KEY CONCEPTS:
Upon completion of this topic, it is expected that the reader will understand these following concepts:
• Use of ECG as a tool
• Correct application of electrodes
• Troubleshooting the equipment
• Interpretation of rhythms
Case study:
Jane Sheehan had called EMS because she felt faint and her heart seemed to be beating too fast. The first response unit had started her on oxygen, obtained vital signs, and was asking questions about the event when the Paramedic unit arrived. The Paramedic received report while placing Ms. Sheehan on a cardiac monitor. The Paramedic quickly interpreted the rhythm, verified that Ms. Sheehan did not have any drug allergies, and then outlined a plan of care for her.
The EMTs wondered aloud what the lines on the monitor meant and what part they played in determining a diagnosis and treatment.
OVERVIEW:
Paramedics use an electrocardiogram each day to monitor the cardiac rhythm in a significant proportion of their patients. Most cardiac monitors today have developed into comprehensive monitoring tools that measure other parameters including blood pressure, pulse oximetry, and capnography. In this topic, we will examine the use of the basic cardiac monitor to observe the patient’s cardiac rhythm.
The Monitoring ECG
In the eyes of the public and many healthcare providers, the distinction between basic life support and advanced life support is the electrocardiogram machine. The electrocardiogram (ECG) provides Paramedics with information about the electrical activity of the patient’s heart (i.e., the depolarization and repolarization of the heart through the cardiac cycle of systole and diastole). Armed with this additional data, the Paramedic can make better clinical decisions regarding treatment and transport.
By interpreting the ECG’s rhythm for disorder, the Paramedic can come to suspect electrolyte disturbances that can cause errors of automaticity (conduction abnormalities) or errors of conduction, as well as signs of is-chemic heart disease. Any of these can indicate a potential life-threatening emergency. Furthermore, changes in a rhythm strip may be indicative of other medical conditions such as head injury, toxic exposure, electrolyte imbalance or other more fundamental disorders such as hypoxia and hypothermia.1
Continuous monitoring of the patient’s heart rhythm allows the Paramedic to note changes in the patient’s condition, as well as the patient’s response to treatments, and thus continue or alter treatment plans accordingly. The goal of prehospital ECG monitoring is to obtain a clear and accurate view of the heart’s electrical activity quickly and dependably.
When using an ECG, the Paramedic’s first priority should be to monitor the heart for the presence of any life-threatening dysrhythmia. The utilization of a diagnostic 12-lead ECG always comes after the patient’s initial rhythm has been confirmed.
Portable ECG Equipment
Portable ECG equipment consists of an oscilloscope and a printer needed to review and record ECG. The original oscilloscopes on an ECG machine operated similar to the first television sets. A beam of electrons struck a phosphorescent screen and produced a point of light. Slight differences in voltages cause movement of the beam, which is displayed on the screen as fluctuations in the point of light. The point of light could be seen to move either as an upward spike (a positive deflection) or in a downward deflection (a negative spike). The ECG oscilloscope is also called a cardiac monitor (Figure 33-1). The monitor is analogous to a computer’s visual display of the machine’s output.
Figure 33-1 A Paramedic’s cardiac monitor-defibrillator.
ECG Tracing
Like the original silver string galvanometer used in the first experiments by Willem Einthoven, the modern ECG machine senses the current changes, or fluctuations, between two electrodes—one negative and one positive—as a wave of depolarization cascades down the heart and displays that information on a screen.2,3 A downward deflection indicates that the electricity is flowing away from a positive, or monitoring, electrode. An upward deflection indicates that the depolarization wave is flowing toward a positive monitoring electrode. If the differences in the flow of electricity resulted in a zero net difference in direction (i.e., electricity was flowing both toward and away from the positive electrode (perpendicular) at the same time), then the resulting signal is equiphasic or flatline.
Using this technology, the movement of electricity within the body could be observed, by the bounce of a point of light, at any given moment. However, the flow of electricity within the heart as it travels down a conductive pathway takes time. Therefore, the dimension of time must be included if the meter is to illustrate the passage of electricity down the conduction pathway. Oscilloscopes can add the dimension of time by moving the point of light across the screen from left to right at a precise rate of speed. Speed is distance over time and is measured in fractions of a second in the heart.
Compared against a static grid placed over the oscilloscope, this horizontal left-to-right movement (manifested on the screen as a trace) can be measured and fluctuations expressed in terms of time (seconds or milliseconds). Any vertical fluctuations seen on the monitor can also be measured. Vertical fluctuations represent the voltage change from zero, either positive or negative. The change from zero can also be measured on a grid and is expressed in terms of millivolts (mV). The larger the voltage difference, the larger the fluctuation.
Current ECG monitors not only measure the energy and the speed of conduction, but they also have many other features that are valuable to the Paramedic.
