abstract
The clinical management of premature and ill term babies is challenged by the necessity of several inter and intra organizational patient journeys. Premature and ill-term babies born in regional Australia and Canada must be moved to another hospital with Neonatal Intensive Care Unit (NICU) facilities. NICU babies requiring surgery must be moved to a Level IV NICU for surgery. Current clinical management supports the transfer of limited patient data via paper or telephone exchange. In this article a framework for the design of Web-service-based clinical management systems to support inter and intra organizational patient journeys is presented. A series of Web services are described and integrated and coordinated through BPEL processes enabling greater support for inter- and intra-organizational transfer of patient data. This framework is demonstrated through a NICU case study. A key benefit of this framework is that it enables the establishment of “on demand” patient journeys eliminating the need to establish permanent point-to-point connections.
introduction and motivation
Healthcare and specifically the allocation of funds towards improved provision of healthcare via improved patient journeys represents a significant portion of the Australian, USA, United Kingdom, and Canadian National Budgets (Curry, McGregor, & Tracy, 2006).
Patient Journeys document a pathway of Clinical Management guidelines that represent the patient’s journey through treatment and care.
Clinical Management systems are designed to assist care providers in diagnosis and treatment using existing already established methods of diagnosis and accepted treatments (Gross-Portney & Watkins, 2000).
Health care redesign and in particular patient journey redesign (also sometimes referred to as patient pathway or flow) involves analyzing the overall processes involved with the intra- and inter- organizational movement of a patient and then identifying how this journey can be improved via the removal of wasted and excessive activities, process duplication and improved communications between the patient, their carers and the clinicians involved with thejourney itself. Process redesign techniques have been used extensively in the business, manufacturing, and computing domains for many years but it is only recently that process improvements in healthcare have been achieved through similar reengineering approaches (Curry, McGregor, & Tracy, 2006).
In general, the research, development and adoption of new information technologies (IT) and information systems (IS) within the healthcare domain is currently lagging behind other industries (McGregor, 2006; Wu, Wang, & Lin, 2005).
Web services enable standardized information exchange through XML messaging. Business Process Execution Language for Web services (BPEL) (Andrews et al., 2003) provides a mechanism to integrate and coordinate the invocation of several Web services within the structure of a business process. Web-service-enabled Patient Journeys have the potential to significantly impact the effective expenditure of these funds by enabling paradigm shifts in Clinical Management.
This article presents case study based research supporting the development of a framework for the design of Web-service-based Clinical Management systems to support intra- and inter-organizational patient journey workflows. The framework enables the modeling of existing patient journeys and supports the reengineering of these patientjourneys to improve communication between clinicians and remove duplication, wasted, and excessive activities. Web services are designed that enable greater support for inter- and intra- organizational transfer of patient data. This research builds on existing model-driven Web services integration and development research (Bordbar & Staikopoulos, 2004) by further applying these concepts researched within the business context to the domain of clinical management activities within a patient journey. To facilitate the coordination of the complete inter and intra organizational patientjourneys, Business Process Execution Language for Web services (BPEL) is used as BPEL enables the generation of executable workflows built using Web services. A key benefit of this framework is that it enables the establishment of “on demand” patient journeys eliminating the need to establish permanent point to point connections.
The case study used for this research is the patient journey of neonatal and ill-term babies between (1) special care nurseries in urban, rural, or remote hospitals to tertiary or children’s hospital Neonatal Intensive Care Units (NICUs) and (2) tertiary NICUs and children’s hospital NICUs, when a baby is transferred for surgery.
