abstract
The significance of aligning IT with corporate strategy is widely recognised, but the lack of an appropriate framework often prevents practitioners from integrating emerging Internet technologies (like Web services and mobile technologies) within organisations’ strategies effectively. This topic introduces a framework that addresses the issue of deploying Web services strategically within a mobile-based healthcare setting. A framework is developed to match potential benefits of Web services with corporate strategy in four business dimensions: innovation, internal healthcare process, patients’ pathway, and management of the healthcare institution. The author argues that the strategic benefits of implementing Web services in a healthcare organisation can only be realized if the Web-services initiatives are planned and implemented within the framework of an IT strategy that is designed to support the business strategy of that healthcare organisa-tion.The topic will use case studies to answer several questions relating to wireless and mobile technologies and how they offer vast opportunity to enhance Web services. It also investigates what challenges are faced if this solution is to be delivered successfully in healthcare. The healthcare industry globally, with specific emphasis on the USA and United Kingdom, has been extremely slow in adopting emerging technologies that focus on better practice management and administrative needs. The topic elaborates on certain emerging information technologies that are currently available to aid the smooth process of implementing mobile-based technologies into healthcare industry.
introduction
This topic is based on research—using a longitudinal case study—into the National Programme for Information Technology (NPfIT). NPfIT is an initiative that has been budgeted to cost the UK government £6.3 billion for the purpose of improving the information systems in the National Health Service (NHS), with emphasis on IT infrastructure and the creation of a nationwide patient database.
The significance of aligning IT with corporate strategy in healthcare organisations is widely recognised, but the lack of an appropriate framework often prevents medical practitioners from integrating emerging Internet technologies (like Web services and mobile technologies) within healthcare organisations’ strategies effectively. This topic introduces a framework that addresses the issue of deploying Web services strategically within a mobile-based healthcare setting. A framework is developed to match potential benefits of Web services with corporate strategy in four business dimensions: innovation, internal healthcare process, patients’ pathway, and the management of healthcare institution. The author argues that the strategic benefits of implementing Web services in a healthcare organisation can only be realized if the Web-services initiatives are planned and implemented within the framework of an IT strategy that is designed to support the business strategy of that healthcare organisation.
The topic will also consider certain essential issues regarding the deployment of any mobile data solution (i.e., reliability, efficiency, and security) in the healthcare industry and how such deployment can support healthcare professionals in saving patients’ lives. Using case studies, the topic will answer the following questions:
• Wireless and mobile technologies offer vast opportunities to enhance services, but what challenges are faced if this solution is to be delivered successfully in healthcare?
• Why has the global healthcare industry, with specific emphasis on the USA and United Kingdom, been extremely slow in adopting technologies that focus on better practice management and administrative needs?
• How complacent can IS strategists be to the productivity paradox in the wake of HIPAA (Health Insurance Portability and Accountability Act in USA) and NPfIT (in UK)?
• What emerging information technologies are there to aid the smooth process of implementing mobile-based technologies into the healthcare industry?
The existing economics and IS literature on information-technology adoption often considers network externalities as one of the main factors that affect adoption decisions (Brown & Ven-katesh, 2003). It is generally assumed that potential adopters achieve a certain level of expectations about network externalities when they have to decide whether to adopt a particular technology. However, there has been little discussion on how the potential adopters reach their expectations. This topic attempts to fill a gap in the literature on the adoption of mobile healthcare technology by offering an optimal control perspective motivated by the rational expectations hypothesis and exploring the process dynamics associated with the actions of decision makers in the healthcare industry. They must adjust their expectations about the benefits of a mobile healthcare technology over time due to bounded rationality. The model posed in this topic addresses mobile healthcare technologies that exhibit strong network externalities. It stresses adaptive learning to show why different healthcare organisations that initially have heterogeneous expectations about the potential value of a mobile healthcare technology eventually are able to arrive at contemporaneous decisions to adopt the same technology, creating the desired network externalities. This further allows these organisations to become catalysts to facilitate processes that lead to healthcare industry-wide adoption.
background
The NHS has been responsible for the provision of healthcare and services in the United Kingdom for the past 56 years on the basis of being free for all at the point of delivery. The traditional perception of the NHS is one of a healthcare system organised as a professional guild, with unlimited finance from the government. This type of NHS is experiencing an irrevocable change as taxpayers are no longer complaisant and paternalistic employers are reacting against inflating costs and escalating complaints from the patients. The employer is reacting to the continuous massive flow of subsidies for inefficient physician practices, fragmented delivery systems, and cost-unconscious consumer demand. The patients are increasingly assertive as to their preferences and few have expressed their willingness to make additional contributions for particular health benefits and medical interventions.
