Formation of Lymph
Body cells normally are bathed in tissue fluid. Some of this fluid drains into blood capillaries and flows directly into veins. Another group of vessels, called lymphatic vessels, also drains this fluid. The lymphatic vessels begin as a network of tiny closed-ended lymphatic capillaries in spaces between cells. These capillaries are slightly larger than blood capillaries and have a unique structure that allows interstitial fluid (ISF) to flow into them but not out. (Of the body’s ISF, 10%-20% enters the lymph capillaries.) As ISF comes into contact with blood, it accumulates more lymphocytes, other cells, proteins, and certain waste products. When this fluid enters lymphatic conduits, it becomes the thin, watery, colorless liquid known as lymph. Because lymph originally derives from plasma, its composition is much the same, except that lymph is lower in protein content. Specialized lymphatic capillaries called lacteals absorb digested fats and fat-soluble vitamins in the small intestine.
Movement of Lymph
Lymphatic vessels contain one-way semilunar valves that prevent backflow of lymphatic fluid into the ISF. The functional unit of larger lymph vessels is the lymphangion (the segment between two valves). This structure can move or stop the flow of lymph. Lymphatic vessels are located both superficially (near the skin surface) and deeper in the body. The larger lymphatic vessels are lined with a single layer of flattened endothelial cells surrounded by smooth muscles encircling the endothelium. (These muscles only change the size of the vessel’s lumen.) The outer layer, the adventitia, consists of fibrous tissue. The smallest lymphatic capillaries have only the single layer of endothelial cells.
Most lymphatic vessels are located near the venous system and are named accordingly. For example, femoral lymphatic vessels are in the thighs. Lymphatic vessels carrying fluid eventually form a network of vessels in specific areas of the body. These areas are called regional nodes. After the fluid moves through the nodes, it is transported by other lymphatic vessels to either the right lymphatic duct or the thoracic duct.
Lymphatic fluid is propelled through the body by rhythmic contractions. These contractions occur because of changes in abdominal and thoracic pressure during breathing and skeletal muscle contractions. The pulsation of arteries also aids in movement of lymph. All of these promote the return of venous blood—and subsequently lymphatic fluid—to the heart.
Lymph Nodes and Nodules
Small bundles of special lymphoid tissue termed lymph nodes are situated in clusters along the lymphatic vessels. An encapsulated lymph node consists of an outer area, the cortex, containing lymphoid follicles; and the inner portion, the medulla. An indentation, the hilum, provides a portal for efferent lymph vessels and for arteries and veins. Many lymph nodes appear in the neck (cervical), groin (inguinal), and armpits (axillary) (see Fig. 23-4). Before lymph reaches the veins or lymphatics, it passes through these nodes.
Lymph nodes perform several vital functions. The most important is that of filtering out and destroying pathogens. The “swollen glands” that may appear in a person’s cervical, inguinal, and axillary regions during illness are really lymph nodes at work. The nodes have enlarged as their macrophages (phagocytic cells) eat and destroy invaders. When palpated, these enlarged, non-malignant nodes are soft and tender and may become painful.
Lymph nodules are small masses of non-encapsulated lymphatic tissues that stand guard in all mucous membranes. Because membranes line cavities that open to the external environment, these nodules are in strategic locations to filter substances that enter the body. Mucous membranes line the respiratory, gastrointestinal, urinary, and reproductive tracts.
Lymph Nodes and Cancer
Cancer cells can travel from their primary site of invasion to distant sites by way of the lymphatic circulation and lymph nodes. Lymph nodes may either function to filter out cancer cells or may inadvertently spread cancer to other body sites. For this reason, when cancer surgery is performed, the lymph nodes in the area are tested. If no cancer cells are present in adjoining lymph nodes, the cancer was most likely localized to its original site. If cancer is found in the lymph nodes, it is said to be spreading or metastasizing. In some cases, the adjoining lymph nodes are removed during surgery. Removal may be a precautionary measure or may be necessary because the nodes already contain cancer cells. Palpable cancerous lymph nodes may be enlarged and, unlike nodes fighting infection, feel firm and non-tender.
