ABSTRACT
E-health use is increasing worldwide, but no current e-health paradigm fulfills the complete range of user needs for online health services. This dilemma clouds a number of issues surrounding e-health, as promoters of e-commerce, personal health records, and consumer health informatics paradigms attempt to create encompassing e-health within the constraints of each unique perspective. In the long term, the most important of these issues may be the need to develop an e-health pedagogy that offers conceptual grounding and course curricula in order to effectively represent all facets of e-health. To address that issue, this article introduces a personal health informatics (PHI) paradigm that incorporates the best features of preceding paradigms by integrating informatics, personal, and healthcare perspectives. Drawing from PHI, a pedagogical framework is proposed to guide instruction in the design and development of encompassing e-health.
INTRODUCTION
Use of e-health continues to expand worldwide. Harris Interactive reports that the number of Americans who have searched for health information online has increased to 117 million, and 85% of the these individuals searched within the month prior to being surveyed (Krane, 2005). Outside the U.S. and Europe, e-health use has grown more slowly (Holliday & Tam, 2004). However, further expansion seems likely as the World Health Organization and similar groups undertake efforts to increase availability of e-health in developing nations (Kwankam, 2004; WHO, 2005).
While some aspects of successful e-health are well-established, such as the need to provide encyclopedic health content, other aspects are less obvious. For example:
• Which services should be deployed online, and how should users interface with these services?
• If communication is offered, what is the best way to coordinate this to balance the needs of the public with those of healthcare representatives (e.g., physicians and clinic staff)?
• How should personal health records (PHR) be incorporated into e-health, who owns the data in these records, and what (if any) data should PHR share with records of the healthcare provider, insurer(s), and payer(s), such as an employer or a government agency?
These are not idle questions to the health informatics and IT professionals who must design and deploy e-health applications. However, the area of e-health currently is underserved (or not served at all) in health informatics and IT curricula. This is a situation that should be remedied as soon as possible, given the large number of healthcare providers who currently are investing in e-health as an important part of organizational strategy (Lazarus, 2001; Martin, Yen & Tan, 2002).
In developing effective curricula for designers and developers of e-health, I propose that it will be helpful to view e-health from a user-centered perspective that can incorporate best practices of current e-health paradigms without being limited by their constraints. This article presents the foun-dational concepts that underlie this perspective and proposes a new pedagogy.
PARADIGMS OF E-HEALTH
E-health is a broad domain with numerous published definitions that primarily address the convergence of healthcare and Internet technology (Oh, Rizo, Enkin, & Jadad, 2005). A frequently cited definition by Eysenbach (2001) highlights e-health’s interdisciplinary underpinnings.
E-health is an emerging field in the intersection of medical informatics, public health and business, referring to health services and information delivered or enhanced through the Internet and related technologies. In a broader sense, the term characterizes not only a technical development, but also a state-of-mind, a way of thinking, an attitude, and a commitment for networked, global thinking, to improve health care locally, region -ally, and worldwide by using information and communication technology. (Eysenbach, 2001, p. e20)
Historically, each of the paradigms discussed in the following sections has played an important role in developing e-health to its current state. Yet, I will argue that none of these paradigms fulfills the complete range of user needs for online health services, and for this reason, none presents a suitable basis for pedagogy in design and development of encompassing e-health.
E-Commerce Paradigm
Prominent early developers of e-health services operated within an e-commerce paradigm in which vendors expected to profit from users paying directly for products and services acquired through the site or from advertisers paying for exposure to users. Typically, vendors were not affiliated with healthcare providers, so they could not provide services that link individuals with their own physician, clinic, or pharmacy. Although numerous vendors developed e-health within the e-commerce paradigm, few survived the ensuing shakeout due to failure to provide value to customers or to adequately control costs, lack of effective revenue models, or simple inability to ensure sustainable competitive advantage (Itagaki, Berlin, & Schatz, 2002; Rovenpor, 2003). Among the prominent e-health ventures representing the e-commerce paradigm, such as DrKoop.com, MediConsult.com, and PlanetRx. com, only a handful remains. The best-known of these is WebMD, which provides an exceptionally wide range of health services but continues to struggle toward profitability.
