as taxonomies of medical cases that could be both used for performance monitoring (in respect to commonly agreed levels of delivered care) and decision support for the healthcare practitioners.
Critical Pathways
Critical Pathways (Wall & Proyect, 1998) are mechanisms for transforming a reactive bureaucratic ritual to a dynamic, indispensable, clinical improvement process. A critical pathway when established is a mechanism for:
• Integrating continuous quality improvements with traditional patients’ care review
• Managing and impacting of clinical and financial outcomes for a specific treatment procedure
• Proactively addressing economic and regulatory changes
• Improving clinical outcomes through reduction in variation
• Controlling unnecessary cost and resource usage without jeopardising quality of care
• Fostering multi-disciplinary approach to patient care
• Linking quality management to staff education
• Managing limited financial resources
• Making efficient use of scarce organizational resources
• Increasing readiness for anticipated changed in healthcare
• Applying and using clinical practice guidelines and other taxonomies set up by different professional societies
Critical Pathways can be seen as “specialized” performance management tools that would provide a BSC framework with very specific performance indicators for each treatment or clinical process.
conclusions
Performance management is a key issue in the continuous process of delivering high quality healthcare services. The use of KPIs has proved that the design of a Balance Scorecard acts as the “cockpit” of a regional (or national) healthcare authority where all metrics are the flight instruments enabling the provision of healthcare based upon equity, financial control, continuous process and structure refinement, and outcome measurements. In that sense, the proposed infrastructure is, technologically speaking, an important knowledge management tool that enables knowledge sharing amongst various healthcare stakeholders and between different healthcare groups. The use of BSC is an enabling framework towards a knowledge management strategy in healthcare since KM is about discovering knowledge from existing information, about creating new knowledge and about implementing processes and taxonomies that enable the reuse and assessment of information as part and bits of knowledge.
Knowledge can be seen as a performance management tool both for administrative purposes and clinical improvements.
During the implementation process of deploying a technological platform for performance management or any other type of knowledge management infrastructure, one must have in mind that:
• The six issues described in the introduction section must being taken into strong consideration from day one.
• It is important to focus on people, processes and outcomes, and to set-up a straightforward strategy to plan, manage, assess, educate, disseminate, and maintain the developed BSC framework.
• Any type of knowledge management project bases its success on continuous improvement and assessment. Metrics and processes are meant to change in order to reflect improvements towards quality of healthcare.
• The knowledge and technology is there, but still very limited best practices have been successfully implemented.
• The implementation of BSC framework is a time consuming process that has to involve all stakeholders’ representatives.