Nonverbal Communication
Nonverbal communication (NVC) is sharing information without using words or language. NVC expresses emotions and attitudes, as well as enhancing what is being expressed verbally. NVC is one component of body language and is sometimes more powerful in conveying a message than is verbal communication. If verbal and nonverbal messages are not congruent, the receiver usually believes the nonverbal cues. Several components of NVC are presented in Box 44-1.
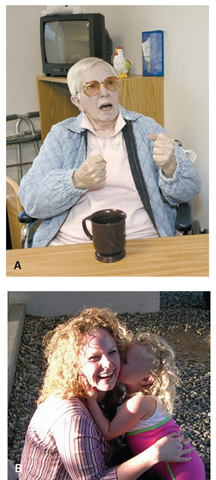
If the body language and verbal cues are not congruent, confusion occurs. For example, Mr. H., a young diabetic client, begins clenching and unclenching his fists when the nurse asks about his sexual activity. He says, “everything is fine,” through gritted teeth. Later, when he trusts the nurse more, he admits that he has been impotent for the past 6 months. Often, body language provides more powerful clues than verbal language because it points to the person’s true feelings (Fig. 44-3).
BOX 44-1.
Verbal and Nonverbal Communication
Verbal Communication
Use of words (e.g., speech, sign language, writing, slang) Oral Communication
Vocal sounds (e.g., grunt, snort)
Nonverbal Communication
Personal space (Proxemics)
Body characteristics: Body art, piercings, branding, plastic surgery, scarification, weight, clothing (cultural differences in what is considered to be beautiful)
Facial expression
Eye contact, eye gaze
Touch (Haptic communication)
Body gestures and movement (Kinesics): Posture, culturally related gestures, friendly gestures, warning gestures, obscene gestures, secret signals, gang signals Vocal characteristics: Geographic differences and accents, pronunciation, fluency/dysfluency, sarcasm Gender differences: Male/female relationships Cultural mores: Behaviors specific to a cultural group or geographic location (how people behave)
FIGURE 44-3 · Nonverbal communication is very powerful and conveys a very strong message, whether you intend it to do so or not. What message is being conveyed nonverbally by each of the people in these pictures?
Messages expressed through body posture and movements, gestures, facial expressions, and other forms of nonverbal behavior provide cues or suggestions to a person’s true feelings or beliefs. This study of body movements and posture, facial expressions, and gestures is referred to as kinesics. The nurse must be aware, however, that nonverbal behavior has different meanings for different people and in different situations. The nurse must be cautious when interpreting nonverbal cues. It is important to check with clients before making assumptions about the meaning of their body language. Remember, NVC includes factors such as clothing, body ornamentation, body shape and size, and gestures.
Key Concept Be sure that your verbal and nonverbal communications give a congruent message to clients. When verbal and nonverbal messages conflict (are not congruent), others are most likely to believe the nonverbal message.
Proxemics and Personal Space. Human proxemics or territoriality (the use of space in relationship to communication) varies greatly among individuals and between cultures or ethnic groups. This concept is closely related to the concept of personal space. Each person has an area around himself or herself called personal space. This area is reserved for only close friends or intimates. This culturally learned behavior varies greatly across cultures, although it may also vary from person to person within a culture or ethnic group. Other variables include sex and social status.
In traditional Western cultures, the areas of personal space or communication zones are approximately:
• Intimate (within 6 inches): behavior with loved ones,sharing secrets, physical assessment in healthcare
• Personal (6 inches to 4 feet): general conversation, interviews, teaching one-on-one, private conversation
• Social (4-12 feet): demonstrations, group interactions, parties
• Public (>12 feet): lectures, behavior with strangers
Although these concepts of proxemics are true for many Americans, they do not necessarily hold true for other cultures. For example, in the Middle East and Far East, the area of personal space is smaller. Consider this concept when working with clients from cultures that differ from your own. An action that would be considered an invasion of personal space by a person from one culture may be considered acceptable behavior by a person from another culture.
It is important for nurses not to unnecessarily violate the client’s personal space boundaries. If the nurse comes too close, it is considered an invasion. If the nurse is too far away, the client may feel isolated or ignored. In most cases, you can sense another person’s personal boundaries. Nurses, however, are often forced to invade a client’s personal space to provide care. It is important to be sensitive to the discomfort this may cause. The nurse should alert the client before touching him or her. Be careful to touch the client gently on the arm or hand before further intruding into his or her space; this practice offers comfort and reassurance so the client feels safer. Often, an approach from the side, rather than directly from the front, is perceived to be less confrontational.
Nursing Alert Remember that nursing care often involves the invasion of a clients traditional personal space. The nurse must be aware that some clients may react in a violent or assaultive manner when touched. This may be particularly true in psychiatry or with a client who has dementia. Do not touch any client without being alert for this possibility In addition, some clients may invade your personal space. The nurse needs to tell the client this is not appropriate. Seek assistance if this client behavior continues.