Web services are technologies with roots in the Application Service Provision (ASP) business model that are used mostly to automate linkages among applications (Hagel, 2002). They are generally anticipated to make critical system connections not only possible but also easy and cheap (Kreger, 2003; Sleeper & Robins, 2001). One of the perceived benefits of Web services is that organisations would be able to concentrate on their core competencies (Perseid Software Limited, 2003). Service providers argued that the remote delivery of software applications would release managers from the perennial problems of running in-house IT departments, allowing more time to develop IT and e-business strategy rather than the day-to-day operations (Currie, Desai, & Kahn, 2004). This justification has been used in traditional forms of outsourcing over many years (Willcocks & Lacity, 1998).
The NHS is experiencing massive changes in the structure of information systems provision markets and organisations. The local service provision (LSP) and national service provision (NSP) models in use by the NPfIT are in a state of ferment. The payment methods borrow from both capitation and fee for service, and methods of utilisation management are compromised between arm’s-length review and full delegation (Guah & Currie, 2006). LSP and NSP consist of large and more complex entities. These are the result of merger, acquisition, and product diversification. The service providers involved have had to take on a visible feature of ceaseless acquisition and divestiture, integration and outsourcing, and combination and recombination. Providers of medical systems, hospital administration systems, and health plans are coming together and then coming apart. They are substituting contracts for joint ownership, creating diversified conglomerates and refocused facilities, and experimenting with ever-new structures of ownership, finance, governance, and management (Robinson, 2000). These would give the NHSIA (National Health Service Information Authority) the benefits not only of a middle ground between the extremes of vertical integration and spot contracting, but also a balance of coordinated and autonomous adaptation in the face of its ever-new challenges.
The general assumption is that expenditures in the nation’s health will outpace the overall growth in the economy (Collins, 2003; Pencheon, 1998). This is reflected in the percentage of the GDP (gross domestic product) of USA (13%), Germany (10.7%), France (9.6%), and the United Kingdom (7.6%) being devoted to the total cost of healthcare resources (Brown, 2002). Unlike the United Kingdom, however, some of these countries are faced with limitations in social willingness to pay. It has been documented that millions of U.S. residents currently lack the most basic insurance coverage (Institute of Medicine, 2002).
Response to Emerging Technologies in the NHs
Over the years, nontechnologists in the NHS have managed to muddle through one powerful new system after another. Generational strategy is one continuously being used to deal with some of the pressures induced by IS. Adopting such innovations as PCs (personal computers) and the Internet requires the personal and organisational costs of unfreezing deeply ingrained old habits. Many workforces ignore, deny, or deal awkwardly with such technologies.
Srinivasan, Lilien, and Rangaswamy (2004) found several reasons why an organisation should respond to new technology development. Two major reasons are listed below:
• Technological change is a principal driver of competition. This is principally because it destroys monopolies, creates new industries, and renders products and markets obsolete.
• Additional sources—both within and outside the organisation or industry—are increasingly complementing in-house technology development efforts.
A common response to new systems is the “not invented here” (NIH) syndrome (Collins, 2003; Guah & Currie, 2004; Haines, 2002). This often leads to certain organisations rejecting a perfectly useful system based on an implicit assumption that the system does not fully recognise or accommodate their own needs and idiosyncrasies (Brown & Venkatesh, 2003; Davis, 1989). Davis sees this as a likely result of a decline in communication with external sources. NIH syndrome could also result from competences that can be proven to be outdated and inefficient in comparison to an existing technology. One Trust, which places a central role in the direction of regional IS strategy, had to reject a system promoted by the Department of Health because the system was not as familiar as another bespoke system (Haines).
The common characteristics of new systems in the NHS are uniformity in products and prices in the face of great variability in consumer preferences and the actual costs of providing service (Collins, 2003). This one-size-fits-all approach usually leads to services that are of excessive costs for some users and insufficient quality for others, impeding the use of price flexibility to enhance capacity utilisation (Robinson, 2000). Also of concern is a combination of overcapacity and low load factors in some regional trusts with undercapacity and shortages elsewhere. Concerns are growing in the NHS that this may generate cross-subsidies from trusts for which the cost of service will be low to trusts for which the cost of service will be high (McGauran, 2002). Additionally, deregulation of healthcare costs has spurred an outpouring of new services. Consequently, several of these services are the following (Collins; Pencheon, 1998):
• A different cost structure.