Monitor Features
The standard ECG monitor typically features a sensitivity and sweep speed control, output printer, lead selector, rate counter, monitor brightness control, and alarms. Many ECG monitors also have telemetry capabilities. Telemetry is the ability to broadcast the ECG via telephone or radio to a distant receiver, typically located at a hospital.4-6
To make the ECG readable, the ECG monitor must have both a sweep speed control and a sensitivity control. The sweep speed control regulates the speed of the tracing on the monitor, and subsequently on the printout. The sensitivity control alters the size of the ECG tracing. Adjusting these functions on the ECG monitor provides the Paramedic with some advantages in certain clinical situations.
To facilitate analysis, and documentation, a printer was added to print out the ECG seen on the screen. The printer provides a printed hard copy of the ECG tracing visible on the ECG monitor. In many cases manufacturers have built in a 5- to 10-second delay between what is visible on the ECG monitor and what is being printed out. This momentary delay permits the Paramedic time to activate the printer if an irregularity in rhythm is seen on the ECG monitor and thus capture the dysrythmia.
In some instances one view, or lead, is better than another when trying to make an ECG interpretation. Lead selection (changing the electrical view of the heart without moving electrodes) permits the Paramedic an opportunity to observe the heart from several angles at an instant. Optional leads and lead selection are discussed shortly.
An added feature of many ECG monitors is the rate counter. The rate counter is a digital readout of the number of ECG complexes that pass in a minute, usually counting the tallest, or deepest, wave on the ECG. Some ECG monitors also have a flashing light, or other visible signal, that indicates when an ECG complex has passed across a point on the monitor. Some rate counters have an audible signal which indicates the passage of an ECG complex across the monitor. The volume of these counters can be adjusted, or shut off, to reduce noise pollution on scene.
The purpose of an ECG monitor is to alert the Paramedic to potentially life-threatening dysrhythmias. To that end, some ECG monitors have alarms that will indicate, via visible and/or audible signal, that a patient’s heart rate is above or below a certain rate. The Paramedic often has the option of choosing the rate values (called the alarm limits) according to the patient circumstances. Some EMS agencies do not permit Paramedics to alter alarm limits or to disable alarms. This fail-safe device offers another level of security to permit early detection of potentially life-threatening dysrhythmias.
Finally, an additional feature on some ECG monitors is an ability to adjust the brilliance of the ECG monitor. Depending on ambient light conditions, it may be desirable to turn up the brilliance of the ECG monitor or to dampen it in order to improve the quality of the ECG.
Monitor Adjustments
Many monitors permit the Paramedic to adjust certain variables in order to improve the ECG tracing’s usefulness. For example, most monitors available to the Paramedic allow a change in speed and amplitude of a tracing. The Paramedic may want to change the speed of the rhythm passing by on the screen. An alteration in the speed of the tracing is an alteration in sweep speed. Standard sweep speed is 25 mm/second. Increasing the sweep speed to 50 mm/second will stretch out the trace and make the trace appear slower than it actually is. However, slowing sweep speed will also allow for closer examination of key features on the ECG, such as changes in the segments or minor deflections in the QRS.
The Paramedic may need to also enlarge the tracing shown on the monitor. This is called increasing the gain. The gain increases the size of the tracing shown on the monitor screen. Occasionally key features of the ECG are too small for clear examination without increasing the gain. By adjusting the gain, the Paramedic can get a clearer picture. Conditions which can cause low amplitude include a variety of medical conditions (Table 33-1).
Calibration
The ECG monitor is a medical device. As such, Paramedics should regularly ensure that the ECG monitor is accurate. Any number of medical interventions may be performed, including defibrillation and medication administration, based in large part upon the ECG tracing. A faulty ECG monitor could lead to an error of treatment. For this reason an ECG monitor should regularly serviced by a biomedical engineer who will re-calibrate the ECG monitor to factory specifications.
On a daily basis, and to assess accuracy of the ECG monitor, the Paramedic compares the ECG machine’s operation against standard settings (i.e., industry standards). Making sure that sweep speed and gain is up to standard is called calibration. Most ECG monitors self-calibrate, internally setting standard sweep speeds and gain, when initially switched on.
