Introduction
Without question, the treatment of atypical facial pain can only be addressed by defining the term. It means different things to different people. Under this heading there are: atypical facial neuralgia; pain from damage to the trigeminal nerve, often from trauma, dental, and ear, nose, and throat (ENT) procedures; trigeminal neuropathy; atypical trigeminal neuralgia; anesthesia dolorosa; as well as a host of other ill-defined face pain problems. In general, it is prudent to think long and hard before making permanent sensory deficits (lesions proximal to the gasserian ganglion) in this group of patients. whose problem may be difficult to define or understand.
"Atypical facial neuralgia,” or "facial pain not fulfilling criteria of previously described groups,” as described in the International Headache Society classification, to most is a pain that is psychogenically determined. The pain may be considered to be a "somatization disorder,” a "conversion disorder,” the result of "hypochondriasis," or a "body dysmorphic disorder.” [1] The pain is usually constant ("I’ve had this pain day and night for 3 years”), often bizarrely described, migrates, and has a predilection for women. It radiates beyond the trigeminal distribution, is frequently associated with depression, and the underlying psychopathology is often obvious. The Minnesota Multiphasic Personality Inventory (MMPI) is often strikingly abnormal in these patients and no surgical intervention is indicated. My approach to this problem is to sympathetically inform the patient that as a surgeon I can do nothing to help them and to guide them, when possible, to psychotherapeutic workers. If they are not already on narcotics or have had no surgery, it is important to counsel and warn them of: (1) the frequency and hazards of drug addiction, and (2) the often unnecessary surgery that well-meaning but misguided clinicians may recommend.
Trigeminal neuralgia is a classic and stereotyped clinical entity and usually easily diagnosed, but there are occasions when certain atypical features creep into the picture, raising the question of whether one is dealing with true trigeminal neuralgia. If true trigeminal neuralgia is not the underlying problem, creating permanent sensory deficit in the face may make the matter worse, because the pain is not relieved and now the patient has an unwanted numb face. In this case, peripheral radiofrequency (RF) blocks may be helpful in clearing the air [2]. If it is not true tic, the sensory deficit will fade in months to a year—or more if a dense block is obtained, and no bridges have been burned. It is important to inform the patient that the sensory deficit from these extracranial blocks is usually more dense than that obtained from retrogasserian RF blocks and that he or she will most likely be happier with the central lesions should that be the ultimate approach.
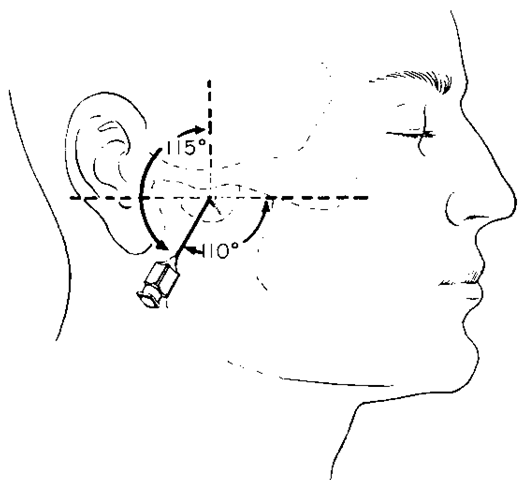
The third division can be blocked by the subzygomatic approach, reaching the mandibular nerve as it exits from the foramen ovale. It is better to block the mandibular nerve with radiofrequency than with alcohol because of the reported spread of the alcohol up into the ganglion and cerebrospinal fluid with sometimes disastrous results. Furthermore, the use of a small cordotomy-type electrode, which is bent at its tip, facilitates the localization of the nerve by directing and redirecting the electrode to the lowest threshold for stimulation. When the electrode is on the nerve, the stimulation threshold is usually around 0.1 volt. A thin-walled 18-gauge lumbar puncture (LP) needle is used with a marker set on the needle at 5 cm. The landmark for needle introduction under local anesthesia is a point 2 cm anterior to the ear canal with the needle oriented below the zygoma perpendicular to the skull in the anteroposterior dimension and angled 115 degrees superiorly (Fig. 1). The LP needle usually slides across the base of the middle fossa impinging on the mandibular nerve at a depth of 5 cm. When the electrode is on the nerve, the patient is put to sleep with 35 to 40 mg of methohexital (Brevital). A maximal lesion is made, the current gradually raised until boiling occurs as evidenced by a sudden drop in the voltage reading. If the nerve is not readily reached, a submento-vertex radiograph may help in orientation by revealing the foramen ovale. Remember that the search is in an anteropos-terior direction with the nerve passing straight inferiorly at this point.
Figure 1 The needle orientation for a subzygomatic block of the mandibular nerve at the foramen ovale.
The maxillary nerve usually has to be blocked more centrally in the pterygomaxillary fissure. The approach here is to place the marker on the LP needle at 6 cm and introduce the needle beneath the zygoma 3 cm anterior to the ear canal. The orientation is 110 degrees anteriorly and 115 degrees superiorly (Fig. 2). The needle usually strikes the pterygoid plate at about 5 cm. It is then walked anteriorly until it falls into the fissure. The maxillary nerve is usually right there. In a small percentage of patients, anatomical variation prevents the maxillary nerve from being reached by this approach. Remember that the search here is in a superior-inferior direction, as the nerve is passing horizontally in the fissure. A lesion is made, as described above.
