Electrodes
For a surface ECG, the electricity must pass from the heart and up through the skin in order for the ECG to detect the current. The stratum corneum, the outermost layer of the skin, does not conduct electricity well because it contains dead and dried out cells. These dead cells cause the skin to act as a resistor; resistance to the passage of electricity.7 To permit the passage of the electrical current through the skin to the surface, the electrode must have an intermediate substance, a conductive medium which bridges the stratum corneum and connects the inside of the body with the electrode.
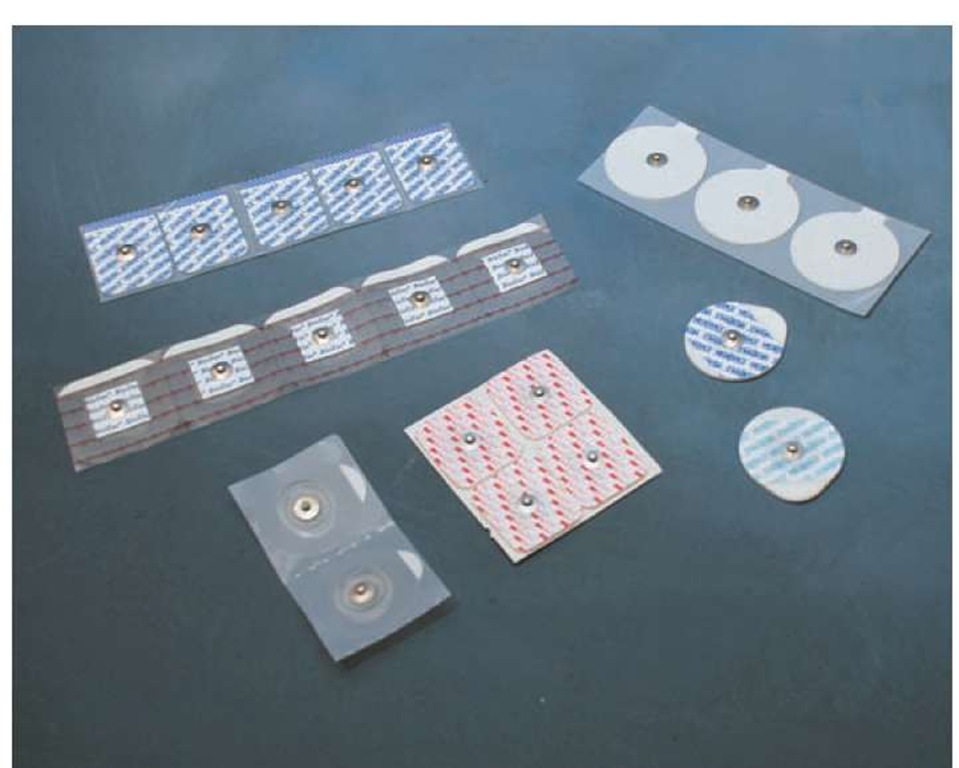
Typically an ECG electrode is used for that purpose. An electrode consists of a gel-like substance that conducts electricity well, such as silver chloride, with an adhesive on a foam or paper backing to help maintain contact (Figure 33-4). The conductive gel is designed to melt with body warmth and soak through the skin. This will enable it to overcome skin resistance to the electrical signal and create an electrical bridge from the inside of the body to the electrode. A sticky piece of foam or paper surrounds the gel. This serves to isolate the electrode from the surrounding environment and enables the electrode to adhere closely to the skin.
Warmth is necessary for the electrode to function. Without warmth the conductive gel does not melt, the electrical pathway is ineffective, and the signal quality will be poor or lost entirely. When the gel only partially melts, due to cold skin or poor adherence of the electrode, then the quality of signal will also be poor (degraded) and the tracing will be unreadable (noisy).
There are many reasons why an electrode will not function. If the gel on the electrode has dried, it will no longer serve as an electrical pathway. Electrodes should be inspected regularly to ensure new and moist electrodes.
Figure 33-4 Examples of ECG electrodes.
Figure 33-5 Electrode position affects the electrical view of the heart.
Electrode Placement
The primary objective of monitoring the electrical activity of a patient’s heart is to discern abnormalities of conduction or automaticity that produce potentially life-threatening dys-rhythmias. An ECG lead is a view of the heart from one particular vantage point that helps to ascertain the dysrhythmia (Figure 33-5). For example, Lead II (a commonly used monitoring lead) views the inferior portion of the heart and would help identify dysrhythmia arising from the inferior wall. Most dysrhythmias can be ascertained using one or two leads. It is important for the Paramedic to choose the lead that provides the best chance of identifying the dysrhythmia.