• An impact on IS budgets.
• A better match between supply and demand.
Incomplete information has been a fascinating attribute of the NHS’s unusual system’s organisational and normative characteristics. The asymmetry of NHS information between patients and medical practitioners has changed in an exogenous fashion over its 56 years. The amount of healthcare information available to patients is usually the result rather than the cause of changes in the economic and political environment (Robinson, 2000).
Project description: National Programme For Information Technology
The NPFIT is an initiative by the National Health Service Information Authority, born as a result of several plans to devise a workable IS strategy for the NHS (NHSIA, 2003; Wanless, 2002). The NPfIT was designed to connect the capabilities of modern IT to the delivery of the NHS plan devised in 1998. The core of this strategy is to take greater control of the specification, procurement, resource management, performance management, and delivery of the information and IT agenda (NHSIA). ”
The NPfIT is an essential element in delivering the NHS plan. It has created £6 billion information infrastructure, which could improve patient care by increasing the efficiency and effectiveness of clinicians and other NHS staff. The intention of the plan is to address the following (http://www.npfit.nhs.uk):
• Create an NHS Care Records Service to improve the sharing of consenting patients’ records across the NHS.
• Make it easier and faster for GPs (general practitioners) and other primary care staff to book hospital appointments for patients.
• Provide a system for electronic transmission of prescriptions.
• Ensure that the IT infrastructure can meet NHS needs now and in the future.
The decision to implement a national programme for IT into the NHS system complexity is only the first step in the IS modernisation journey for a multifaceted organisation. There are many examples of new technologies disrupting organisational routines and relationships in the NHS (Atkinson & Peel, 1998; Majeed, 2003; Metters, Abrams, Greenfield, Parmar, & Venn, 1997). These usually require both medical professionals and NHS regional trusts managers to relearn how to work together. Orlikowski (1993) and Edmondson (2003) suggest that one technology can be seen differently by two groups of people in an organisation. Findings from Barney and Griffin (1992) and Orlikowski have showed how this could result in the elicitation of different responses for members of that organisation.
scope of Project Work
The topic takes a more in-depth look at the role of the NHSIA (seen as the project leader for the NPfIT), currently the most visible spokesperson and translator for the potential implications of the resulting new technologies. Research has shown NHS IS staff to pay particular attention to what the NHSIA says and does in regard to information systems (Collins, 2003; Ferlie & Shortell, 2001). This research builds on a framework that identifies the key dimensions of the NHSIA tactic that is situation specific for NPfIT assumptions. The work looks at the NHSIA goal and roles for the NPfIT, as well as the role of the private-sector service providers in the implementation of NPfIT.
Here are a few objectives the NPfIT hopes to accomplish:
• To have a series of tightly specified and priced framework contracts on a short list (of about five) primary service providers (PSPs) who can work at the regional and local Strategic Health Authority (StHA) level. This should enforce the integration and implementation partnership—at a national level—during all aspects of the NPfIT project. Each PSP will have an aligned consortium of service providers and vendors for the integrated care resource service element of the NPfIT, and will be mandated to work with the domain PSP for electronic booking, the infrastructure providers, and healthcare providers. StHA PSPs may not make their products exclusive or mandatory to their StHA.
• To create priced packages of national services and applications that the PSPs and StHAs can together implement locally. This activity will include managing the creation of a single Human Resource Information Systems (HRIS) and other national services to access and move health-record information as required.
• To create service-level agreements for the national services and other services out of the scope of the PSP consortium that the PSPs can work toward in providing an integrated service to the StHA
• To develop and maintain the national standards and specifications that all vendors must use. It is also anticipated to create the national business cases required for the Department of Health governance (required by the National Treasury), and to support the local decision-making business cases required at the StHA level. • To procure, under national contracts, a backbone network infrastructure
Such an arrangement provides the greatest clarity in respect to the appropriate allocation of responsibilities and should be well understood in the public and private sectors (see Table 1). Services will be procured on a long-term basis so the combination of local and central funding will be required for at least 5, and preferably 10, years at guaranteed levels.
The Research Study
This study intended to address the gap in the existing literature with regard to the complex issues surrounding the adoption of mobile technology in healthcare. I define mobile healthcare as the use of all kinds of wireless devices (cell phones, personal digital assistants, mobile e-mail devices, handheld computers, etc.) to provide health information and patient-care records to healthcare practitioners, patients, and their caregivers, employers, and employees of health service providers and public regulars of healthcare and services.
