abstract
Superior access, quality, and value of healthcare services has become a national priority for healthcare to combat the exponentially increasing costs of healthcare expenditure. E-Health in its many forms and possibilities appears to offer a panacea for facilitating the necessary transformation for healthcare. While a plethora of e-health initiatives keep mushrooming both nationally and globally, there exists to date no unified system to evaluate these respective initiatives and assess their relative strengths and deficiencies in realizing superior access, quality and value of healthcare services. Our research serves to address this void. This is done by focusing on the following three key components: 1) understanding the Web of players (regulators, payers, providers, healthcare organizations, suppliers, and last but not least patients) and how e-health can modify the interactions between these players as well as create added value healthcare services, 2) understand the competitive forces facing e-health organizations and the role of the Internet in modifying these forces, and 3) from analyzing the Web of players combined with the competitive forces for e-health organizations we develop a framework that serves to identify the key forces facing an e-health and suggestions of how such an organization can structure itself to be e-health prepared.
introduction
E-health is a broad term that encompasses many different activities related to the use of the Internet for the delivery of healthcare service. Healthcare professionals are extending the use of the Internet to include a source of evidence-based consumer information as well as to facilitate the research of protocols for healthcare delivery, accessing laboratory and medical records, and performing second opinion consults (Sharma & Wickrama-singhe, 2005; Sharma, Wickramasingeh, Xu, & Ahmed, 2006). Moreover, the Internet is being used by patients to become more knowledgeable about health practices as seen from their questions to their physicians (Gargeya & Sorrell, 2005).
Although, a relatively new term and unheard of prior to 1999, e-health has now become the latest “e-buzzword” used to characterize not only “Internet medicine,” but also virtually everything related to computers and medicine (Sharma et al., 2006; Von Lubitz & Wickramasinghe, 2006). The scope and boundary of e-health, as well as e-heath organizations, is still evolving. However one can only imagine it will grow rapidly especially given that governments in both U.S. and Europe, and organizations such as WHO (World Healthcare Organization) are advocating that e-health be on the top of all healthcare agendas and an integral component of any healthcare delivery initiative (Von Lubitz et al., 2006).
Given the growth and variety of e-health initiatives, it becomes important to examine the forces affecting these initiatives and factors leading to the success of e-health. To date, little research examines metrics of measurement pertaining to e-health initiatives or their economic value. What are the forces of competition affecting e-heath? Are the competitive forces constrained by external considerations? Is the issue of competition an appropriate concern for e-health? If so, what are the strong and weak competitive forces? We argue that analysis of these forces would lead us to understand the long-term sustainability of any e-health initiative.
traditional competitive forces
The starting point for understanding the competitive forces facing any e-health initiative lies in understanding the fundamentals of traditional competitive forces that impact all industries and then how the Internet as a disruptive technology has impacted these forces.
The strategy of an organization has two major components (Hendersen & Venkatraman, 1993). These are 1) formulation–making decisions regarding the mission, goals, and objectives of the organization and 2) implementation–mak-ing decisions regarding how the organization can structure itself to realize its goal and car-ryout specific activites. For today’s healthcare organizations the goals, mission, and objectives all focus around access, quality, and value and realizing this value proposition for healthcare then becomes the key (Wickramasinghe, Fadlalla, Geisler, & Schaffer, 2005). Essentially, the goal of strategic management is to find a “fit” between the organization and its environment that maximizes its performance (Hofer, 1975). This then describes the market-based view of the firm and has been predominantly developed and pushed by the frameworks of Michael Porter. The first of Porter’s famous frameworks is the generic strategies (Porter, 1980).
The use of technology must always enable or enhance the businesses objectives and strategies of the organization. This is particularly true for 21st Century organizations where many of their key operations and functions are so heavily reliant on technology and the demand for information and knowledge is so critical. A firms’ relative competitive position (i.e., its ability to perform above or below the industry average is determined by its competitive advantage). Porter (1980) identified three generic strategies that impact a firm’s competitive advantage. These include cost, focus, and differentiation. Furthermore, Porter himself notes that two and only two basic forms of competitive advantage typically exist:
1. Cost leadership.
2. Differentiation.
Firms can use these two forms of competitive advantage to either compete across a broad scope of an industry or to focus on competing in specific niches; thereby, leading to three generic strategies. Porter (ibid) notes that firms should be cautious about pursuing more than one generic strategy; namely cost, differentiation, and focus. For example, if a cost leadership strategy is adopted it is unlikely that a firm can also maintain and sustain differentiation since it would not be possible to simultaneously pursue the costly capital investment or maintain high operating costs required for differentiation and thus in the long run the firm has a confused strategy which leads to failure.