The article is organized as follows. First a discussion is presented on related recent research in the areas of health informatics to support ICUs together with recent Web services and BPEL research. The next section presents an overview of the framework for the design of Web service based clinical management patientjourneys. The following section introduces the Neonatal Intensive Care Unit (NICU) case study environment. Afterwards, the application of the framework to generate BPEL process to support neonatal patient journeys is presented. The article is concluded where future work is presented.
related work
Much of the recent computing and IT related research to support intensive care units (ICUs) has focused on clinical alerts (Catley & Frize, 2003; Catley et al., 2003; Shabot, LoBue, & Chen, 2000; Sukuvaara, Makivirta, Kari, & Koski, 1989; van der Kouwe & Burgess, 2003). The information made available to these systems is limited to a small set of physiological data and/or clinical data from patients located within their ICUs. Clinician access to these systems is limited to the receipt of alerts with minimal content via email and in some cases pagers.
An integrated XML-based health care framework for a neonatal intensive care unit is described by Catley and Frize (2003) and Catley, Frize, Walker, and StGermain (2003). That research enables the capture of local real-time patient device data within a data repository located within a data collection unit (DCU). It utilises XML as a means to transfer data from a NICU data repository to clinical decision support system (CDSS). The transmission of the data from the medical devices to the DCU is not in XML.
Kregar (2001) defines a Web service as an interface that describes a collection of operations that are network-accessible through standardised XML messaging. Web Service Definition Language (WSDL) supports the implementation of Web services by providing a standard XML format for describing network services as a set of endpoints operating on messages containing either document-oriented or procedure-oriented information (Christensen, Curbera, Meredith, & Weerawarana, 2001).
Business Process Execution Language for Web Services (BPEL) defines a notation for specifying business process behaviour based on Web services (Andrews et al., 2003). There has been recent focus on linking process modeling with Web services development resulting in model driven Web services integration and development (Bordbar & Staikopoulos, 2004).
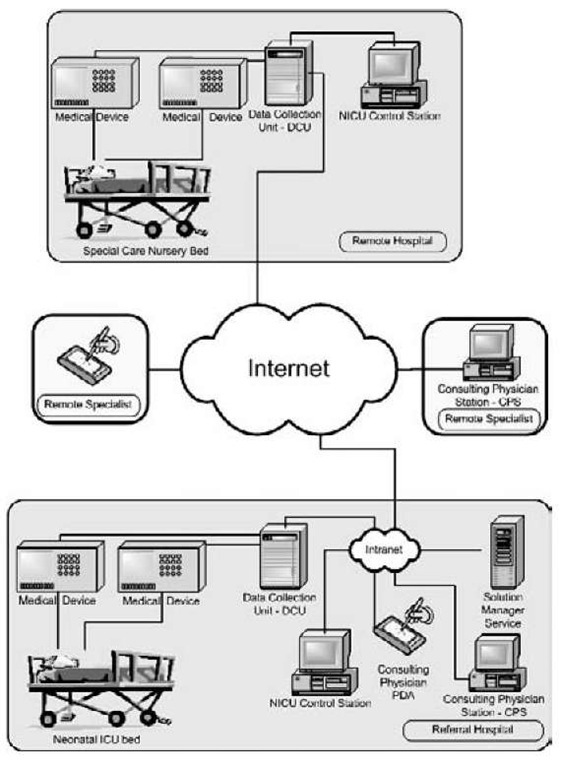
Figure 1. e-Baby architecture
This research is part of the larger “e-Baby” research project (Foster & McGregor, 2006; McGregor, 2005; McGregor, Bryan, Curry, & Tracy, 2002; McGregor, Heath, & Wei, 2005; McGregor, Kneale, & Tracy, 2005, 2006). The broad aims of the e-Baby project are to develop:
• Generic computer interface technologies to allow the integration of data emanating from several disparate medical monitoring systems and a clinical information database.
• Data management technologies to allow for the detection of trends and patterns in clinical and real-time physiological data.
• An Internet-based data distribution mechanism which is capable of integrating data from a number of cooperating data sources while supporting access security controls down to a specific item within a specific individual’s medical record.
The e-Baby architecture defines architectural components located at Referral Hospitals containing NICUs, Remote Hospitals with Special Care Nurseries and supports remote and Referral Hospital access by Neonatologists.