Table 1. PSP implementation timetable (as of July 2002)
|
Activity/Output |
Target Date |
|
Agree on procurement strategy (Department of Health (DoH) & local health authorities) |
End Jul 2002 |
|
Service requirement finalized and approved |
End Sep 2002 |
|
Outline business case developed and approved |
End Sep 2002 |
|
Official Journal of European Communities (OJEC) advert |
Oct 2002 |
|
Procurement of systems and implementation services for electronic booking begins |
Oct 2002 |
|
National long list of PSPs created |
Dec 2002 |
|
Invitation to negotiate issued |
Jan 2003 |
|
National short list of PSPs created |
Apr 2003 |
|
First local health authorities begin detailed planning with PSPs |
Aug 2003 |
|
PSP framework contract finalized |
Oct 2003 |
|
Infrastructure provider(s) contract agreed |
Oct 2003 |
|
First local health authorities begin implementation |
Nov 2003 |
|
Infrastructure migration begins |
Mar 2004 |
The findings reported in this topic are part of a larger 5-year research study that was developed to investigate the deployment, hosting, and integration of the ASP and Web-services technologies from both a supply-side and demand-side perspective. The overall research was in two phases. The first phase, comprising ofa pilot study, was conducted in the USA and United Kingdom (Currie et al., 2004). An exploratory-descriptive case-study methodology (Yin, 1994) was used to investigate 28 ASP vendors and seven customer sites in the United Kingdom. The dual focus upon supply side and demand side was critical for obtaining a balanced view between vendor aspirations about the value of their business models and customer experiences, which may suggest a less optimistic picture. The unit of analysis was the business model (Amit & Zott, 2001), not the firm or industry level, so a case-study methodology was anticipated to provide a rich data set for analysing firm activities and behaviour (Currie et al.).
The result from the pilot study led to the funding of two additional research studies by the Engineering and Physical Sciences Research Council (EPSRC) and Economic and Social Research Council (ESRC) respectively. Industrial collaborators were selected for the roles of technology partners, service providers, and potential or existing customers. These studies were concerned with identifying sources of value creation from the ASP business model and Web-service technologies in different vertical sectors (including health).
Research Methodology
The research followed a number of stages involving the use of both qualitative and quantitative data-collection techniques and approaches (Walsham, 1993). A questionnaire survey was distributed by e-mail to businesses and healthcare organisations all over the United Kingdom. These organisations were listed on a national database maintained by the NHSIA, plus those maintained by the university. To ensure relevant managers and practitioners responded, the covering note clearly stated the purpose of the questionnaire and requested that it be passed on to the person(s) with responsibility for managing healthcare e-business strategy. Scales to address the research questions were not available from the literature, so the questionnaire was developed based on the theory of strategic value (Banker & Kauffman, 1988). It included a checklist, open-ended questions, and a section seeking organisational data. Research questions under Part 1 required respondents to answer yes or no if the application of Internet technologies in healthcare were bringing value to patients. Data in Part 2 of the questionnaire were collected by open-ended questions seeking respondents’ views on the best approach to healthcare performance improvement and Web-service value creation. This line of questioning was used to increase the reliability of data since all respondents were asked the same questions, but some added additional information. The purpose was to impose uniformity across the sample of representation rather than to replicate the data obtained from each participant (Yin, 1994).
PATIENT-INFORMATION MANAGEMENT
Healthcare organisations are showing a clear interest in accelerating the transformation of clinical care through the routine use of appropriate emerging technologies by clinicians when diagnosing problems and subsequently planning and administering patient care. To support such noble efforts toward delivering better healthcare to the public, President George Bush and other national leaders have publicly called for the development of a national health information infrastructure. The U.S. government (in 2005) has over the past 2 years published plans for all Americans to have an electronic health record by 2014. Similar to the NPfIT in the United Kingdom, the plans call for a hierarchical set of local, regional, state, and national networks that facilitate peer-to-peer sharing of patient records.