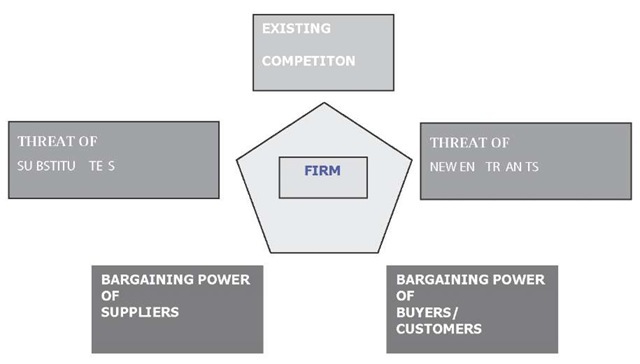
In order to design and develop ones strategy, an organization should first perform an industry analysis. Porters Five Forces or Competitive Forces model is most useful (Porter, 1980, 1985). Figure 1 depicts this model. Essentially, Porter has taken concepts from micro-economics and modeled them in terms of five key forces that together outline the rules of competition and attractiveness of the industry.
The forces are as follows:
1. Threat of new entrant: A company new to the industry that could take away market share from the incumbent firms.
2. Threat of substitute: An alternative means that could take market share from product/service offered by the firms in the industry.
3. Bargaining power of buyers: The strength of buyers or groups of buyers within the industry relative to the firms.
4. Bargaining power of suppliers: The strength of suppliers relative to the firms in the industry.
5. Rivalry of existing competition: Relative position and market share of major competitors.
The collective strength of these five forces determines the attractiveness of the industry and thus the potential for superior financial performance by influencing prices, costs, and the level of capital investment required (Porter, 1985). Once a thorough industry analysis has occurred, it is generally easier for a firm to determine which generic strategy makes most sense for it to pursue and enables the firm to exploit most of its core competencies in its existing environment.
Figure 1. Porter’s Competitive (Five) Forces Model
Role of the Internet of the competitive Forces
Feeny (2001) presents a framework that highlights the strategic opportunities afforded to organizations by using the Internet. In particular, he highlights three e-opportunity domains. Table 1 details these domain and their respective components.
E-opportunities in Healthcare
Given the three areas of e-opportunities previously discussed, Glaser (2002) identifies several key e-opportunities for healthcare. Table 2 details these.
Web of players in healthcare
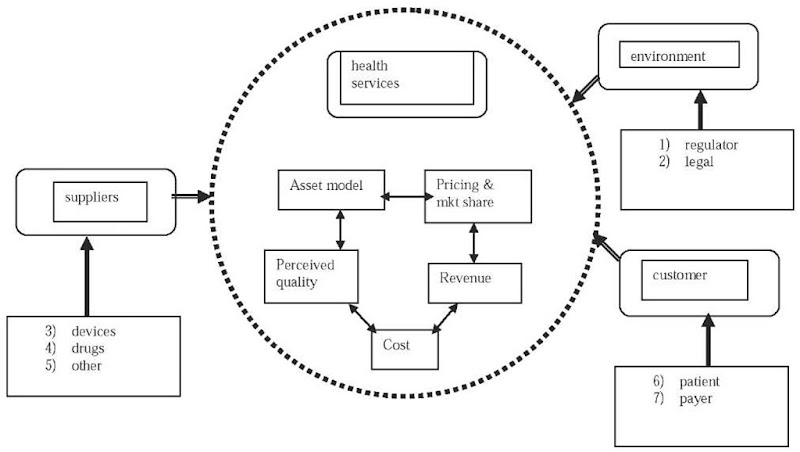
Figure 2 depicts the Web of healthcare players and the key elements of the any e-health architecture that serves to support the interactions between and within this Web of players. In order to fully capture the flows of information it is necessary to first identify the primary producers and consumers of data and information within the healthcare system. At the center of the information flows is the HCIS (healthcare information system, i.e., the e-health network) because not only does it connect the key players within the healthcare system in an efficient and effective manner, but also it forms the central repository for key information such as patient medical records, billing, and treatment details. Hence, the HCIS provides the foundation for supporting the information flows and decision making throughout the healthcare system. Figure 2 then represents a macro view of the inter-relationships between the key players within this system as well as the sources, destinations and flows of information between these players and the pivotal role of the HCIS.