The Solution Manager Service (SMS) architecture within the context of its use for business performance measurement is introduced in (McGregor & Schiefer, 2003, 2004; McGregor, Schiefer, & zur Muehlen, 2006; Schiefer & McGregor, 2004). The SMS is an agent-based intelligent decision support system that allows organizations to collect information about their business processes in a centralized repository, and share them among authorized parties, such as supply chain partners, clients, or government agencies. A key contribution of that research is that the interaction with this IDSS is via a set of Web services. In addition, the infrastructure boasts several innovative agent-based modules that support different components, providing the intelligence within this IDSS (McGregor, Schiefer et al., 2006). Within that research business process audit stream data is transmitted to the SMS via the use of a log Web service. The e-Baby research reapplies the principles of the SMS within the context of receiving and processing physiological stream data via a physiological log Web service.
This article focuses on the framework that enables the coupling of various previously defined e-Baby components (Foster & McGregor, 2006; McGregor, 2005; McGregor et al., 2002; McGregor, Heath et al., 2005; McGregor, Kneale et al., 2005, 2006) using Web-services-based Clinical Management systems to support intra and inter organizational patient journey workflows.
Framework for the design OF WEB service BAsED clinical management patient journeys
In this section the framework to enable the establishment of Web-service-based clinical management patient journeys is introduced. The framework builds on previous model driven Web service integration and development research (Bordbar & Staikopoulos, 2004) and proposes the following phases:
1. Model the existing patient journey
2. Reengineer the patient journey
3. Determine inter and intra information flows
4. Web Services Design
5. BPEL Design
6. Development/Testing/Implementation Phase
7. Post Implementation Evaluation
Each phase within the framework is briefly described in the following subsections. An NICU case study is used to demonstrate this framework in the following section.
Existing Patient Journey Model
During this phase information is gathered to enable the construction of patient journey model. Participants may include management, IT support staff, healthcare workers, patients, and their carers. This framework enables the patient journey to be modelled within a chosen patient journey/ business process modelling tool. In this article, cross-functional flowcharts have been used to diagrammatically represent the existing patient journey. Further research has commenced on a patientjourney modelling and communication tool for use during this phase that better supports the domain of healthcare (Curry, McGregor, & Tracy, 2006). Output from this phase is the documented existing patient journey model.
Reengineer the Patient Journey
The patient journey is then reengineered during this phase. To enable this reengineering focus sessions are run by an experienced facilitator whose role it is to encourage discussion and involvement amongst the participants and translate what is said into a resulting diagrammatic.
Output from this phase is the documented reengineered patient journey model.
Determine Inter and Intra Information Flows
Once the reengineered patient journey has been established, information flows are defined for each communication between the participating organization units. XML schemas are then constructed to represent information flows. The outputs from this phase are the associated XML Schemas.
Web services Design
For each information flow between organization units that has been defined by an XML schema, Web services are designed to support the intra-and inter-organizational transfer of information. Output from this phase is the design of the Web services.
BPEL Design
During this phase the patient journey model is utilized to provide the information to enable the translation of the patient journey into a Business Process Execution Language for Web Services (BPEL) design. Organizational participants in the patient journey become partners in the BPEL definition. Web Services are invoked at the appropriate place in the patient journey. The output from this phase is the BPEL representation of the patient journey.
Development/Testing/ Implementation Phase
The Web services and controlling BPEL are developed, tested, and implemented using the chosen development lifecycle during this phase. The BPEL representation of the BPEL journey and the associated Web services are implemented during this phase.
Post Implementation Evaluation
Once implemented, the patient journey is evaluated. Evaluation within this context is performed via clinical trial to evaluate performance based on the clinical management requirements. In addition, further performance evaluation is performed based on system performance measurement to assess system performance. Output from this evaluation will drive future iterations of this framework.