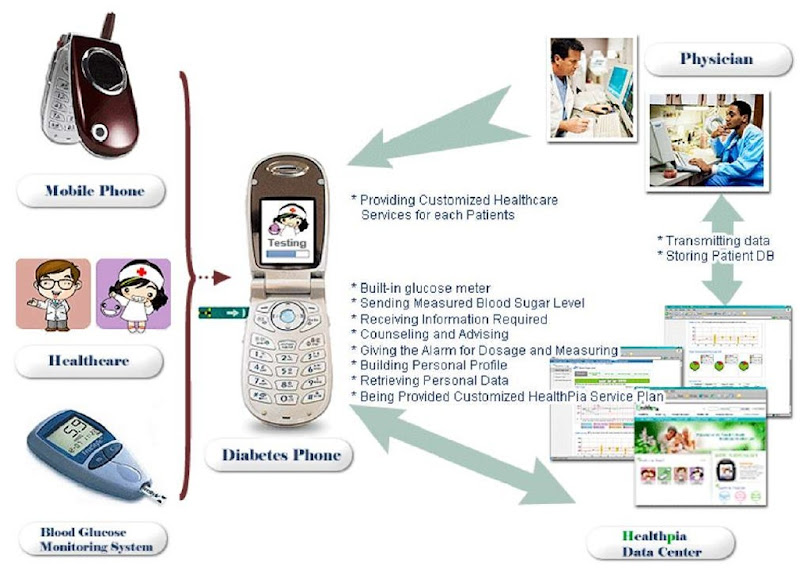
When considering the deployment of any mobile data solution, reliability, efficiency, and security are essential, none more so than in the emergency services if lives are to be saved. To support such communication of critical and personal information, there has been an increased demand for the creation of electronic methods for storing and tracking clinical information (see Figure 1). This requires the solution for some fundamental architectural problems within the healthcare environment: scalability, reliability, recoverability, interchangeable vocabularies, and integration:
• Most service providers can support several thousands of simultaneous log-ons. Many are finding it difficult to demonstrate scalability in thin-client, rules-based order entry or structured clinical information.
• Service providers need to show evidence that they have appropriate schedules for downtime because healthcare organisations require reliability of 99.999% due to the critical nature of the information in the healthcare industry.
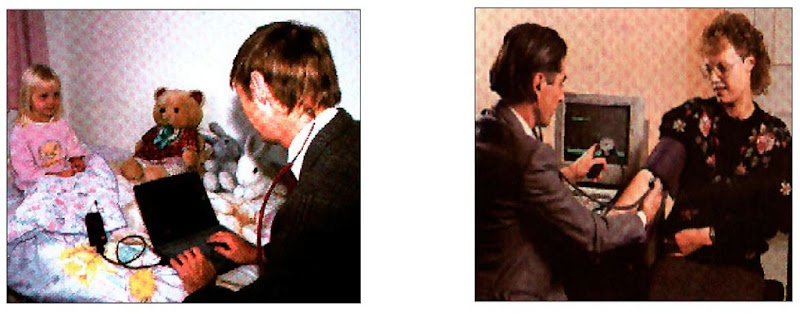
• There has to be a recognisable solution for a very quick data-recoverable plan in the event that downtime or a system failure occurs. Healthcare organisations have to ensure there are fault-proof backup plans to provide medical practitioners with information that is only available in an electronic form in the event that systems become suddenly unavailable. Certain work processes in the healthcare industry (including emergency care, scheduling, registration, order entry, and clinical procedure recording) would need to continue seamlessly, even with a primary-system interruption (see Figure 1). After there has been an interruption, recovery must be complete with no loss of information. Backup, therefore, must prevent any IT failure from making care to the patient impossible. Where mobile healthcare technology is involved, adequate hardware, infrastructure, and tested processes should exist as part of a complete implementation to guarantee this recoverability.
Figure 1. Flexible and independent patient care
Due to a previous lack of harmonized acquisition, healthcare organisations in both the United Kingdom and USA are frequently challenged by a variety of code sets and files that have proliferated across various healthcare institutions. HIPAA attachment transactions (in the United States) and the NPfIT (in the United Kingdom) are beginning to dictate that the future exchange of patient information be carried out electronically between healthcare organisations. To facilitate this portable and interoperable mobile healthcare technology, certain local vocabularies need to be replaced and the use of government-specified code sets should be synchronized. The way forward is to maintain current systems and historic data through mapping infrastructures that manage the correct translation, giving semantic meaning to patient data with the hope that one day soon there will be a complete migration to common vocabularies.
Many applications currently in the NHS have been designed with the assumption that that the approach and architecture does not need to coexist and interoperate. While some of these may support integration with other applications that also have significantly different philosophical stances, they do not fully recognise that the need for a healthcare organisation to implement a total solution involves the practicalities of many different dimensions of time, scope, economics, and service providers’ organisational politics. Toward this goal, all interoperability for a mobile healthcare technology should require that all features and functions work across all applications. The NPfIT proj ect is proving that all service providers have to significantly alter their current approach to internal and external integration, security, and nomenclatures during the life of the project.
case 1: MotoHealth
Motorola, along with its partners, initiated a tele-medicine service at Harvard Teaching Hospital called MotoHealth (http://www.motorola.com/mediacenter/news/detial) late 2004. The Motorola solution uses mobile phones to help healthcare professionals to monitor chronically ill patients during their normal daily routines. This product was designed to meet the customer’s convenience, and as a discreet way of monitoring patients in the mobile environment, can replace in-home hospital and home monitoring devices. As a result, it gives the patient more independence to continue daily activities virtually anywhere they like. This method to providing healthcare pushes healthcare and services out of high-cost health institutions. It enables the patient’s body to become the point of care and the mobile healthcare technology becomes the bridge to the patient’s body, thus, enabling the delivery of care, educational advice, and support remotely and transparently.