Sometimes, the client’s use of personal space is not cultural but indicates a mental or physical disorder. For example, the psychiatric client who consistently invades the personal space of others is said to be intrusive and may be threatening. Another client who maintains a very large personal space may be paranoid and afraid of contact with others. On the other hand, the client with a hearing or visual disorder may need to be very close to the speaker in order to determine what is being said. It is important to consider the reasons for variations in expected personal space boundaries when giving nursing care.
Eye Contact. Eye contact or eye gaze means looking directly into the eyes of the other person. Lack of direct eye contact has various meanings among cultures. Sometimes indirect eye contact means that a person is nervous, shy, or lying. However, it may also signify respect, as in Southeast Asian, Hispanic American, and Native American cultures. In these cultures, direct eye contact often signifies defiance or hostility. Staring may be interpreted by many cultures as open hostility, defiance, rudeness, or as a threat. Rolling the eyes is often interpreted as disgust or disbelief.
On the other hand, cultures such as those of the Middle East, consider a lack of direct eye contact as inattention, lack of concern, or even rudeness. Eye contact also varies between genders in some cultures. For example, men can have direct eye contact with each other, whereas women are expected to avoid direct eye contact when speaking to men. In Western cultures, direct eye contact or a wink between people is often a part of dating behavior.
Facial Expressions. Facial expressions convey messages of many emotions: joy, sadness, anger, and fear. Some people mask their feelings well, which makes understanding what they are thinking very difficult. Nurses learn to control facial expressions if they are experiencing emotions that may offend the client or block effective communication. For example, the nurse remains calm, with a neutral expression, when viewing wounds or smelling body secretions.
Body Movements and Posture. A twitching or bouncing foot may indicate anger, impatience, boredom, or nervousness. A slouched appearance may indicate depression or pain. Wringing hands may indicate fear, pain, or worry. Shrugging the shoulders implies, “I don’t know,” in many cultures. Pacing, rocking, and other repetitive movements may be a side effect of medications or may indicate fear or discomfort. Avoid making assumptions about these body language messages, however. You can ask the client what he or she is feeling if there is concern about these or other visual cues.
Gestures and Rituals. We use a number of gestures as a matter of course in daily life. Waving may indicate a greeting or “goodbye” or may be used to send someone away. A wink may indicate a mutual secret or may be seen as a flirting gesture. In some countries, people greet each other by kissing on both cheeks. In Western culture, the “air kiss” is a common greeting.
Nursing Alert It is very important to realize that some frequently used Western gestures may be interpreted very differently in other cultures. For example, the traditional Western "thumbs up” gesture is interpreted as an obscene gesture in countries such as Iran.
Personal Appearance and Grooming. Personal hygiene, general appearance, clothing, and body ornamentation relate information about clients. These nonverbal messages may convey clients’ true feelings about themselves, or they may be misleading, especially in illness. Individuals who are trying to meet their basic physiologic needs, such as oxygenation, may not have the physical or emotional energy to work on higherorder needs, such as cleanliness or grooming. Lack of personal care may also be a reflection of emotional factors, such as depression. In addition, persons with severe and persistent mental illness or out-of-control chemical dependency often have difficulty managing self-care. Homelessness may also prevent a person from bathing or washing his or her clothing.
FIGURE 44-4 · Therapeutic use of touch is the most potent nonverbal communication technique. A gentle and reassuring touch tells the client the nurse cares and is there to help. Be sure to use touch in this manner only if it is nonthreatening to the client.
Therapeutic Use of Touch. Touch, referred to as haptic communication, can say “I care” (Fig. 44-4). A firm touch can discourage a child from doing something dangerous; a light touch can encourage a person to walk down the hall. Touches can involve such movements as holding hands, a “high five,” or a pat on the shoulder. In some cases, touch by another person makes people anxious. Some people do not like to be touched, feeling that it invades their personal space. Be sensitive to the feelings of all clients. Sometimes, a nurse may need to touch a client to carry out a nursing procedure. In such a case, the nurse should verbally convey understanding of the client’s discomfort.
* Key Concept Nursing care revolves around communication: giving, receiving, and interpreting information. Communication is both verbal and nonverbal. Listening is an important communication tool as well.
Factors Influencing Communication
Many factors influence the effectiveness of communication. Some factors enhance communication. Other seemingly harmless factors create barriers between people.
Attention
A listening or attention barrier can occur because of lack of concentration. Selective listening may also be the culprit. In such a case, a person hears only what he or she wants or expects to hear. The nurse may not be paying attention and may not hear because of emotional responses to what the client is saying. Or, the nurse may be mentally framing the next question or thinking of something else. Sometimes, a client is experiencing pain or discomfort (physical or emotional) so great that he or she cannot listen or concentrate. The client may also be preoccupied with internal stimuli (e.g., auditory hallucinations). If both the sender and the receiver do not give, or are not able to give, full attention to the current communication, an effective nurse-client relationship may not occur. It may be necessary to postpone the interaction.
Special Considerations :CULTURE & ETHNICITY
Using Unbiased Language When Documenting Client Behaviors
• The nurse objectively describes eye contact, rather than applying judgments. For example, “The client looks at the floor when speaking” is descriptive and nonjudgmental. (A judgmental statement such as “good eye contact” implies that all clients should behave like most Western Europeans or Caucasian Americans.) The nurse might go on to state that (in the nurse’s opinion) the client is “insecure and afraid.” However, this assessment may be incorrect if, for example, the client is Native American and looking down is considered a sign of respect.