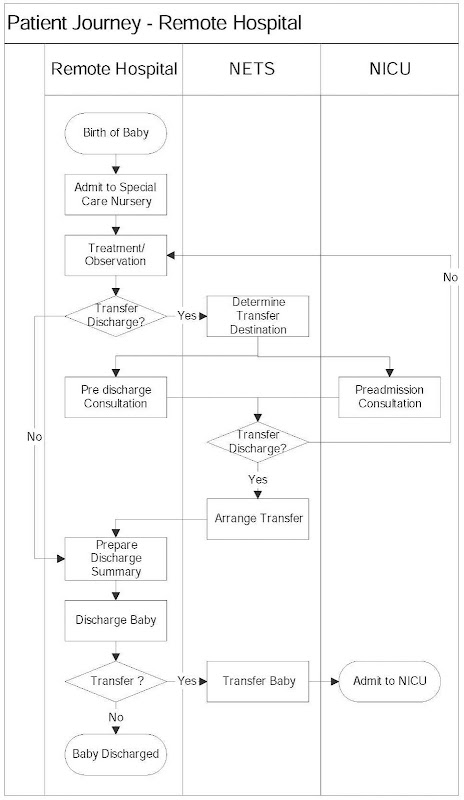
Figure 2. Neonate or ill-term baby patient journey—remote and referral hospital
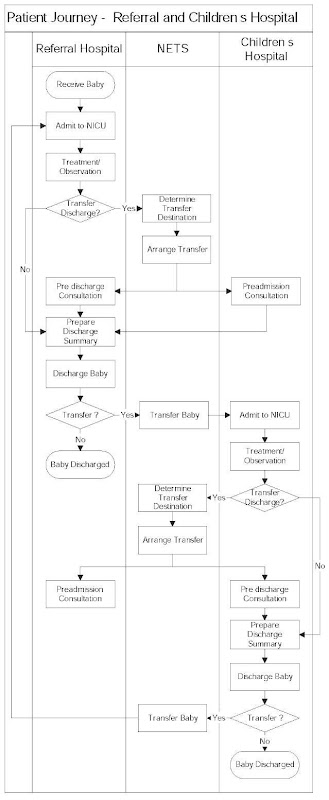
Figure 3. Neonate or ill term baby patient journey—referral and Children’s Hospital
NEONATAL INTER AND INTRA ORGANIZATIONAL PATIENT JOURNEYS
The framework to enable the establishment of Web service based clinical management patient journeys is now demonstrated using neonatal inter- and intra-organization patient journeys.
Intensive care units (ICUs) worldwide offer support for patients in need of critical care. They boast a range of state of the art medical monitoring devices to monitor a patient’s physiological parameters such as blood oxygen, blood pressure, and heart rate. Other devices such as ventilators offer mechanical life support.
Broadly, there are three types of intensive care namely, adult, pediatric, and neonatal. While the age of the patient is the differentiator between adult and pediatric ICUs, the clinical management differs greatly from these ICUs to the neonatal ICUs (NICUs)—where gestational age greatly impacts clinical management.
From a total of 86,414 babies born in New South Wales (NSW), Australia during 2003, 15 percent (12,296) required admission to a special care ward and 2.6 percent (2,277) were admitted to neonatal intensive care units (NICUs). These figures are similar to previous years (NSW Midwives, 2004). Premature babies can be up to 17 weeks early and may only weigh 450gms; they can spend three or four months in intensive care and have dozens of specific diseases before discharge. Ten percent of severely ill babies will die and 15 percent of survivors will have significant life-long disability. Premature babies, by the time they are discharged, can increase in body mass by as much as six times, and have had dozens of medical diagnoses and treatments. Many of these may have long-term implications for the future health of the individual. In addition, 15 percent of neonatal intensive care admissions are transferred after delivery from smaller regional or remote hospitals without intensive care facilities to larger tertiary referral or children’s hospitals with Neonatal Intensive Care Units (NICUs). Similar conditions apply within Australia, New Zealand, Canada, and the USA where small non-tertiary units are spread throughout the country (McGregor, Kneale et al., 2006).
