Experimental development of bioactive titanium in forms by LASAK
The LASAK Company developed bioactive titanium with original surface modification at the end of the 1990s. Due to the limitations of the glass-ceramic implant mentioned above, we have been developing a new type of implant combining bioactive properties and higher mechanical resistance in cooperation with LASAK Company since 1998. Characteristics of this material (higher strength, bioactivity) have provided optimal implant characteristics for PLIF (Yan, 1997; Strnad, 2010). The material used for this implant is technically pure titanium (grade 3) which is dedicated for surgical implants (Regulation ISO 5832-2:1993(E): Implants for surgery, ISO 5835-2). To ensure bioactivity of this material, the implant surface is chemically modified by LASAK technology (Adjudication on Permission to Use a Medical Device No. 82/125/00-IIB by State Institute for Drugs Control of the Ministry of Health of the Czech Republic). Mechanical properties of this material are identical to pure titanium, and its strength and fracture persistence are several times better than characteristics of the bone tissue and the glass-ceramic material (see Table 3).
|
|
Titanium |
Bone |
Glass-ceramic |
|
Compressive strength (MPa) |
|
100-230 |
1080 |
|
Tensile strength, flexural strength* (MPa) |
240-680 |
200* |
170-218* |
|
Elasticity modulus (GPa) |
100-120 |
25 |
220 |
|
Fracture persistence (MPa-m-1/2) |
~40-100 |
2-12 |
2 |
Table 3. Comparison of mechanical properties of titanium, bone and glass-ceramic BAS-0.
The mechanically and chemically modified surface of the bioactive titanium by LASAK technology is able to induce the production of calcium-phosphate (apatite), and this compound arises from the interaction between the surface of the material and body fluid within hours to days. The chemical and crystallographical properties of this mineral are nearly identical with the bone apatite. Experimental studies with bioactive and bioinert titanium demonstrated that titanium with a bioactive surface better tolerates unfavourable conditions for osseointegration, as gaps between the implant and the bone (Strnad et al, 2003). Bioinert titanium allows penetration of fibrous tissue into the interface implant/bone, and promotes instability or migration of implants towards the spinal canal in conditions requiring spondylosurgery. However, a firm interaction between the calcium-phosphate layer of the implant and the surrounding bone forms immediately after application if bioactive titanium with technological modification according to LASAK is used, which ultimately eliminates this risk.
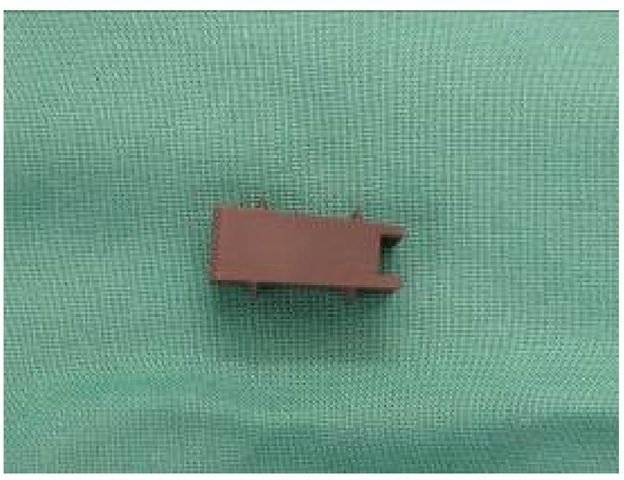
Strength parameters and bioactivity would be expected to improve conditions for osseointegration in the intervertebral space, as compared to implants generated from bioinert materials and glass-ceramic. Therefore, this type of material appears to be optimal for the development of a new implant for PLIF. Based on our experiences with the glass-ceramic BAS-O, we designed a new implant model constructed from this material. Due to different properties of these two materials (glass-ceramic/biotitanium), we modified the shape of the implant, and we designed new application instrumentation. The basic model was the shape of skewed prism (4o) (20 mm long, 8 mm wide, with graduated high 6, 8 and 10 mm). The implant was equipped with two pairs of projections or winglets (2 mm high) on the opposite sides of the prism. The compression and bending load of our original model for PLIF was virtually mathematically tested using computer technology in cooperation with CVUT Prague. These tests showed that the shape of the skewed prism with winglets can theoretically ensure the restoration of the anatomy of the operated segment of lumbar spine without a risk of a plunge into the adjacent vertebral bodies both during compression and flexion and without a risk of its damage (Figure 6).
Based on these mathematical analyses, we maintained the basic shape of the implant with the above mentioned parameters. The higher strength of the material allowed us to design simplified application instrumentation. We used a thread in the implant body instead of the Teflon-coated fork used in the implant BAS-O. Due to its strength, no opposite space dilatation was necessary before the application as a result of the bioactive titanium implant, and no risk of damage of the implant shape by metal loaders was detected. Therefore, the handling of the implant during an intervention is easy and safe. The shape of the implant ensured good restoration of the anatomy of the operated area (restoration of the interbody space and its stability) with minimal risk of implant plunge into the adjacent vertebral bodies, as demonstrated by imaging investigations. Other benefits of the new implant included higher strength and shape variability.
Fig. 6. Illustration of the mathematical testing of the implant model.
Fig. 7. Implaspin in the intersomatic space of a cadaver by CT (2001).
We removed the whole motion segment with implants from cadavers after experimental operations, and we assessed their localization and the degree of their damage by X-ray and CT scans (Filip et al, 2001). Both investigations showed proper localization of the implants in the intervertebral spaces without any contact with the spinal canal or perforation of the winglets into the adjacent vertebral bodies (figure 7).