• The nurse objectively describes behavior related to personal space. For example, “client maintains approximately 3 feet of personal space and moves away when approached.” In the nurse’s opinion, the client might be described as “staff-avoidant.” However, this assessment may be incorrect, depending on the cultural background of the client.
• The nurse describes the tone and volume of the client’s verbalizations in objective terms. An objective statement might be, “client speaks very loudly.” The judgment that the client is “hostile” may be incorrect, however, when the nurse considers that in some cultures, all people speak very loudly. (On the other hand, the client may be hearing-impaired and may speak loudly as a result.)
A male nurse may write about a female client, “client refuses to speak.” However, it might be incorrect to say that the client is “paranoid” or “aphasic.” It is important for this nurse to remember that in some cultures, women are not permitted to speak to men outside their families.
Objective documentation may be, “client speaks softly.” However, rather than stating that client is “shy” or “afraid,” it is important to remember that in some cultures, women are expected to speak softly at all times.
• The use of profanity is common in some cultures and is considered part of everyday language. Documenting what the client says, in quotation marks, rather than making judgments, is objective.
• Many people of the world consider folk medicine or mystical beliefs to be a normal part of life. Therefore, if a client talks about the “evil eye” or a “cold disease,” documentation of the actual statement is appropriate and objective. A nurse might wrongly determine that this client is “delusional,” for example, when these beliefs are common to most members of that client’s culture.
The preceding are examples. The nurse uses the same general guidelines when documenting other nonverbal behaviors, such as reaction to pain, body posture, and general attitudes about health and illness. The nurse will be objective if he or she documents exactly what the client says and does, rather than making judgments based on the interpretation of those statements or actions. (Formal nursing assessments are made using NANDA guidelines. Unit 6 of this topic, The Nursing Process, describes these guidelines in more detail.)
Age
Age can be an advantage or disadvantage to effective communication. Very young or very old clients may be unable to communicate fully because of physical or intellectual capacity. Some clients are uncomfortable with caregivers much younger or older than they are. A young nurse may have difficulty working with a client near the same age. On the other hand, age can be an advantage. An older client may prefer to receive care from an older nurse, or a younger client may be more willing to accept instructions from an older nurse. An older client may also be energized by the presence of a young nurse.
Gender
Gender roles may influence nurse-client interactions. For example, a man who is accustomed to being in charge may resent being told what to do by a female nurse, particularly if she is much younger than he. A nurse who believes men should be tough may find it difficult to see a male client cry. A female client may be embarrassed by a male nurse performing personal care procedures. It is also important to consider the client’s ethnic background; in some cultures, interactions between men and women are specifically prescribed. Approaching a personal situation matter-of-factly or professionally may eliminate embarrassment.
Culture and Subculture
Cultural norms and traditions influence the behaviors and perceptions of all people, including nurses.Each nurse would be well-advised to develop an awareness of his or her own personal beliefs and practices, based on culture and ethnicity. Cultural differences are significant, for example, in relation to concepts such as personal space, eye contact, and interactions between men and women. Understanding and accepting differences is the key to developing therapeutic communication. The effective nurse actively seeks and maintains the client’s sense of self-worth by acting in a non-judgmental manner.
Key Concept Remember: A smile is part of the universal human language. It is understood by all.
Difficult Client Behaviors
Inappropriate behavior on the part of clients creates a barrier to communication.
Sexual Harassment. If a client sexually harasses you, consult with your instructor or team leader to handle this inappropriate behavior correctly. Sexual harassment is defined as any unwanted sexual activity. This includes any inappropriate or unwanted touching, as well as sexual statements, or lewd jokes or comments. The use of profanity and name-calling is also included. If a client continues these inappropriate actions after being warned, the nurse may consider pressing charges. (It is important to consider the client’s physical condition. For example, the client who has Alzheimer’s disease may not be totally responsible for his or her actions.)
Key Concept A nurse is never required to allow inappropriate behavior from a client.This includes verbal or physical abuse, as well as sexual harassment.
Aggressiveness. Some clients are very anxious or angry when admitted to a healthcare facility. They may respond with aggression, which may be directed toward the nurse or the situation in general. It is important for the nurse to remain objective and to practice assertiveness (confidence without aggression or passivity). Box 44-2 gives a brief description of aggressive and assertive behaviors and an introduction to assertiveness training for nurses.
Key Concept Remember that any aggressive behavior toward clients by a nurse, whether physical or verbal, constitutes assault on the part of the nurse.
Nursing Alert It is important to maintain your own safety If you feel that a client is threatening you and you are in danger.If you are in doubt, withdraw from the situation and ask for help.
Social Factors
Social acceptance of a particular illness plays a role in a person’s reaction to the illness. For example, a sexually transmitted infection or psychiatric disorder may be more difficult or embarrassing for the client than a disorder such as glaucoma or diabetes, because of society’s attitudes. The person with an arm or leg amputation or a colostomy may feel more self-conscious than the person who has had some type of surgery that is not visible to others.