The NSW newborn and paediatric Emergency Transport Service (NETS) is the state wide clinical service for medical retrieval of critically ill newborns, infants, and children in NSW, Australia. Since 1995 NETS neonatal retrievals from regional hospitals to tertiary referral or children’s hospitals has averaged 70 per month. There are only three children’s hospitals in NSW, (two children’s hospitals in Sydney and the John Hunter Children’s Hospital in Newcastle). Children’s Hospitals contain NICUs and in addition, are able to perform surgery on Neonates. Another seven hospitals are tertiary referral hospitals providing NICUs onsite for newborn babies. All of these hospitals are in major metropolitan areas on the eastern coast of NSW. There are approximately 200 other hospitals in NSW without specialist NICU care that must refer to Neonatologists within the NICUs at either the children’s or tertiary referral hospitals for the care of critically ill newborns and infants.
Current treatment practices for premature babies and ill-term babies born in geographically rural and remote hospitals are impacted by the lack of NICU support onsite. Regional hospitals have equipment to provide limited NICU support, but without the ability for a Neonatologist to receive information from this equipment, the baby must be moved to another hospital with Neonatologist support. Given the critical requirement to maintain a consistent environment, moving a baby at this time can be life threatening. Transferred pre-term and critically-ill-term babies have higher mortality rates and much higher rates of long-term disability than similar babies born in hospitals with NICU facilities (McGregor et al., 2002). A major limitation is that the attending physician must contact a Neonatologist via telephone, who may or may not be located at the NICU at that time, to describe the baby’s condition and, where possible, relay any physiological information verbally. The consulting Neonatologist must then make decisions based on this verbal exchange.
It is very common for critically ill babies to have significantly abnormal variation in the measured parameters minute by minute and not all of these variations are made available to the consulting Neonatologist. Frequent transient falls in blood pressure and blood oxygen content, often with swings into the high range, may be of critical importance in survival and quality of survival free of significant disability (Lister, Bryan, & Tracy, 2000).
Adding to the complexity of this neonatal support function, the NICUs located at the children’s hospitals and tertiary referral hospitals each have a limited number of humidicribs. As a result, the remote hospital attending physician must contact NETS who utilise their referral database to determine which children’s or tertiary referral hospital NICUs the remote hospital should contact for support and/or transfer, based on humidicrib availability. Thus the NICU patient journey support that the approximate 200 regional and tertiary referral metropolitan hospitals require is an adhoc connection to any of the Children’s or Tertiary Referral hospital NICUs (10) for which they are referred to by NETS, on a needs basis, at a total rate of 70 per month (McGregor, Kneale et al., 2006).
Typical medical records for the most premature babies consist of manually prepared paper notes that detail enormous data collection and can weigh up to three to four kilograms. The preparation of these notes is dependent on the hand-annotated records of nursing staff, usually at 60-minute intervals, and 30-minute intervals at best. Also, within the NICUs, the collection of the information contained within the baby’s notes to form a discharge letter represents a manually intensive analysis of physiological statistics, together with the replication of clinical data that can take the Neonatologist many hours to produce.
The following subsections present and describe the use of the framework proposed within this research on two high-level patient journeys namely: neonate or ill-term baby patient journey—remote hospital; and neonate or ill-term baby patient journey—referral hospital. The example commences with the second phase where the improved patient journey model has been developed and concludes at the BPEL Design.