Healthcare procedures such as medical diagnostics, treatment decisions, and consequent effecting of these decisions, prevention, communication, and equipment usage can be thought of as iatric in nature (Wickramasinghe & Fad-lalla, 2004). Integral to these iatric procedures is the generating and processing of information (Wickramasinghe & Fadlalla, 2004). The patient naturally provides key information at the time of a clinical visit or other interaction with his/her provider. Such a visit also generates other information including insurance information, medical history, and treatment protocols (if applicable) which must satisfy regulatory requirements, payer directives and, obviously, the healthcare organization’s informational needs. Thus, we see that from a single intervention many forms and types of information are captured, generated, and then disseminated throughout the healthcare system. All this information and its flows must satisfy some common integrity characteristics such as accuracy, consistency, reliability, completeness, usefulness, usability, and manipulability. Consequently, generating a level oftrust and confidence in the information’s content and processes. Since the information flows across various organizational boundaries, the challenge of ensuring information integrity is further compounded because any integrity problems will propagate with ripple effects following the same trajectory as the information itself. Given the high degree of inter-relatedness between the various players, the consequences of poor quality information (such as the cost of information integrity problems) are multiplied and far reaching. This highlights the need for robust, well designed, and well managed HCIS (Wickramasinghe & Fadlalla, 2004). Such a perspective should not be limited to new systems, but rather, equally and perhaps of even more importance should be applied to existing systems as well.
Table 1. The three e-opportunity domains and their components
|
|
Components |
|
e-operations |
• Automation of administrative processes • Supply-chain reconfiguration • Reengineering of primary infrastructure • Intensive competitive procurement • Increased parenting value |
|
e-marketing |
• Enhanced selling process • Enhance customer usage experience • Enhanced customer buying experience |
|
e-services |
• Understanding of customer needs • Provision of customer service • Knowledge of all relevant providers • Negotiation of customer requirements • Construction of customeroption^^ |
Table 2. The e-opportunities for healthcare organizations
|
|
Components |
|
e-operations |
• Internet-based supply purchasing • Prescription writing, formulary checking, and interaction checking using hand-held devices |
|
e-marketing |
• Delivery of consumer health content and wellness management tools over the Internet • Use of consumer health profiles to suggest disease management and wellness programs |
|
e-services |
• Patient-provider communication and transaction applications • Web-based applications to support the clinical conversation between referring and consulting physicians |
|
Crossing multiple domains |
• Increasing the level of information content in the product • Increasing the information intensity along the supply chain • Increase in the dispersion of information |
MODELING THE COMPETITIVE FORCES IN E-HEALTH
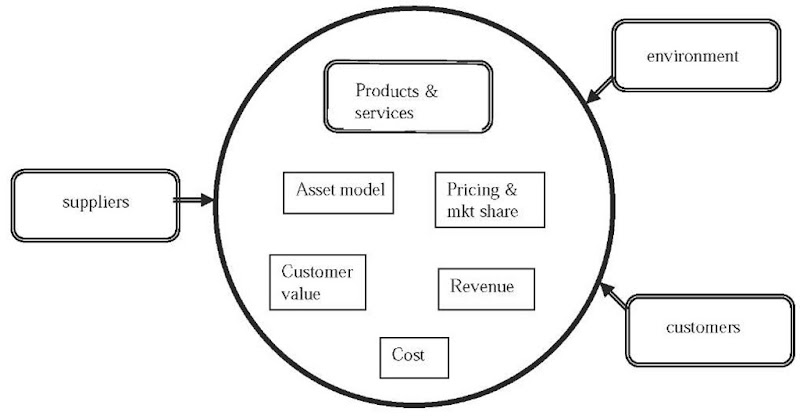
In order to model e-health, let us first construct a general model of the competitive forces pertaining to e-business. E-business is not simply offering traditional products and services on line. It requires broad-scale asset redeployment and process changes, which ultimately serve as the basis for a company’s competitive advantage in today’s Digital Economy. For this study, the e-business model could be broken into components such as; products and services, customer value, pricing component, revenue source, the cost component, and asset model as shown in Figure 3.