This case has proven that when a mobile healthcare technology is implemented as part of a comprehensive healthcare program, it can give healthcare providers useful daily updates on a patient’s physiological levels such as blood pressure, glucose level, and weight control. Such a method of healthcare facilitates proactive treatment action, resulting in fewer hospitalizations and visits to emergency rooms, potentially lowering the increasing demand on the costs of providing healthcare and services to the public.
Policy Issues
Arguably, the most viable techniques for successful mobile healthcare technology implementation are practical guidelines and good management practices. Policies established by a healthcare organisation are the first steps toward this goal.
There are, however, few steps for establishing a policy for mobile healthcare technology:
Guidelines must be developed for the acquisition of mobile healthcare technologies. This would balance the need to encourage innovative applications against wasteful spending, which can be seen by certain members of the staff as duplication of effort. This in turn makes it the responsibility of every medical practitioner who may need a particular type of application to strictly adhere to this policy.
There must be regular inventory taken. This helps to identify and evaluate all installed hardware and software before setting or changing the standards. These would certainly affect policy decisions and future acquisitions. While standards can sometimes be looked upon as restrictive in the IT industry, medical practitioners actually see these to offer benefits for the care providers and the patients alike. Nearly all healthcare organisations have standards that cover many aspects of their operations within the healthcare process. Generally, standards in the NHS are recorded in formal standards and procedures manuals, but in certain cases, we came across informal handwritten notes (i.e., “this is the way we do things here”) that are also considered to be standards.
Ruyter, Wetzels, and Kleijnen (2001) show how organisations implementing e-commerce first learn to exploit the Internet for information transfer before supporting transactions, and then finally use it for commercial trading and collaboration among various actors. Considering mobile healthcare is still in its infancy, borrowing from the e-commerce experience will mean that healthcare organisations will probably adopt wireless e-business methodologies first to support their existing healthcare processes and improve efficiency before they come up with new business models to transform the competitive landscape in the healthcare industry.
In the case of the NHS, wireless enterprise implementation issues frequently extend well beyond the technology domain and into areas of medical practices and organisational culture (see Figure 2). Nearly all the regional healthcare trusts that are actively pursuing wireless enterprise strategies at the moment are handcrafting solutions around their own local IT infrastructures and their own homegrown healthcare processes partly because there are very few packaged mobile healthcare solutions on the market.
The focus, currently, is on accessing information via wireless mobile healthcare messaging. However, the future should hold more applications like mobile access, telemedicine, and alerts for facilitating better disease management and controls. Given the emerging state of mobile technology and its potential impact on healthcare, mobile healthcare can be seen as truly radical. Mobile healthcare has the potential to remake this entire industry and obsolete established strategies. Most healthcare organisations in Western Europe and North America feel they must participate in this emerging healthcare technology in order to survive the increasing demand to service a continuously evolving patient environment.
Figure 2. Home visits and general-practice consultation
The research found two reasons why healthcare organisations are beginning to pay keen attention to mobile healthcare:
• These organisations are being defensive. There is a general belief that newcomers in the healthcare-provision market may be plotting to use new functionalities available through the use of mobile healthcare to attack the incumbents’ core providers.
• Converse to the previous reason is the understanding that mobile healthcare could realize its potential. If this happens successfully, mobile healthcare would be too attractive a proposition to ignore, and joining in at a later date may prove too expensive.