Reengineer the Patient Journey
Neonate or Ill Term Baby Patient Journey—Remote Hospital
The neonatal or ill-term baby patient journey where the baby is born in a remote hospital is summarised in Figure 2. A neonate or ill-term baby born within a Remote Hospital firstly goes through the activity of Admit to Special Care Nursery (ie. placed within a humidicrib in the Special Care Nursery). They then begin to undergo Treatment/Observation. During the Treatment/ Observation, the attending paediatrician will constantly access the baby’s condition. While the care of neonates on a daily basis is quite complex and requires in simple terms nutrition planning, observation, and treatment, of relevance to this research is the point in the treatment/observation activity determining whether the baby can be discharged, or whether a discharge via transfer to a NICU may be required. If a transfer may be required, they will contact NETS to determine the transfer destination. Once NETS has allocated a humidicrib within a receiving NICU, the pediatrician at the remote hospital will contact the receiving on-call neonatologist from the NICU (who may or may not be located within the NICU at that time) for a predischarge/preadmission consultation and to determine whether a transfer discharge is required. If they decide not to transfer the baby the paediatrician continues the treatment/observation activity. If they decide a transfer discharge is required, NETS is contacted again to arrange the transfer. The pediatrician will then prepare the discharge summary. If the discharge is a transfer, NETS perform the activity of transferring the baby.
Neonate or Ill Term Baby Patient Journey—Referral Hospital
The neonatal or ill-term baby patient journey for a baby admitted into a tertiary hospital’s NICU is summarised in Figure 3. Once admitted to the NICU, they then, similarly to that defined earlier, begin to undergo the complex Treatment/ Observation activity. Of relevance to this research is the point(s) during the treatment/observation activity that the attending neonatologist will assess whether the baby can be discharged, or whether surgery may be required. If surgery may be required, then a transfer will be required. They will contact NETS to determine the transfer destination to confirm which children’s hospital the baby will be transferred to. Once NETS has allocated a humidicrib within a receiving NICU, the Neonatologist at the tertiary hospital will contact the receiving on-call neonatologist from the children’s hospital NICU (who may or may not be located within the NICU at that time) for a predischarge/preadmission consultation prior to surgery and to arrange the transfer. The neonatologist will then prepare the discharge summary. If the discharge is a transfer, NETS perform the activity of transferring the baby. Within the children’s hospital, the baby undergoes the same patient journey as that of the referral hospital. The surgery is performed during the treatment/observation. Once the baby is stable post surgery, NETS are contacted to arrange the return of the baby to the tertiary hospital NICU and a similar transfer process proceeds.
Determine Inter and Intra Information Flows
As can be seen from Figure 2 and Figure 3, in-terorganization information flows are required to support the following activities:
1. Determine Transfer Destination
2. Predischarge/Preadmission Consultation
3. Transfer Baby
Determine Transfer Destination
The pediatriciation/neonatologist require the ability to contact NETS to determine where a humidicrib is available to receive the transferred baby.
Predischarge/Preadmission Consultation
The neonatologists located at both the children’s hospitals and tertiary referral hospitals require the ability to obtain information from the monitors attached to babies that are not physically located at that specific hospital, but perhaps at another regional hospital where only limited support for premature babies exists. Similarly, a Neonatolo-gist need not be located within the hospital to view patient data, but should be free to view this information through any secure Internet/Intranet connection.
Transfer Baby
Remote hospitals require the ability to send discharge information through to the receiving NICU in a standardised format to enable the receiving NICU to integrate the information directly within the receiving hospitals database.
In addition, there is a need to extract information from NICU databases to automate the preparation of discharge information to be sent to the receiving NICU.
Finally, the pediatriciation/neonatologist requires the ability to contact NETS to confirm the execution of the transfer.
Web services Design
To support the information flows required as detailed in the previous section, five Web services are required to satisfy each of the listed information flow functions namely the:
1. Availability Web Service established by NETS
2. Physiological Log Web Service established by each NICU
3. Allocation Web Service established by NETS
4. Clinical Web Service established by each NICU
5. Analyse Web Service established by each NICU
Each Web service is detailed briefly below.
