Sphygmomanometer
Blood pressure can be measured indirectly with a sphygmomanometer. This device consists of an inflatable bladder, enclosed in a cuff that is attached to a bulb or a pump; the bladder also has a deflating mechanism. The cuff is wrapped around the arm. Cuffs come in various sizes, as indicated in Table 46-5. If an incorrect size is used, accurate compression of the artery may not occur and the measurement will be incorrect.
Key Concept Blood pressure may be measured on the forearm or on the leg, as long as the appropriate size cuff is used. The pressure readings from all locations on the body should be approximately the same. Indicate the use of a site other than the upper arm.
In some cases, the indirect BP reading is obtained with an aneroid sphygmomanometer by listening to the heartbeat with a stethoscope. The stethoscope is placed over the brachial artery on the inside bend of the elbow. The stethoscope magnifies the sound of the heartbeat within the arteries.
Occasionally, you may see a mercury manometer in a client’s home. The placement of the arm wrap is the same for all types.
Nursing Alert If you find a mercury blood pressure manometer in a healthcare facility report it to your supervisor immediately. In the client’s home, encourage the client to replace the mercury manometer with an aneroid or electronic model.
Aneroid Manometer
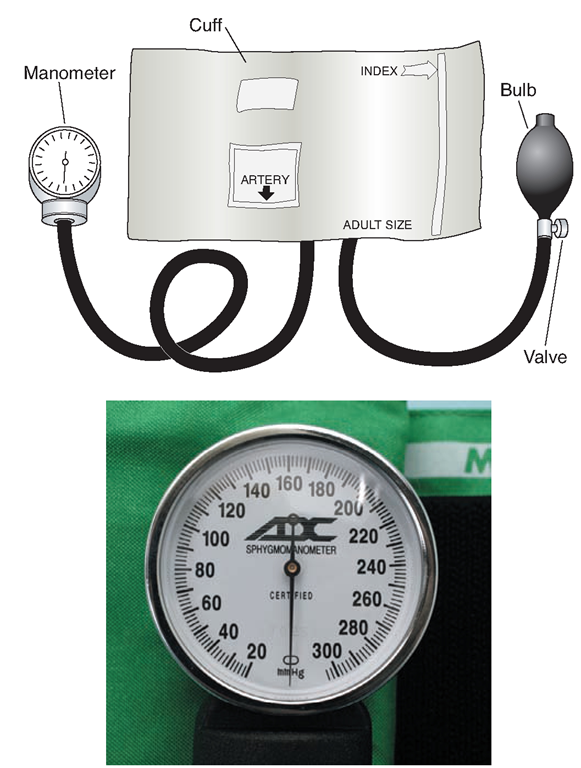
With the aneroid (spring-type) manometer, the arm wrap is attached to a dial, rather than to an electronic device (Fig. 46-16). Pressure readings are observed on the dial. Estimating the systolic pressure in an emergency is possible with this method because the heartbeats can be seen as the needle bounces. Most facilities mount these manometers near the client’s bedside, although a portable type is frequently used as well, particularly in rescue situations and in home care.
Electronic Blood Pressure Apparatus
In most healthcare facilities, the electronic monitor is used. This device does not require the use of a stethoscope.
TABLE 46-5 Recommended Bladder Dimensions for Blood Pressure Cuff
|
ARM CIRCUMFERENCE AT MIDPOINT* (cm) |
CUFF NAME |
BLADDER WIDTH (cm) |
BLADDER LENGTH (cm) |
|
5-7.5 |
Newborn |
3 |
5 |
|
7.5-13 |
Infant |
5 |
8 |
|
13-22 |
Child |
8 |
13 |
|
22-32 |
Adult |
13 |
24 |
|
32-42 |
Wide adult |
17 |
32 |
|
42-50+ |
Thigh |
20 |
42 |
*Midpoint of arm is defined as half the distance from the acromion to the olecranon
In patients with very large limbs, the indirect blood pressure may be measured in the leg or forearm. Be sure to use the correct size cuff.
FIGURE 46-16 · An aneroid manometer; attached to a blood pressure (BP) cuff (top). Below, a close-up shows the indicator needle and the numbers.
The electronic blood pressure apparatus measures the BP via a sensor or microphone in the cuff and provides a digital display of the client’s BP. Many of these machines are automatic. The cuff is wrapped, a button is pushed, and the machine pumps up the cuff and displays the BP reading. The pulse and mean arterial pressure are usually displayed as well.
The cuff for the electronic BP machine is applied in the same manner as for the aneroid manometer. An arrow on the cuff indicates where the artery should be, in relation to the cuff.
In some situations, an automatic blood pressure cuff cannot be used. For example, in the client with Huntington’s disease or any other type of chorea or with severe tremors caused by medications, the automatic cuff will not register. The automatic machine reacts to the client’s movements and is not able to function. Some clients feel that the automatic cuff becomes too tight, and they cannot tolerate its use.
Nursing Alert Do not use a client’s arm for blood pressure measurement if it is compromised in any way For example, do not use the arm if the client has:
• A vascular access for dialysis, a stent, or fistula
• Had a recent mastectomy on that side
• An arm injury or open wound
• A splint or cast
• An IV or saline lock
If any of these situations exist, use the other arm. If both arms are unavailable, use of an alternate site, such as the leg, is necessary
Palpation
When a stethoscope is unavailable, blood pressure can be estimated using the aneroid manometer. Palpate pulsations of the artery as pressure is released from the cuff. Estimate the systolic pressure when the pulsation is first felt. You will also be able to visualize pulsations on the aneroid dial. Usually, it is possible only to estimate the systolic pressure through this technique, because pulsations do not diminish as the cuff pressure is released. Palpation may be the only technique for estimating BP if the client is in hypovolemic shock caused by hemorrhage or other emergency. In this case, the nurse often cannot hear the sounds. Electronic BP measurement is usually more accurate.