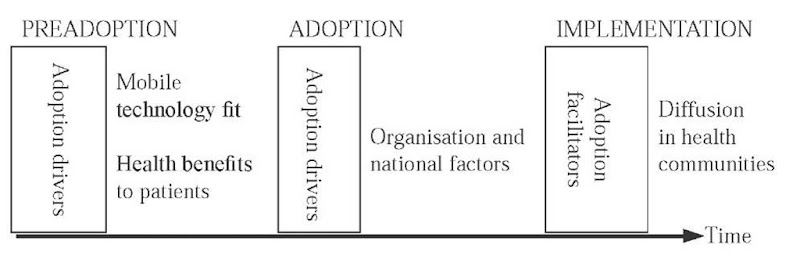
The author poses a conceptual framework for the research upon which this topic is based, showing the different stages of the technology-adoption process for healthcare organisations as well as the main factors operating at each stage (see Figure 3). In the preadoption stage, healthcare organisations take an internal perspective and analyse the fitness of the mobile healthcare technology for the contemplated task as well as the value of this technology. These should be the drivers of the adoption decision. The phase after that shows the healthcare organisation analysing whether organisational and environmental factors are favourable for continuing with this novel technology. This may uncover inhibitors that could slow down the adoption process. In situations where the healthcare organisation decides to implement the mobile healthcare technology in the next stage, it should find adoption facilitators that can help in the diffusion of mobile technology within the healthcare environment. Readers should note that implementation is beyond the scope of this framework.
This framework borrows from the technology-organisation-environment framework put forward by Tornatzky and Fleischer (1990) as well as the deinstitutionalisation framework by Tolbert and Zucker (1994). Tornatzky and Fleischer’s framework identifies three aspects of an organisation’s context that influence the process by which it adopts and implements innovation: technological context, organisational context, and environmental context. The omission of environmental context here is due to the fact that this topic is about a single industry in which the environment is held constant.
The author considers innovation in healthcare as an idea, medical practice, or any material artefact in the healthcare process that is perceived to be new by the relevant unit of adoption in medical treatment. The relative advantage, compatibility, complexity, trial, and observation of such innovation can usually be used to determine the tendency for its adoption in the healthcare environment.
Figure 3. Conceptual framework of mobile healthcare technology adoption
By relative advantage, the author means the degree to which an innovation within the health industry is perceived as better than the idea it supersedes. Compatibility, on the other hand, is seen as the degree to which an innovation within the health industry is perceived as being consistent with the existing values given by a particular healthcare community, or with past experiences and needs of potential adopters within the healthcare process. Compatibility of mobile healthcare technology can also be explained in terms of a combination of what healthcare practitioners feel or think about a particular innovation. This would also involve a critical look at the practical and operational compatibility with what healthcare practitioners are doing in the ongoing healthcare process. This interpretation of compatible innovation is in conjunction with perceived usefulness, the degree to which an end user believes a certain system can help perform a certain medical task. Complexity is the degree to which an innovation within the health industry is seen to be difficult to understand and use within the healthcare industry.
The trial of an innovation within the healthcare industry is an important part of evaluating new technologies within this critical industry. It is the degree to which an innovation within the health industry is experimented with on a limited basis. Given an opportunity to experiment with a new mobile healthcare technology before decisions are made about the adoption is an important benefit, especially for emerging technologies. This is an industry where practitioners take very highly the availability of information, while learning from experiences with previously disappointing IT projects.
Observation is a reliable means by which the healthcare industry evaluates innovations. This process identifies the degree to which the performance of a mobile healthcare technology and related benefits to the patients are visible to the medical practitioners and not only the service providers.
The determinants of mobile healthcare technology adoption are the benefits to the patients vs. the cost of such adoption. Most often, the NHS measures this in terms of the difference in costs for the shift from a previous technology to a mobile healthcare technology. Also worth considering are several factors that are important to the health service, such as the improvements made to the healthcare process as a result of a mobile healthcare technology after its introduction. There might even be a discovery of new uses for the mobile healthcare technology and the development of certain complementary inputs.
Hartmann and Sifonis (2000) relates to some of these features of mobile healthcare technology application by the identification of four dimensions within an organisation: leadership, governance, technology, and operational competencies. By leadership, they referred to the process of managing the initiatives and how the host organisation should stay motivated throughout the adoption process. By governance, they referred to the process of organising the innovation as regards the structure and operating procedures. Technology is where Hartmann and Sifonis looked at the organisation’s ability to rapidly develop and implement new applications. They finally explained operational competencies as the way the host organisation manages the coordination of the relationship between leadership, governance, and technology as well as exploiting the available resources.
Levy and Powell (2005), on the other hand, presented evidence—from their study of small and medium-sized businesses in the United Kingdom—that the adoption of emerging technologies posits a similar framework as adoption related to the readiness of organisations taking into consideration the perceived ease of use and perceived usefulness. The readiness of the NHS to adopt mobile healthcare technology can be determined by reviewing the financial and technological resources available as well as various other factors dealing with the compatibility and consistency of emerging technologies with organisational culture and values.