A frequent atypical face pain problem seen by the neurosurgeon is the pain resulting from an injury to the trigeminal nerve, whether it is from trauma, sinus disease, or surgical procedures on the face. Some refer to this as ”trigeminal neuropathic pain” [3].
Figure 2 The needle orientation for a subzygomatic block of the maxillary nerve in the pterygomaxillary fissure.
This pain is localized to this nerve, most often in the second division and is the result of injury to the nerve peripherally. There may be no overt sensory loss and usually there is no relief from anticonvulsants such as carbamazepine. This injury may, in time, lead to the development of central self-generating and self-perpetuating neu-ronal discharges that are perceived as chronic face pain [4]. That this central mechanism may be at play is supported by the observation that destructive lesions proximal to more peripheral lesions, which could be reasoned to interrupt afferent discharges, are often ineffective in relieving the pain. Therefore, although extracranial RF blocks, as described above, can easily be performed, they should only be attempted if the neurosurgeon sees the patient early after the onset of the pain and before central mechanisms become established. Unfortunately, this is rarely the case and the neurosurgeon more often first sees the patient many months or years after the onset. Thorough informed consent is necessary if RF blocks are to be used in these patients. An alternative and nondestructive approach to be considered in these patients is the use of chronic electrical stimulation of the gasserian ganglion by the percutaneous insertion of electrodes by way of the foramen ovale. Approximately 50% of patients so treated obtain good relief with acceptable complications. Several reports outlining the results and technique are available [5-7].
The stereotaxic approach to the nucleus caudalis has been used to treat with RF various atypical face pain problems [8]. This is a complicated technique not used by many at this time and the complications of ataxia and severe dysesthesias have dissuaded many from its general use. Similarly, RF mesencephalic tractotomy should be reserved for those familiar with the technique and aware of the significant complications: oculomotor dysfunction and 5% mortality. These techniques are best for those with chronic face pain from cancer, not for the ”garden variety” of atypical face pain. The same can be said regarding the use of RF thalamotomy, which has primarily been used to treat post-herpetic neuralgia and anesthesia dolorosa, often with inconsistent results.
Akin to trigeminal neuropathic pain is the pain limited to areas of the trigeminal nerve that is unrelated to peripheral injury. It is of unknown origin and spontaneous in onset. This is a most difficult area to understand or treat, and the best advice would be to avoid any RF destructive procedures.
A difficult and atypical pain problem refractory to analgesic medication is chronic ocular pain, usually secondary to glaucoma, penetrating injury, or previous retinal detachment surgery. Radiofrequency lesions to the retrogas-serian first-division fibers were successful in immediately and completely relieving this pain in all nine patients [9].
To treat these patients, the retrogasserian rootlets are approached by the previously described techniques for RF thermocoagulation [2,10,11]. Using this approach, graded incremental lesions in the first division can be made by treating the first division fibers while the patient is awake. It is important to appreciate that RF lesions in the first division are often associated with little, or sometimes no discomfort, facilitating treatment in the awake patient but, at the same time, providing no clue to the surgeon that he is indeed making a lesion. Corneal sensation can be lost if the awake patient is not constantly monitored while the lesion is being made. The lesioning is accomplished by making multiple incremental thermocoagula-tions of increasing voltage (and milliamperage) while constantly observing the eyelash blink reflex. This reflex is tested by flicking the eyelash with the twisted corner of a single layer of facial tissue. As the lesion creeps into the first division, there is first a diminution of the consensual blink followed by a decrease in the direct blink. With this technique, the lesioning can then be stopped when there is some loss of corneal sensation but with preservation of the corneal reflex. It would appear that this treatment for this clinical entity is largely unknown and underutilized.
Although not properly an atypical facial pain, chronic migrainous neuralgia, a form of cluster headache, can be intractable and unresponsive to medical therapy. These patients may be desperate for relief. The pain is usually centered and most severe in the region of the eye. Radiofrequency thermocoagulation has been used to treat patients with this syndrome. The results were excellent in eight patients in a University of Minnesota series [12]. Seven of these eight patients had an analgesic or hypalgesic cornea. In a Mayo Clinic series, the results were excellent in 11 and good in two of 24 patients in who analgesia of the first division was obtained [13]. The results were poor in seven patients in whom little sensory deficit was obtained in V1, and two patients with 75% loss of sensation had a poor result. In a third series of 27 patients with this disorder, RF retrogasserian rhizolysis produced excellent results in 15 patients, very good in 2, good in 3, fair in 1, and poor in 6 [14]. The complications were mild and transient and the benefits of surgery far outweighed the discomfort from the complications. Thus, if sensory deficit in the first division can be obtained, RF treatment of this difficult entity may offer lasting relief. This treatment is also probably underutilized.
It is important to appreciate that an anesthetic cornea only rarely leads to serious complications, keratitis in particular. A review of 100 patients with anesthetic corneas as the result of alcohol injections into the trigeminal sensory root found that only five patients became blind [15]. One of these patients was ”mentally not normal,” one was an alcoholic, one had preexisting corneal scarring, and one was ”a rather simple man” who did not seek early treatment. The fear of blindness from keratitis would seem to be somewhat overrated and should not deter the patient or surgeon from pursuing RF treatment when indicated. Early treatment of keratitis is most important.
In summary, the use of destructive RF thermocoagulations to treat atypical facial pain is limited and the surgeon must prudently and cautiously heed the advice of those with experience in this area and suppress the compulsion to pursue a seemingly sound, but misguided, course of treatment.