Additionally, their shape and surface were not damaged by the new type of instrumentation. Therefore, we assumed that these findings would transfer from experimental studies into clinical practice. However, we were not able to verify the osseoconductive properties of the implant surface in the cadavers. A perfect contact was observed between the surrounding bone tissue resulting from the simple application in cadavers, which was a good precondition for supporting osseointegration in the interbody space via osteoblasts’ migration along its surface. Thus, we verified the osseoconductive properties of the BIO surface of the implant in an animal model (Strnad, 2008). The implant surface in the direct contact with newly produced bone tissue yielded the following values [BIC (%) = 48,5 ± 2,9, 66,0 ± 7,4 and 90,6± 7,0, respectively, two, five and twelve weeks after implantation].
Fig. 8. Histological section of the interface of newly formed bone tissue on the BIO surface of the titanium implant twelve weeks after implantation. This figure illustrates the osseoconductive properties of the surface (optical microscope, toluidine blue staining, original magnification – 200x).
Implaspin in clinical practice
Encouraged by these experimental results, we began to use this type of implant in clinical practice in indications for PLIF instead of the glass-ceramic implant since 2002 (Figure 9).
The operation technique PLIF was identical to the operation technique used in cadavers (Filip et al, 2010). For example, we decompressed the nervous structures through posterior median line approach, and we then radically removed the degenerated intervertebral disc under the control of the operation microscope. Afterwards, we removed the surfaces of the adjacent vertebral bodies, and we then inserted the bioactive titanium implant using the innovated instrumentation (Figure 10). Finally, we added transpedicular fixation of the whole segment (Synthes, Signus, Easy spine, etc.) (Figure 11).
Fig. 9. Implant from bioactive titanium – Implaspin (2002).
Fig. 10. Insertion of Implaspin into the interbody space.
Fig. 11. Transpedicular application of screws (SIGNUS)
To date, we have not observed any complications associated with the implant application into the interbody space. According to the postoperative scans, the implant was always placed in the correct position with winglet penetration into the spongious tissue of the adjacent vertebral bodies. We have selected the size empirically according to the extent of osteochondrosis of the affected disc and the degenerative lesions of the surrounding tissues on scans (X-ray, CT, MRI) during the intervention. In the majority of cases, we used implants (8 or 10 mm high) with angle 4% to maintain lordosis in the lumbar area (Figure 12).
Fig. 12. Fixation L4/5 (Implaspin plus transpedicular screws Signus).
According to the experimental studies, tight contact with the surrounding bone tissue was necessary to activate the bioactivity of the surface. This contact was ensured by the shape of the implant and the winglets that penetrated into the spongious bone tissue of the adjacent vertebral bodies, and was the precondition for migration of the osteoblasts along the implant body resulting in the formation of a junction of the adjacent vertebral bodies by bone tissue without the need to sample bone grafts or to add supporting synthetic materials inside or around the implants.
In 2002 to 2007, operations were performed on 57 patients using the bioactive implant Implaspin in the Neurosurgery Clinic of the Faculty Hospital in Ostrava and in the Neurosurgery Department of Tomas Bat’a's Regional Hospital in Zlin. We assessed a population of 25 patients with follow-up examinations conducted two or more years following surgery, according to the clinical condition. The follow-ups were also based on the generally used score system ODI and imaging methods (X-ray, CT, MRI) that occurred three, six, twelve and 24 months after surgery. During the follow-ups, we examined the patients for signs of implant damage, instability of the operated segment, and signs of supposed osteoblastic activity of the bioactive surface of the implant on the scans. Results of the ODI questionnaire showed that with Implaspin, our success rate improved by 1 degree (59%-40%), or we stabilized the clinical condition of the majority of the patients long-term (2 and more years), which corresponds to results of other clinics using other implant types (Bessho et al, 1997; Brantigan et al 1993; Brayan et al, 2002; Bienik and Swiecki, 1991; Ciappetta et al, 1997; see Table 4).
|
ODI score in our population [%] |
Mean [n] 25 |
FBSS [n] 9 |
IS [n] 6 |
DI [n] 10 |
|
Before surgery |
59 |
65 |
55 |
57 |
|
3 months after surgery |
42 |
46 |
40 |
40 |
|
6 months after surgery |
40 |
45 |
37 |
38 |
|
12 months after surgery |
41 |
45 |
39 |
39 |
|
24 months after surgery |
40 |
47 |
35 |
38 |
Table 4. Mean Oswestry score values before surgery and at regular visits (FBSS – failed back surgery syndrome; IS – isthmic spondylolisthesis; DI – degenerative instability).
The assessment of the implant position on scans (X-ray, CT, MRI) at postoperative visits demonstrated no signs of implant damage or implant migration out of the intersomatic space. These investigations have not yet shown any signs of instability of the operated segment (i.e., formation of new osteophytes, progression of hypertrophy of the articular facets, and migration of the implant at the site of application). We observed one severe complication in the population which was caused by an inaccurate application of the transpedicular screws. The wound healed in this patient, and the neurological findings stabilized after removal of the screws. The stabilization of the condition may be supported by the implant shape and the winglets which prevented instability even after the removal of the transpedicular screws. This finding was confirmed by the imaging investigations. Based on the clinical condition and the absence of instability signs on imaging investigations, we concluded that the formation of bone fusion was due to osteopblasts’ migration along the bioactive of Implaspin surface.