Figure 2. Web of e-health players adapted from Wickramasinghe et al 2004
The prime objective of business model is to make money (La Monica, 2000). The various components of business model as shown in Figure 1 work together to create profit margins for the business. First of all, the electronic business model should offer products and services online. These products and services should be differentiated with competitors by low price or unique customer value. The products are differentiated if customers perceive some value in these that other products do not have. Differentiation can be done by offering different product features, timing, location, service, product mix, linkage between functions, etc. (Afuah & Tucci, 2000). Customer value can be judged whether firm offering its customers something distinctive or at a lower cost than its competitors. The success of business model depends upon how does the firm price the value? An important part of profiting from the value that firms offer customers is to price it properly. For pricing, market shares and margins would be most critical. The good business model should strive for high market share and thus firm should devise strategies accordingly. Pricing of products depends upon the cost and asset model of the firm. The cost (fixed cost + variable cost) should be spread in a fashion that profit margins remain high. The profits in electronic business model case will not only come from sales but may come from many other sources. Therefore, revenue source is another important component for business model. The sustainability of business model can be gauged based upon non-imitable nature of products and services. How can firm continue improve market share and make more money and have competitive advantage are the kind of questions needs to answers for the sus-tainability of business model. For example; using simple profits equation; Profits=(P-Vc)Q-Fc , firm can assess how each of the components of business model impact profitability. If a firm offers distinctive products, it can charge premium price P for it. A good business model should keep low variable cost but should have high market share for higher profitability (Afuah et al., 2000). Taking these components of a business model into consideration, let us now map this to the healthcare domain (Figure 4).
In so doing, some of the nuances pertaining to the dynamics of healthcare become apparent; such as, the receiver of services, or the patient, is not usually the principal payer. Moreover, the model serves to underscore that for e-health initiatives to truly add value and be sustainable the dynamics of a generic e-business model must be satisfied. Hence, some determination needs to be made regarding Vc, Fc, P, and Q in this context.
Figure 3. Generic e-business model components
Figure 4. e-health business model components
To understand these dynamics more easily let us consider a case study example of the implementation of an electronic patient record.
case study
The Johns Hopkins Medicine Center for Information Services Public LAN (JPL) is a computer network designed to provide patient care providers access to clinical applications. This computer network is utilized by all types of patient care providers in both inpatient and out patient services. These providers include, but not limited to, doctors, interns, fellows, nurses, unit clerks, pharmacists, nutritionists, and admission specialists. In this article, an examination of the history of the Public LAN, the current state of the LAN, and the future of the Public LAN will be examined. Since its inception the Public LAN as been the leader in efficiency and innovation for Desktop Computing Services (DCS), a division of Information Technology @ Johns Hopkins (IT@Hopkins).
Introduction of the public LAN
During the spring of 1996, JHMCIS and a group of doctors developed an in-house application to provide patient care. This application is called Electronic Patient Record or EPR. The application was to be used in patient areas for tracking patient record. These records can then be viewed by other clinicians throughout the hospital. A second application was introduced at the same time to provide a graphical user interface to many of the hospital’s mainframe and mid-range systems. This application is Host Interface Program or HIP. The challenge at this stage was to provide a computer system that could be used by the doctors that would allow EPR and HIP to be used to provide patient care and at the same time have a desktop system that was secure.
These desktops were to be deployed in medical exam rooms and the major problem was having a desktop that could provide these applications to the clinicians without allowing the clinicians or patients the ability to access the operating system and the computer configuration. This led to the development of the Public Desktop.