Table 33-1 Conditions That May Cause a Low-Amplitude ECG
|
• |
Amyloidosis—deposits of proteinaceous mass in muscle fibers |
|
• |
Hypothyroidism (a.k.a. myxedema) |
|
• |
Restrictive cardiomyopathy |
|
o Endomyocardial fibrosis |
|
|
• |
Pericardial effusions |
|
o Hemopericardium |
|
|
o Infectious transudate |
|
|
• |
Pericardial tamponade |
|
• |
Tension pneumothorax |
|
• |
Obesity |
|
• |
Hypothermia |
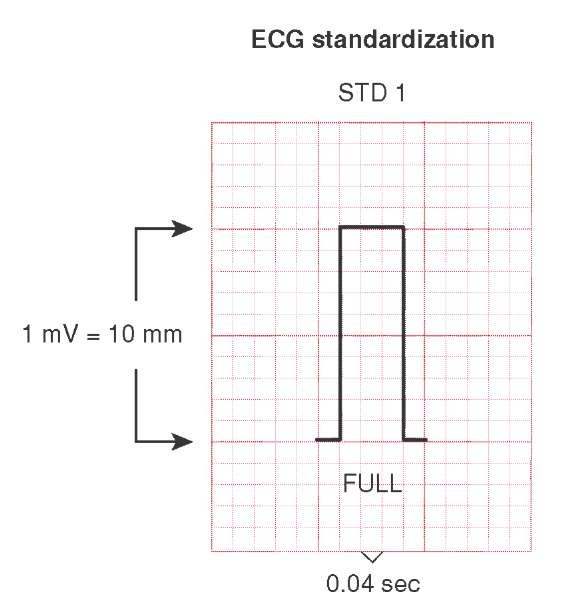
The calibration mark (Figure 33-2), visible at the beginning of the ECG printout, is a square wave that is 10 mm high, or 1 mV, and 10 mm wide. Each box measures 0.1 mV vertically and 0.4 mm horizontally. The calibration mark is created by a calibration impulse, an electric impulse, by the ECG machine. The resulting wave should be sharply delineated (i.e., quick corners that make a squared wave).
ECG Paper
Reading an ECG on the monitor can be difficult at times. Therefore, a hard copy can improve the accuracy of the analysis. For this reason, most Paramedics print out a copy of the ECG, called an ECG rhythm strip. The paper used for ECG recordings is imprinted on heat-sensitive paper via heated stylus or is printed by a laser. It is lined in a manner similar to graph paper to enable a Paramedic to accurately measure and compare ECG waves.
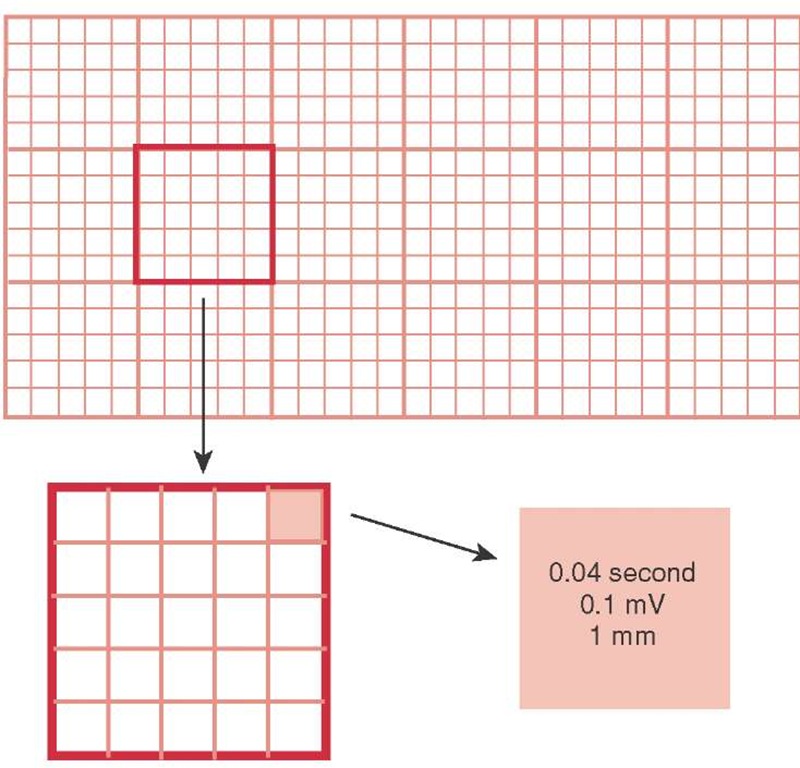
In order to determine regularity, rate, timing, and amplitude of the ECG features, the Paramedic must understand the grid structure of ECG paper. The paper is lined vertically and horizontally (Figure 33-3). On the vertical axis, a line occurs every 1 mm and a darker line occurs every 5 mm. For the horizontal axis, a line occurs every 0.04 seconds and a darker line every 0.20 seconds. The amplitude markings are correct assuming there is a standard gain of 10 mm/mV, and the time markings are correct assuming a standard sweep speed of 25 mm/second.
When assessing the rate of a rhythm or the time frame of a feature on the ECG, the Paramedic will use the horizontal markings. The horizontal axis equals time (0.20 seconds per large square). When measuring the amplitude of a feature, the Paramedic will use the vertical axis. The vertical axis equals amplitude, which can be roughly equated to the strength of the electrical signal.
Figure 33-2 Normal standardized calibration mark.
Figure 33-3 The standard ECG graph.
Wire Systems
The wiring harness, also called the ECG cable, connects the electrodes to the ECG monitor and is a single thick cable that separates into three, four, or five thinner wires. (Some harnesses will have an additional port that will accept a six-wire plug to enable the acquisition of a 12-lead ECG.)
The machine end of the harness has a pin connector that must be set firmly into its socket in order to avoid a poor connection, which will create an unreadable signal. The thinner wires are connected to electrodes at the distal end. These, in turn, are placed on the patient.