Personal Health Record Paradigm
A second approach to e-health that initially was based on profit motives is the personal health record (PHR) paradigm. The PHR is defined as follows:
An electronic, universally available, lifelong resource of health information needed by individuals to make health decisions. Individuals own and manage the information in the PHR, which comes from healthcare providers and the individual. The PHR is maintained in a secure and private environment, with the individual determining rights of access. The PHR is separate from and does not replace the legal record of any provider. (AHIMA, 2005, p. 64A)
The idea of computerizing personal health information is not new. A number of vendors introduced PHR products during the 1990s, both as stand-alone software and as online services. To date, demand for commercial PHR products has been low—only 2% of individuals who maintain health records use purchased PHR software (Taylor, 2004) —and none of these products has gained financial success (Holt, 2005). However, several factors may prompt increased use of PHRs in the near term. First, the U.S. public gained increased awareness of the value of portable health records as a result of the massive human displacement and damage to healthcare facilities sustained from hurricanes during 2005. This awareness is likely to affect public sentiment and governmental policies for some time to come (Kloss, 2005). Second, PHR software is continuing to improve. Current offerings have become easier to use and are more fully capable of integrating health resources beyond the individual’s immediate data, such as linking to relevant medical journals and FDA drug information (Campbell, 2005). Finally, researchers are beginning to study how individuals go about maintaining health records in non-computerized settings, and this research is clarifying the opportunities and constraints that PHR developers face. For example, two recent studies in this area assess the importance of privacy and security in health records (Taylor, 2004) and shed light on the diverse strategies that individuals prefer to employ in storing health records (Moen & Brennan, 2005).
consumer Health Informatics Paradigm
Although healthcare providers did not participate strongly in early stages of e-health development (Lazarus, 2001), these organizations have been instrumental in developing an increasing amount of e-health within a consumer health informatics (CHI) paradigm. CHI is “a branch of medical informatics that analyzes consumers’ needs for information; studies and implements methods for making information accessible to consumers; and models and integrates consumers’ preferences into medical information systems” (Eysenbach, 2000, p. 1713). Where e-commerce vendors hoped to achieve competitive advantage, healthcare provider organizations appear to be driven more by concerns of achieving competitive equity, both with competing providers and commercial e-health sites. Because CHI is produced by healthcare provider organizations, e-health produced within this paradigm has been oriented toward providing added customer service, increasing healthcare delivery quality, and containing costs rather than selling products, services, or advertising access. Although the CHI paradigm is designed to address needs of the individual user, it inherently takes an organizational perspective that imposes a passive view of users as consumers rather than suppliers of information. Thus, providing PHRs and integrating external patient data typically have not been high priorities for e-health created within the CHI paradigm.
A New Paradigm: Personal Health Informatics
Each of the three historical paradigms identifies an area of need in the population of e-health users. However, none addresses the total range of needs that e-health users identify. These include communicating with physicians and clinic staff, arranging services (e.g., scheduling appointments and renewing prescriptions), checking bills and making payments, viewing lab results, accessing records of procedures/tests/immunizations, receiving online alerts, monitoring chronic conditions, and interacting with online support communities (e.g., patient chat groups), in addition to accessing encyclopedic health information (Fox, 2005; Harris, 2000; Taylor & Leitman, 2002). Furthermore, individuals want the ability to control their personal data, to ensure that recordkeeping aspects of e-health are interoperable and portable, and to be assured of privacy and security (Holt, 2005; Taylor, 2004). In order to capture the complete set of knowledge and skills that will be necessary to encompass e-health services, I propose that it is essential to consider a new paradigm that can integrate best practices of the three paradigms discussed previously. Because of its user-centered focus, which views e-health from the perspective of individual users in the role of information provider as well as information consumer, I term this paradigm personal health informatics (PHI). PHI is defined as the knowledge, skills, practices, and research perspectives necessary to develop e-health that is effective, efficient, encompassing, and user-centered.