The Public desktop is a Microsoft Windows based desktop that has the clinical applications installed, as well as an Internet browser and the Microsoft Office suite. The challenge was managing these systems in areas with limited access during business hours as they were in use by clinicians providing patient care. The operating system was secured and limited access was given to the users. The users were not able to install any applications or download any programs.
The Public LAN started out with 70 desktops in three clinical areas. The Harriet Lane Clinic, which is an outpatient clinic for pediatrics, the neonatal intensive care unit, and the adolescent outpatient clinic. This pilot lasted approximately six months. During the next three years, the Public LAN grew to 1100 desktops.
The Growth of the public LAN
Today the Public LAN supports over 1800 desktops and many clinical applications. During the first three years of the Public LAN, the number of systems reached over 1100 systems. Included in this growth, not only the number of devices supported, but the number of applications that were supported on these desktops. The driving forces of these changes were outdated clinical applications that were being replaced with client server applications and the millennium with applications that were not year 2000 compliant.
During this time, the application supported grew to include BDM, a new pharmacy application, Vision—a nutrition application and ClicTate, a pediatrics version of EPR. With the intention of more clinical applications moving from the mainframe and mid-range systems to client server applications, the desktops are going to need to be able to handle these additional applications.
The process of managing these systems became a challenge as well. Since the desktops were standardized, DCS was able to implement Microsoft’s System Management Server (SMS). This allowed not only the ability to manage these desktops, but also distribute software, inventory the hardware, and software of a specific system, and provide remote control capabilities. SMS was included when the pilot of the Public LAN was deployed but its true value was not realized until the rapid growth of the LAN.
The public LAN Today
The Public LAN today is well over 1800 desktops, supporting more than 30 clinical applications. Most of these applications are still accessed via HIP, however more client server applications are also supported. The additional client server applications have lead to different configurations of the desktop’s application software or “flavors” of Public workstations. Currently there are currently many different configurations for the Public Workstations. These different configurations include:
• Standard configuration.
• Training configuration.
• Wilmer Eye Clinic configuration.
• Pharmacy configuration.
• Nutrition configuration.
• Provider Order Entry configuration.
• Operating room configuration.
• DCOM image viewing configuration.
• Eclypsis Point of Care configuration.
• Procedure Reporting System configuration.
• OB/GYN Configuration.
These different configurations can be on a few as 20 desktops to as many as 600, where the standard configuration is on all of the desktops. The standard configuration is:
• Windows XP Professional.
• EPR.
• HIP.
• Internet Explorer.
• Microsoft Office Suite.
• Adobe Reader.
• Calculator.
The additional configurations are based on adding additional clinical applications to the desktops. In addition, many of the systems have multiple clinical applications installed.
The Lessons Learned
During the growth of the Public LAN, many lessons have been learned. These lessons include best practices for desktops management, application management and deployment, and reduction in the total cost of ownership of a desktop.
The current network is supported by three desktop technicians, which is an average of 600 plus desktops per technician. Desktop Computing Services needed to have a way to manage these systems not only located at the East Baltimore campus, but at other campuses within the Baltimore metropolitan area. The use of Microsoft Systems Management Software (SMS) was deployed to allow desktop management. SMS allows a technician the ability to remote control in to a desktop and perform work as if they were at the desktop. This capability also allows the support staff to view the process of the user and see the error as it happened. SMS also is used to deploy application software to the desktop.
Due to the increased number of clinical applications, the number of different application software configurations increased. In order to manage this DCS used SMS for application deployment. DCS is able to determine the application software installed on the desktop and perform upgrades to the software. The upgrade to an application is preformed by using SMS to “push” and install the software on the desktop without any user intervention. Therefore, and application could be upgraded or installed without having to visit the desktop.
With the integration of SMS to manage the desktops, this has reduced the total cost of ownership of supporting the Public LAN. This decrease is realized by having a ratio of one desktop technician per 600 desktops. DCS is able to remote control the desktop; this prevents the technician from have in walk across campus to help a user. In addition, the installation of applications and upgrades to applications is completed on many systems at once without having to visit each individual desktop. Also, DCS has secured the desktop to prevent the users from accessing the operating system and the hard drive. If the users were able to access the operating system and download and install applications, including spyware, this would greatly increase the support costs of the desktop.