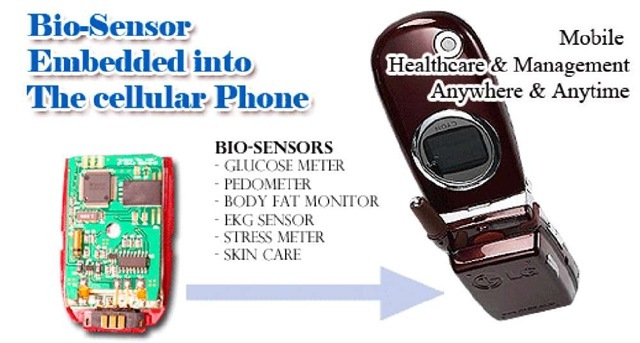
Case 2: Pervasive Monitoring system
Oracle, along with its London partners, piloted a wireless sensor interface technology platform in mid-2005 (http://www.toumaz.com/news.php?act). It used advanced transactional database capabilities and offered the potential to transform the treatment and management of chronic diseases for millions of patients. This project was meant to bring the economies of scale of semiconductors into the healthcare industry with its advantages of real-time, personalised care and the delivery of some form of breakthrough. The system was based on a low-cost, disposable, integrated sensor interface chip.
Due to the chip’s ultra low power and very small battery size, it could be worn on the body with complete freedom of movement, or it could be implanted. Such a mobile healthcare technology is compatible with a wide range of sensors (see Figure 4) and can therefore be configured to detect vital signs such as ECG (electrocardiogram), blood oxygen and glucose, body temperature, and mobility. The device can also dynamically process and filter event data (including irregularities in heartbeat or blood pressure) and send the details to a mobile phone or PC via an ultra low-power, short-range radio telemetry link.
Further improvements to this kind of mobile healthcare technology could enhance the quality and efficiency of the healthcare patients of the NHS receive in the future. It could permit the following in future healthcare:
• Provide more timely and personalised care.
• Deliver unprecedented freedom, flexibility, and control for patients.
• Include exciting possibilities for medical practitioners to ultimately offer consumer items for which selection is based on quality and efficiency.
Figure 4. Mobile healthcare technology with built-in sensor
conclusion
This topic has provided examples of mobile healthcare technologies (case studies) for which the successful delivery of mobile solutions can help with certain kinds of emergency services. When considering the deployment of any mobile data solution, reliability, efficiency, and security are essential, none more so than in the emergency services if lives are to be saved. Wireless and mobile technology offers the opportunity to vastly enhance services, but there are still challenges to be faced if a cost-efficient solution is to be delivered.
Although some of these initiatives described as e-health can deliver certain benefits (including increased productivity and effectiveness of healthcare personnel and improved delivery of information and services), they will be faced with a number of challenges. Service providers in the private sector are looking to government for more leadership on identification issues and, as such, mobile healthcare technology should be a welcomed measure.
IT is seen as a key driver in the delivery of an efficient public sector, but how can departments justify further expenditure and eventually provide a clear road map to return on investment whilst delivering what has been promised? Also, what are the key short-term issues and, more importantly, the solutions that government departments can focus on? This panel will examine the savings that ICT investment is expected to deliver in the public sector, and how to serve more people by making things more efficient.
The United Kingdom has certainly increased its uptake on open-source software since the Office of Government Commerce’s (OGC’s) announcement that open source is a viable desktop alternative for the majority of users. However, many government organisations have chosen to remain with their existing proprietary software. This panel will examine the advantages and the drawbacks of both software solutions.
While this topic is not intended to give specific guidelines for using mobile healthcare technologies, the author finds it useful to mention the following two points:
• Have clear objectives. Mobile healthcare technology is only a means to an end. It is advisable for managers of healthcare organisations to not be dazzled by the technology.
• Mobile healthcare technology is a unique medium, requiring management to capitalize on its uniqueness. The information being transmitted by mobile healthcare technology is the same, but is just delivered in a different way.
A conceptual framework has been posed from the research upon which this topic is based, showing the different stages of the mobile healthcare technology-adoption process for healthcare organisations as well as the main factors operating at each stage.
In conclusion, the author has argued that Web services can aid the strategic planning of a healthcare organisation and can be used for competitive advantage. Web services can also contribute to improving our understanding and management of the critical issues surrounding mobile-based healthcare. Such understanding not only avoids disastrous consequences during the adoption of information systems, but also proves essential in supporting healthcare professionals to effectively manage the current trend of rapid increase in healthcare costs.