FOUNDATIONS OF A PHI PEDAGOGY
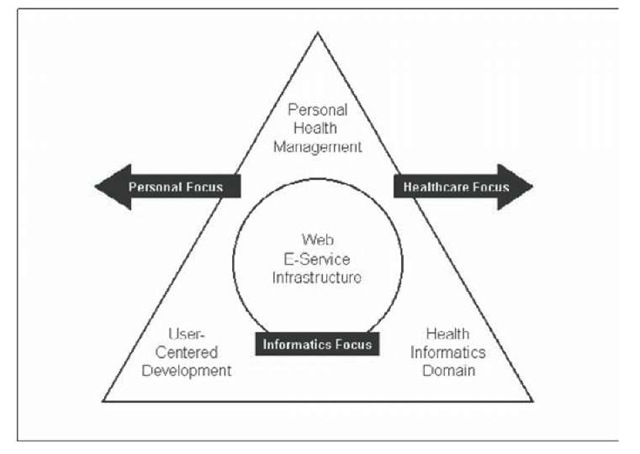
A conceptual model of PHI is presented in Figure 1. Four structural components define the content of PHI within three focal areas. Web e-service infrastructure is the hardware, software, and networking capabilities that support all e-health functions. Because e-health is primarily service-oriented, the informatics focus in PHI centers on infrastructure that is specialized for e-ser-vice presentation and delivery. Personal health management and user-centered development comprise the personal focus that PHI presents to individual users. User-centered development methods provide tools for eliciting user needs, designing solutions, and evaluating the utility of these solutions in meeting user needs. Personal health management addresses individual practices as well as psychological, social, and cultural aspects of the management, storage, and retrieval of personal health information. Personal health management and the health informatics domain combine in the healthcare focus of PHI. Content within the health informatics domain addresses the skills, knowledge, and surrounding use of IT within the subject health area(s).
In order for students to enter the health informatics and IT workforce with sufficient preparation to develop e-health that can fully support individual users’ needs, training will be needed in each of the structural areas of PHI, which are presented in Figure 1. None of these areas is beyond the grasp of graduate or advanced undergraduate students; however, the combination of content areas represents a set of specializations that rarely are combined in current curricula. Thus, for the time being, PHI training necessarily will have to be pieced together from existing textbooks, research reports, and industry cases. I address each curricular area in the following sections.
E-service Web Infrastructure curriculum
E-health in the PHI paradigm is essentially a form of e-service, defined as services provided over electronic networks such as the Internet (Rust & Lemon, 2001) Thus, most texts that focus on development and administration of Web infrastructure for e-services will be applicable to PHI. Texts that address the general topic of e-commerce typically are less applicable, as large portions of these dwell on factors that are not central to e-health, such as general business models, marketing and consumer behavior issues, and methods for increasing online sales. Web infrastructure changes rapidly, so texts in this area must not be allowed to become stale. New texts should be chosen, based upon inclusion of emerging technologies such as mobile devices, speech recognition, and natural language parsers, as well as effective coverage of more mature technologies such as XHTML, database connectivity, and network communications.
User-centered Development curriculum
User-centered development refers to a software development process that incorporates the user viewpoint, assesses user needs, and validates that user needs are met. There are two complementary approaches to this process that will be valuable to students of PHI. The first of these is the de sign guide approach. Design guides emphasize generic or context-specific design principles, such as the following example for use of color on Web sites:
In the physical world, color has embedded meaning, usually culturally based. In the American culture, at a simplistic level, red means stop and green means go, red means hot and blue means cold, black means death and white means birth, and green represents money and greed. These embedded meanings of color differ from culture to culture; for instance, the color white is symbolic not of birth, but of a funeral in Japan or India. (Lazar, 2001, p. 158)
Design guides are valuable in establishing general guidelines in conventional use of design features and in broadening students’ appreciation of ways that others’ perspectives may differ from their own.