The Future of the public LAN
The future of the Public LAN at Johns Hopkins Hospital is ever evolving. The needs of the clinicians for resources to provide patient care are continually changing. With patients bringing medical records in on CD-ROM to access to network resources the Public LAN must evolve to meet these needs. In order to meet these needs the Public LAN support staff is required to find clever and innovative ways to provide these resources. New hardware is being added to the Public desktops to allow viewing of clinical data on CD-ROM, the use of USB keys for file storage has been enabled and logging in with a personal account.
The ability for a clinician to login with their personal account allows them to access network resources. These resources include access to network file servers and departmental file servers. In order for a clinician to use a personal account they are required to have a timeout of their session. The timeout of the session will log the user off after a certain amount of idle time. The reason for this is to prevent others from accessing information and to prevent non Johns Hopkins employees to access data and network resources.
The future of the Public LAN is ever evolving. The Johns Hopkins Hospital is building two new clinical towers that will be state of the art. The devices that provide patient care will also need to be state of the art and provide clinicians the ability to provide patient care in a completely paperless, film-less, and wireless network. The Public LAN will be able to provide these solutions and will realize the benefits of these efforts, as patients are cared for more efficiently and effectively.
Mapping the case to the Model
The implementation of the EPR at Johns’ Hopkins represents a relatively common e-health initiative in the current healthcare environment. The EPR enables the seamless flow of patient data and thus facilitates the delivery of efficient and effective quality healthcare to the patient. This is certainly professed as a key benefit for the embracing of EPR in most instances.
The e-health sustainability model however, suggests that one must analyze the micro- and meso-dynamics more closely to actually determine the sustainability of such an initiative. Specifically, it is necessary to capture key factors including, perceived quality, fixed and variable costs, price and market share and quantity and then look at the interaction of these factors before sustainability of the initiative can be pronounced. However, this is beyond the scope of this article but will form the focus of future research.
What can be noted at this point and will be research in more detail in future work is the size or scale of the e-health initiative. Returning to the simple profit equation Profits=(P-Vc)Q-Fc, in the case scenario above, fixed costs will be constant and Vc for any EPR will be marginal given the generic nature of the program and the applications of it by various providers hence we hypothesis that the sustainability of the EPR would increase with Q the quantity or size. Thus, the larger the EPR initiative the more likely it is to be sustainable. Quantitative data to support the relationship between scope and quantity and impact of ICTs in general in healthcare settings can be found in previous studies (Wickramasinghe & Lamb, 2002; Wickramasinghe & Silvers, 2003).
Discussion
In mapping the John’s Hopkins case to the model in Figure 4, we can see that the reality of an e-health initiative involves the interactions of various groups of stakeholders. Knowledge management provides an umbrella under which we may discuss a number of opportunities and raise issues relative to components of the business model. The vision of collaboration between components of the business model recognized as stakeholders is one of great opportunity. Stakeholders in this case include suppliers, the firm, the customer, and the government as a key representative of the environment. Each stakeholder brings to the table talent, resources, and differentiated perspectives that, together, create a robust whole in addressing problems and projects. For example, suppliers can be a source of knowledge that can assist the firm in delivering cost effective products and services. Customers are an additional source of knowledge in terms of personal history and preferences. The firm can manage knowledge in a form that maximizes the probability of value added products and services. The government can serve as a catalyst to create an environment conducive to knowledge exchange and management.
Unfortunately, great opportunities do not always turn into reality. Collaboration successes between suppliers, the firm, and its customers much less the government can, sadly, be few and far between. In addition to strengths and distinctions, each stakeholder also brings to the table residual weaknesses and biases that can scuttle the best of collaborative intentions. For example, internal firm bureaucracy can easily drive out the best of suppler intentions and customer good will. Problems can easily be left unaddressed and efforts can easily fail as reality drives out vision. This can be exacerbated by cultural norms and historical behaviors embedded in government policies.