Availability Web Service
A database of all receiving neonatologists, together with their hospital’s details are contained within the Referral Database. This information provides details based on humidicrib availability. The Referral Database is located within NETS and accessible via a set of Web services. The Availability Web Service forwards details of the receiving Neonatologist together with the details for the receiving Neonatologist’s Physiological Web Service. Further details on Web services by NETS are contained in (McGregor, Kneale et al., 2005, 2006).
Physiological Web Service
To address the need for standardising physiological data transmission, a Web service based framework for the transmission, display, and storage of physiological data for local and remote neonatal intensive care has been established known as the physiological Web service. The Web service enables transmission of time interval packets of physiological data through the physiological Web service by sending Physiological Log Packets and receiving Acknowledgements. Further details on the physiological Web service are contained in (McGregor, Heath et al., 2005; McGregor, Purdy, & Kneale, 2005).
Allocation Web Service
This Web service enables NETS to be advised of the execution of the transfer.
Clinical Web Service
This Web service enables the receiving NICU to advertise the standardised format to receive discharge information from other hospitals
Analyse Web Service
This Web service enables NICUs to extract discharge summary information from their systems to send to receiving NICUs via their Clinical Web Service.
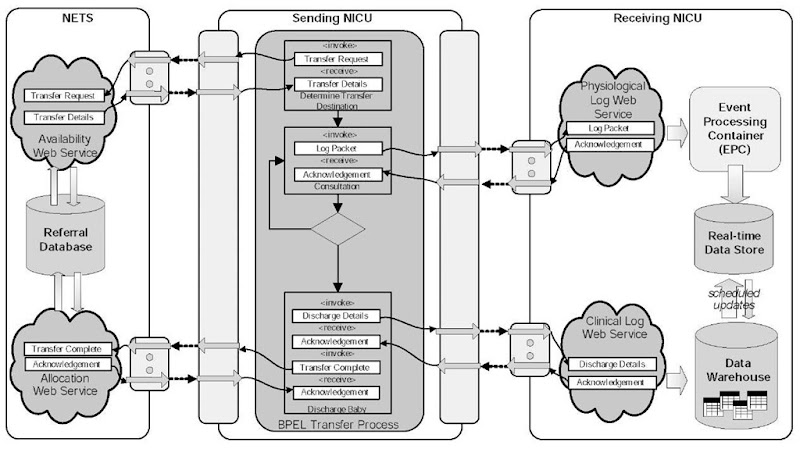
BPEL Design
The BPEL design of the patientjourney as detailed previously are now presented in the following two subsections. The Web services introduced in the previous section are invoked at the appropriate place in the patient journey.
BPEL Transfer Patient Journey—Remote Hospital
The BPEL Transfer Patient Journey from a remote hospital is summarized in Figure 4 highlighting calls to the Availability Web Service, Physiological Web Service, Clinical Web Service and finally the Allocation Web Service.