The second approach emphasizes the design process by establishing an algorithmic approach or how-to guidance for developing functionality and user interface features. For example, the SALVO method (Wilson & Connolly, 2000) guides students through five development stages. The first three of these are planning stages in which designers specify user needs, adopt a technology-specific design guide, and leverage appropriate matches between technology and user needs in order to enhance user abilities and to support user disabilities. Once planning stages are initially completed, developers perform visualization techniques, including mockups to elicit user feedback early in the development cycle. Visualization is followed by an observation stage, in which designers observe and evaluate attempts by users to perform representative tasks using the mockup or completed software. SALVO takes an iterative approach to development, and it is accepted throughout the development cycle that prior stages and sequences of stages can be repeated, as necessary. The design process approach provides PHI students with a methodology and specific tools for customizing e-health in order to meet the needs of a specific user audience, which may differ substantially, for example, between a macular degeneration support group and the general public.
Figure 1. Conceptual model of key PHI structural components
Personal Health Management curriculum
Personal health management is an emerging area of research, and new findings likely will emerge that add appreciably to current knowledge in this field. Although it may be too early to look for texts that focus on personal health management and good empirical studies, and cases are available that would be highly applicable to PHI. One exemplar is a study by Moen and Brennan (2005) that investigates strategies for health information management (HIM) that are applied by individuals in their own homes. Their research identifies four HIM strategies:
• Just in Time. Information is kept with the person at most times in anticipation of immediate need.
• Just at Hand. Information is stored in familiar, highly accessible locations, often serving as a reminder.
• Just in Case. Information is stored in order to be accessible in case of need, but out of view.
• Just Because. Information is retained in interim storage pending a decision to file or to discard it.
This study presents several important implications for developers of HIM software that would be highly relevant for PHI students to consider and discuss. These include effects of tradeoffs between information accessibility and visibility on the success of individuals’ efforts to coordinate HIM, implications of the high degree of reliance that individuals place on paper-based records, and design decisions that would be necessary in order to align electronic records to support the differentiated storage strategies that individuals are found to prefer.
Health Informatics Domain curriculum
The health informatics domain encompasses use of IT to support the delivery of healthcare services (including communication, coordination, logistics, and other business processes) as well as applicable practices and procedures that surround the use of IT in the healthcare setting. It is important to recognize that while the health informatics domain is a key component of PHI, it is not the central element of e-health from the user’s perspective. In order to preserve a user-centered focus, it is essential that distinctive components of PHI pedagogy should not be replaced by health informatics courses that focus on IT from a perspective that is internal to the organization (i.e., managerial or technical). Where PHI is taught within an existing health informatics program, a range of courses already will be in place in order to effectively cover topics in the domain. Where PHI is taught in technology programs, topics in the health informatics domain may be covered effectively by traditional health informatics or by medical informatics texts.
suggested Modes of curriculum Organization
As discussed previously, PHI can be integrated into the undergraduate or graduate curricula of existing health informatics programs or used to augment offerings in technology programs, such as information systems, computer science, or information science. As a specialization within a health informatics program that already incorporates domain coverage, in-depth PHI training can be achieved by a curriculum that offers one course-equivalent each in user-centered development and personal health management and up to two courses in Web e-service infrastructure. If two courses are offered, the first should focus on basic development methods, including XHTML, XML, and simple database connectivity, and the second on administration issues and advanced development methods including Web services, mobile applications, and emerging technologies.
As an augmentation to a technology program that already incorporates Web e-service infrastructure coverage, substantial depth of PHI training can be achieved by offering a specialization with one course equivalent in each of user-centered development, personal health management, and health informatics. A final alternative is to offer a basic introduction to each of these subjects within a single course equivalent. Although not ideal for career preparation, this alternative could be an effective way to direct technology-area undergraduates toward careers and further educational opportunities in the field of health informatics and IT.
conclusion
Although not always profitable for commercial vendors, e-health has been a success for individual users. Major healthcare provider organizations have adopted e-health as a means of attaining competitive equity in the marketplace, thus providing greater opportunities for individuals to use e-health and creating a demand for trained health informatics and IT professionals to work in e-health. PHI presents a conceptual perspective that incorporates the best features of preceding paradigms and provides a framework for improving instruction in e-health design, development, and administration.