For Lead II, one electrode is placed on the right wrist, one electrode on the left wrist, and one electrode on the left foot (to recreate Einthoven’s Triangle) (Figure 33-6). In many cases, it is inconvenient to place the electrodes out onto the limbs where the wires may become tangled. Therefore, the Paramedic may choose to place electrodes on the right and left upper arms at the deltoids. Lower electrodes are then placed on the right and left thighs. The third alternative strategy, suggested by Takuma and associates, is to place the electrodes in the subclavicular space (the deltopectoral fossae) on the right and left and then on the right and left lower rib cage.8 The important concept is to try to maintain Einthoven’s Triangle.
STREET SMART
Many Paramedics use the same electrodes for the monitoring ECG as for a 12-lead ECG. Key to an accurate 12-lead ECG is the re-creation of Einthoven’s Triangle. Jowett and associates suggested that placing the limb leads on the torso can lead to inaccurate interpretation of the 12-lead by producing false patterns of ischemia.9
Figure 33-6 Electrode placement for limb leads.
Best results are obtained from placing the electrode over muscle and not over bony prominences. The Paramedic should also avoid placing an electrode over any jewelry, implanted devices such as pacemakers (automated internal defibrillator/ cardioverters), or medication patches.
To ensure patient comfort, connect or clip the wires to the electrodes before attaching the electrodes to the skin. Pressing the snap connection to an electrode that is already on the skin is uncomfortable for the patient. Perhaps more importantly, it squeezes the gel out from under the electrode, potentially causing loss of signal.
Standard Lead II Configuration
If the negative lead is on the right shoulder and the positive lead is on the left leg, then the ECG machine is monitoring Lead II. Lead II provides a view of the inferior wall of the heart.10-12 The upper portion of the conduction system resides within the inferior wall, from the SA node to the AV node. This portion of the left ventricle also receives its blood supply from the right coronary artery.
Whenever there is suspicion of an acute occlusion of the right coronary artery, and therefore doubt about performance of the upper portion of the conduction system (a conduction abnormality as manifest by changes in the PR interval), then the patient should be observed in Lead II. Because Lead II provides an excellent view of the inferior wall/upper portion of the conduction system, it produces the clearest P waves.
Modified Chest Lead
While it may be easier to distinguish P waves in Lead II, the placement of the electrodes may be more difficult in the field. Also, the electrodes in Lead II may interfere with important procedures such as defibrillation. For these and other reasons, many Paramedics choose modified chest Lead 1 (MCL1) to monitor patients instead of/in addition to Lead II (Figure 33-7). MCL1 simulates the precordial lead V1, one of the six precordial leads of a 12-lead.
Figure 33-7 Lead placement for MCL1.
By placing the positive monitoring electrode at the right sternal border at the fourth intercostal space, between the fourth and fifth ribs, and looking across the chest from the left shoulder, the Paramedic obtains a view of the anterior wall of the left ventricle.
The MCL1 lead not only permits differentiation of ectopic complexes (ventricular from supraventricular with aberrancy), but MCL1 keeps the defibrillation platform open for defibrillation pads or paddles. MCL1 also helps the Paramedic distinguish between right and left bundle branch blocks. A new onset left bundle branch block as a sign of an acute coronary event will be discussed later.
Perhaps the most pressing reason to use MCL1 as a monitoring lead is that it views the anterior wall. The left coronary artery (LCA), including the left anterior descending coronary artery (LAD), are commonly occluded during an acute coronary event and these arteries provide blood to the anterior wall of the left ventricle. MCL1 provides a vantage point from which to monitor the anterior wall and quickly identify lethal threatening dysrhythmias such as ventricular fibrillation.
Preparation of Skin
Electrodes are designed to adhere to and transmit electrical signals from a warm, dry, flat skin surface. In order to obtain these conditions, the Paramedic must take several steps to prepare the skin before applying the electrode.13
First, the skin should be relatively free of hair. The Paramedic can clip some hair to ensure electrode contact. Some Paramedics use single-blade razors to clear unwanted chest hair. However, if the patient receives anticoagulants later, then microlacerations created by the razor may bleed. Some Paramedics prefer to use disposable hair clippers specifically designed for this purpose. However, handheld bandage scissors, the type with the blunted tips, are adequate to trim chest hair.