Figure 4. BPEL Transfer Process—Remote to NICU
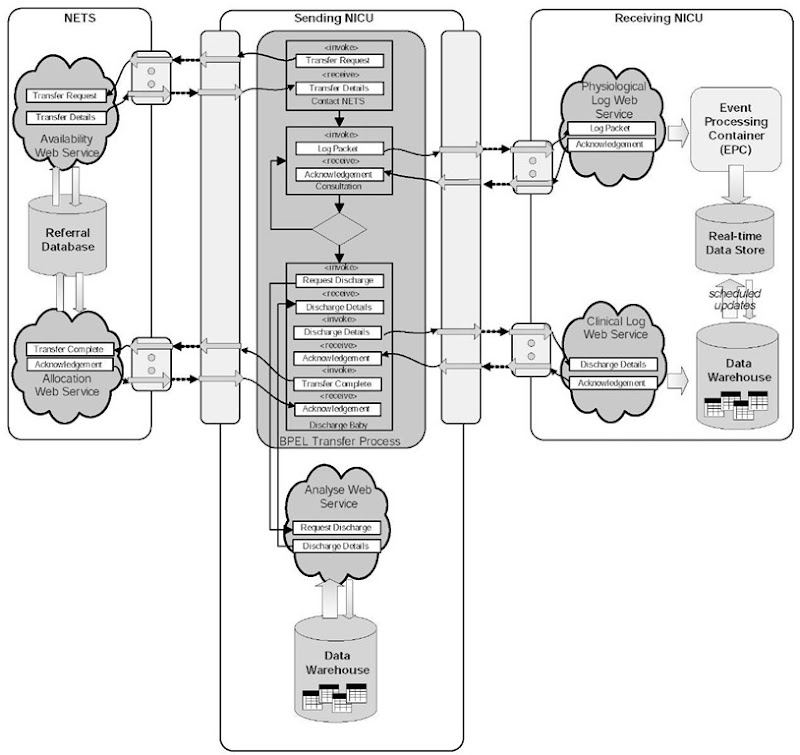
BPEL Transfer Patient Journey—NICU to NICU
The BPEL Transfer Patient Journey between NICUs is summarized in Figures 4 and 5, highlighting calls to the Availability Web Service, Physiological Web Service, Clinical Web Service, and finally the Allocation Web Service. In addition during the Discharge Baby activity a local call to the local Analyse Web Service is made to gather the information to be forwarded via the Clinical Log Web Service.
patient journey prototypes
Several of the Web service components within this research have been or are currently being prototyped within or in association with the Nepean Hospital NICU.
The physiological log Web service and Data Warehouse components of the Solution Manager
Service have been demonstrated via a pilot development using physiological data supplied by a Dragar Ventilator and the Phillips Component Monitoring System (CMS) monitor (McGregor, Heath et al., 2005). Initial testing of compression of XML encoded physiological data streams to improve Web service performance is detailed in (McGregor, Purdy et al., 2005).
The NETS availability Web service and Referral Database has been developed and are currently being prototyped as part of the Bush Babies on Broadband component of the e-Baby collaboration (McGregor, Kneale et al., 2005, 2006).
XML encoding of the discharge summary has been completed and further testing of the generation of this XML coded discharge summary will form part of our future research.
Figure 5. BPEL transfer process—NICU to NICU
conclusion and future work
This article has presented case study based research supporting the development of a framework for the design of Web-service-based Clinical Management systems to support intra- and inter-organizational patient journey workflows. The framework enables the modeling of existing patient journeys and supports the reengineering of these patient journeys to improve communication between clinicians and remove duplication, wasted and excessive activities. Web Services are designed that enable greater support for inter- and intra-organizational transfer of patient data. To facilitate the coordination of the complete inter and intra organizational patient journeys, Business Process Execution Language for Web services (BPEL) is used. A key benefit of this framework is that it enables the establishment of “on demand” patient journeys eliminating the need to establish permanent point to point connections.
This article further describes the application of that architecture to a specific pilot in association with the NICU at Nepean Hospital, Penrith Australia where several of the Web services have been or are currently being tested and trialed. The set of Web services described here have been found to enable mobility, interoperability, alert delivery, and to improve data capture for later research and analysis. While the paradigm shift to using Web services within BPEL processes to support NICUs offers the potential to significantly improve the speed, efficiency, and effectiveness of critical care within NICUs, there are currently several factors impacting its mainstream adoption. These include issues relating to the use of wireless networks in addition to security, privacy, cost, and a lack of standards for physiological data capture and exchange and user interface design. In addition, management issues associated with inter-organization collaboration impact embracing such approaches.
While this research has used cross-functional flowcharts to model the patient journey, research has commenced on an alternate patient journey modeling/communication tool to more richly describe patient journeys (Curry, McGregor, & Tracy, 2006).
Data security and privacy are significant issue s within the healthcare domain. Future research has commenced to incorporate privacy policy information and security models during all phases of this framework.