A case in point is the handling of SARS. Levels of suffering and unnecessary deaths were, in part, a result of lack of collaboration between stakeholders. In this case, government agencies (specifically the hospital authorities) were negligent in sharing information and allocating resources amongst hospitals. The hospitals, however, were not guilt free and were accused of withholding information to customers including patients and their families. Further, the relationship between suppliers and hospitals was insufficient to respond to the need for supplies. Shortages were evident and supplies misapplied in circumstances that could have been adverted through collaboration. The situation was further strained as lack of information sharing across governments and excessive bureaucratic delay inhibited quick action to rapidly respond to changing circumstances. In summary, stakeholder collaboration could have, arguably, avoided hardship at individual and societal levels. Unfortunately, it didn’t happen and the World Health Organization (WHO) was, rightly, exasperated.
Experiences with SARS have sensitized stakeholders at all levels with respect to effectively dealing with potential pandemics e.g., H5N1-based bird flu. Over the past months, we have already seen a much higher level of information exchange and collaboration than existed in the lead-up to SARS. Governments have more readily shared information and established channels for dealing with global adversity. Hospitals have begun preparations including emergency response practice. Suppliers have opened historically propriety processes and licenses to enable extended manufacturing capability (e.g., Roche with Tami-flu, as but one example). Customers have sought (and obtained) information relative to prevention and preparation for a variety of circumstances as well as acted as a source of information back to appropriate authorities regarding infectious incidences, e.g., bird flock deaths. Numerous conferences with multiple stakeholders present have provided forums for knowledge sharing, enhanced understanding leading towards the creation of action plans. In short, bird flu threats have galvanized stakeholders in a way that was unseen in the handling of SARS, in part, as a result of witnessing and experiencing hardship.
Knowledge management provides a focus that can enhance the probability of success in encouraging and sustaining broad-based stakeholder collaboration. Formalized knowledge management promotes the ultimate desire for the benefits of stakeholder collaboration to be sufficiently well developed and supported to offset inherent weaknesses. Knowledge management plays a key role in assuring that aspects of information creation, sharing, and dissemination compatible with multiple stakeholder objectives can be successfully achieved (Alavi & Leidner, 2001). Problems are often beyond the scope of any particular stakeholder, which encourages cooperation in order for success to be attained (Van de Ven, Angle, & Poole, 2000).
The concept of suppler, firm, customer, and government collaboration is sound but operation-alization is difficult and fraught with problems. This doesn’t suggest that the concept should be abandoned, just managed, and supported. Sadly, this situation is not unique (Lyytinen & Rose, 2003). The missing element is often cooperative knowledge creation and exchange. Each element of the collaboration needs a better understanding and focus on cooperation. Unfortunately, this doesn’t naturally exist and easily turns antagonistic. Cooperation is difficult to achieve even when linkages are in place. It is far too easy to say that “details can be worked out.” Unfortunately, the “devil” is in the detail. Towards that end, stakeholder collaboration in achieving knowledge management objectives is paramount.
conclusion
The underlying goal for healthcare is to provide cost effective quality treatment (i.e., realize its value proposition in this challenging environment). In order to do this healthcare needs to maximize its information management techniques and make prudent use of ICTs (Information Communication Technologies). In such a context e-health initiatives will clearly play a dominant role in healthcare delivery. This has been underscored by leaders of US and the EU as well as leading bodies such as the World Healthcare Organization (WHO) that focus on global healthcare issues and policy. Moreover, Both European and US authorities define their initiatives primarily in terms of medical information technology centering on computerized patient record [CPR] or, in more acceptable parlance, the HER electronic health record as referred to by WHO. Hence, e-health is here to stay. What becomes critical then is the sustainability of these e-health initiatives and their ability to bring benefits to the key actor in healthcare, the patient.
This article has set out to delve into the abyss of e-health sustainability. A logical starting place to us seemed to identify the primary drivers in a generic e-business model and then map them into healthcare. Our e-health sustainability model then serves to identify the critical factors and important dynamics faced by any e-health initiative. In addition, we identified the importance of scale and scope economies in this process through the mapping of case study data. Finally, we noted that it is necessary to incorporate the techniques and strategies of knowledge management if superior collaboration between the multiple stakeholders is to ensue. Through the example of SARS we underscored how important this aspect is not only to the sustainability of e-health but in order to realize effective healthcare delivery. Clearly this is only the beginning and we now need further investigation and research, which we plan to embark upon. We close by encouraging other researchers to also delve deeper into this imperative healthcare research area.