Next, skin oils must be removed. Skin oils reduce the adhesion of the electrode and hinder penetration of electrode gel. An alcohol-soaked pad applied to the area and then pressed against the skin in an outward-circling motion will remove dirt, oil, and other particulates which could prevent proper adhesion of the electrode. Visible perspiration also can prevent proper adhesion of the electrode. The alcohol pad also helps to evaporate perspiration. The skin in the target area should then be dried with gauze or a towel prior to placement of the electrodes in order to remove debris and remaining alcohol.
If the patient is grossly diaphoretic, it may be helpful to apply tincture of benzoin. Tincture of benzoin is a topical lotion that, when dried, is tacky to touch and helps electrodes adhere to the skin. It is important to not apply tincture of benzoin directly over the electrode site as it does not conduct electricity well. Properly applied, the tincture of benzoin should leave a bull’s eye-appearing ring in which the middle is clear of the benzoin.
Finally, the best ECG signal is obtained when the area is gently abraded to remove dead skin cells and to improve circulation (i.e., increase warmth) to the area. The use of fine grit sandpaper (commercially available for this purpose) or even a gauze pad to abrade the skin can markedly improve the quality of the ECG signal.
Systematic Approach to ECG Rhythm Interpretation
A rapid and accurate interpretation of a patient’s ECG rhythm is important and potentially life-saving. To attain speed and accuracy, the Paramedic must take a disciplined approach to ECG interpretation. Faithful adherence to a systematic approach analysis of the ECG rhythm strip, a process called ECG interpretation, promises the best results in the shortest amount of time.
There are a number of ECG interpretation schemas available. Some take a simple left to right approach to reading an ECG, similar to reading a topic. The method originally described by Dr. Henry J. L. Marriott works well in the out-of-hospital environment as it focuses on rapid identification of high-risk patients.14 Dr. Marriott’s systematic approach to ECG interpretation also can be easily integrated with the algorithmic approach to advanced cardiac life support advanced by the American Heart Association. Regardless of the method of ECG interpretation chosen, the Paramedic should master that technique and resolve to use that systematic approach with each ECG tracing.
Descriptive Analysis
Some Paramedics have a tendency to quickly label an ECG rhythm because it looks like another ECG rhythm the Paramedic has seen before. This practice relies on pattern recognition. The use of pattern recognition is poor practice. Errors in ECG interpretation can be made when Paramedics fail to note the fine nuances that differentiate one rhythm from another (e.g., the difference between a bradycardia with U waves versus a sinus bradycardia with a heart block).
A descriptive analysis provides the building blocks to an ECG interpretation. Using the Marriott method of analysis, the elements of the descriptive analysis would consist of the rhythm, rate, width of the QRS complex, and atrial activity.
Armed with a descriptive analysis, the Paramedic assembles the information and, using an understanding of cardiac anatomy (specifically electrophysiology), generates a rhythm interpretation.
On occasion, an ECG rhythm strip baffles a Paramedic. The practice of using descriptive analysis allows the Paramedic to accurately describe the ECG rhythm strip to a physician or another colleague who, in turn, may be able to interpret the rhythm even without benefit of seeing the rhythm strip.
STREET SMART
An ECG interpretation should not be made by solely observing the ECG monitor. Before an ECG interpretation is made, the Paramedic should print out a hard copy of the rhythm displayed on the ECG monitor and, using descriptive analysis, come to a conclusion about the rhythm, documenting that interpretation.
Emergency Decision Making
Some medical emergencies are time-sensitive. Unfortunately, there may not be time to come to a comprehensive interpretation about an ECG rhythm before definitive action must be taken. This fact is best evidenced by the advanced cardiac life support algorithms. Many of these algorithms intend that the Paramedic establish a gross analysis of the ECG rhythm strip (e.g., "wide complex tachycardia") in order to use the algorithm. This permits quick action to resolve the dysrhythmia. A descriptive analysis, as suggested by the Marriott method, lends itself to this type of swift decision making.
STREET SMART
An ECG monitor is a valuable tool but is limited by the Paramedic’s ability to tie the interpretation of the rhythm strip to the clinical picture. The assessment of an ECG rhythm strip provides only one piece of data in the clinical picture. Only when a Paramedic takes this data, adds it to the history, and uses the information obtained from the physical performed on the patient, can a diagnosis be made.
Determining the Isoelectric Line
The first step in an ECG interpretation is to determine the isoelectric line. The isoelectric line indicates that period of time when the myocardium, particularly the ventricular mass, has been repolarized and awaits depolarization. The isoelectric line extends from the end of the T wave to the start of the ventricular depolarization represented by the QRS complex. An isoelectric line on the monitor and on the rhythm strip should appear as a flat line between ECG complexes.