Doppler Ultrasound
If sounds are difficult to hear or indistinct, a Doppler ultrasound, instead of the stethoscope, may be used to amplify sounds. Similar to palpation, only the systolic pressure can be obtained using this method of determining blood pressure (see Fig. 46-12).
Measuring Blood Pressure
In Practice: Nursing Procedure 46-5 presents steps for measuring blood pressure using a manual or electronic cuff.
Key Concept Measure BP and pulse initially in both arms, especially if the client has known vascular disease or if the reading is not within normal range. A difference of 5 to 10 points commonly exists between arms. A difference in readings of more than 10 points usually indicates arterial occlusion in the arm with the lower pressure.
Whenever BP is measured with a manometer, listen to the heartbeat through the stethoscope and watch the manometer at the same time. When the cuff deflates, blood returns through the artery. Korotkoff’s sounds are heard in the stethoscope. There are five phases of Korotkoff’s sounds, as described in Figure 46-17. The onset of phase I is the recorded systolic pressure. The onset of phase IV indicates diastolic pressure in children, and phase V indicates diastolic pressure in adults. When using the electronic device, it is not necessary to listen to heart sounds; the systolic and diastolic pressures are indicated on the meter.
Measure BP when the client is resting and quiet. Physical exertion or emotional stress will affect BP. Prepare the client by explaining that the cuff on the arm may feel tight for a second or two; otherwise, the procedure is not bothersome and will take only a few minutes.
Sometimes, it will be impossible to measure BP in the client’s arm (e.g., in the client with an IV or the client recovering from mastectomy). Use the thigh if a cuff that is sufficiently wide and long (specifically identified as a thigh cuff) is available. Wrap the cuff at mid thigh with the cuff’s bladder in the back. Be careful to use a cuff that is the correct width. Auscultate over the popliteal artery in the back of the knee if a stethoscope is used.
FIGURE 46-17 · Korotkoffs sounds. The readings here are approximate, based on a blood pressure (BP) of 120/80. Phase I (following initial silence, the turbulence begins): Characterized by first appearance of faint but clear tapping sounds that gradually increase in intensity. The first tapping sound is recorded as the systolic pressure (about 120-110). Phase II: Characterized by blowing, muffled, or swishing sounds (about 109-100). These sounds may temporarily disappear; especially if the client is hypertensive. This absence of sound is called the auscultatory gap and may be as great as 40 points. Failure to recognize this gap may result in error, overestimating the diastolic pressure. Phase III: Characterized by distinct, loud, sharp sounds as the blood flows relatively freely through the increasingly open artery (about 99-88). These sounds are softer than those in Phase II. Phase IV: Characterized by a distinct, abrupt, muffling sound with a soft, blowing quality (about 87-80). The onset of this phase is recorded as the diastolic pressure in children. Phase V:This is the last sound heard before a period of continuous silence (below 80). The point at which the last sound is heard is recorded as the diastolic pressure in adults.
Key Concept The lower arm also can be used, with auscultation over the radial artery in the wrist. If using an alternate site for taking BP identify it in the documentation and use the same site continuously throughout the client’s care, to maintain comparable data. Be sure to document where BP values were measured if the site is unusual.
Orthostatic Blood Pressure Measurement
Some clients, particularly those who are older or taking certain medications, will experience a drastic drop in BP and/or an increase in pulse when changing from lying to sitting or from sitting to standing. A drop of as much as 25 points systolic or 10 points diastolic must be reported. When a severe drop in BP occurs, the condition is known as orthostatic or postural hypotension. See In Practice: Nursing Procedure 46-5 for the steps involved in taking an orthostatic blood pressure measurement.
Nursing Alert An orthostatic drop in blood pressure with an accompanying rise in pulse should be reported to the healthcare provider
Key Concept Certain medications, including many antiseizure medications and antipsychotics used in psychiatry commonly cause orthostatic hypotension. Clients on these medications often have orthostatic blood pressure readings ordered as a routine order The client with postural hypotension must be careful when rising, due to the danger of fainting.
PULSE OXIMETRY
In many situations, such as during the admission process or when the client is receiving supplemental oxygen, pulse oximetry is considered a component of baseline vital signs. Oximetry is a noninvasive procedure that uses a photoelectric impulse to measure the amount of light transmitted or reflected by deoxygenated versus oxygenated hemoglobin. It yields a measurement of the oxygen saturation of functional hemoglobin in the blood, indicated as a percentage. The instrument used is called a pulse oximeter or transducer. A sensor is placed on a finger, toe, or earlobe. The healthcare provider orders the minimum acceptable level of oxygen saturation before using supplementary oxygen. In Practice: Nursing Procedure 46-6 lists the steps in using a pulse oximeter.
KEY POINTS
• Temperature, pulse, respiration, and blood pressure are called vital signs (or cardinal symptoms) because they are indicators of functions of the body that are necessary to maintain life. Pulse oximetry is often included.
• Documentation of vital signs and pain is essential to collecting information regarding the client’s status and well-being.
• Temperature is the measurement of heat inside the body (core temperature). It is the balance between the heat the body produces and loses.
• Pulse is the vibration of the blood through the arteries as the heart beats. It is measured by rate and rhythm.
• Respiration is the process by which the lungs bring oxygen into the body and remove carbon dioxide.
• Blood pressure measures the pressure the blood exerts on the walls of the arteries. Rate and force of heartbeat, blood vessel condition, and blood volume determine the reading as the ventricles contract and rest.
• Pulse oximetry indicates the percentage of oxygen saturation in the hemoglobin.