Lymphatic Organs
The lymphatic organs are the tonsils, spleen, and thymus. They are masses of lymphatic tissue with somewhat different functions than those of the lymph vessels or nodes. The tonsils and spleen are designed to filter tissue fluid, although not necessarily lymph. The thymus plays a role in the development of the immune system.
Tonsils
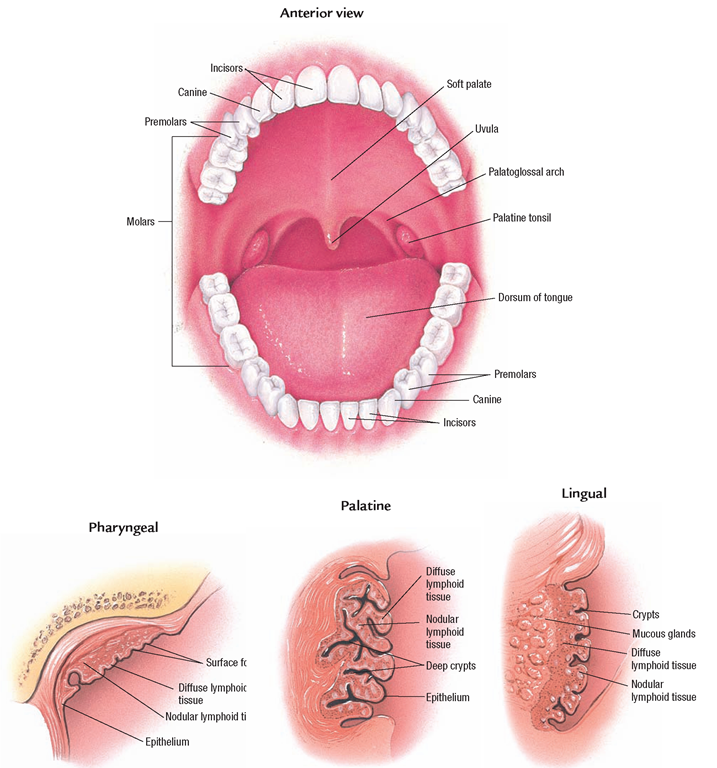
Tonsils form a ring of lymphatic tissue around the pharynx (Fig. 23-5). This tissue forms a protective barrier for substances entering the oral and respiratory passages. The tonsils may become so infected that removal (tonsillectomy) is advisable. A slight enlargement, however, is not an indication for surgery.
FIGURE 23-5 · The tonsils are lymphatic tissue. They form a protective ring around the pharynx.
Key Concept In the past, children often had their tonsils removed at the first sign of infection (tonsillitis). Today it is known that tonsils (because they are lymphatic material) provide filtration and protection; they are removed only if absolutely necessary
Spleen
The spleen is an organ containing lymphoid tissue designed to filter blood. It is a somewhat flattened, dark purple organ about 6 inches (15.24 cm) long and 3 inches (7.62 cm) wide. The spleen consists of red pulp, which fills the interspaces of the spleen’s sinuses and white pulp, sheaths of lymphatic tissue surrounding the arteries of the spleen. The spleen is located directly below the diaphragm, above the left kidney, and behind the stomach.
The spleen has several functions. In the fetus, the spleen (along with the liver) has a role in blood cell formation (later this role is taken over by red bone marrow). In an adult, the spleen destroys old RBCs and forms bilirubin from the hemoglobin. It acts as a reservoir for blood, which can be released to the body quickly in an emergency, such as hemorrhage. (In the event of bone marrow failure, the spleen may also produce some RBCs.) The spleen filters and destroys pathogens and other foreign materials from the blood. Specially treated B-lymphocytes that produce antibodies against foreign antigens and T-lymphocytes that attach to invading viruses or foreign entities are contained in the spleen. Both of these lymphocytes have an active role in the immune system of the body.The spleen also contains monocytes, which become macrophages in the spleen, to fight infection by phagocytosis. As described earlier in this topic, all of these agranulocytes help the body fight infection in different ways.
Although its functions are important, the spleen can be removed without ill effects. An adult without a spleen, however, is more susceptible to some bacterial infections, such as pneumonia and meningitis. After the spleen is removed, the liver, bone marrow, and lymph nodes assume some of the spleen’s functions.
Thymus
The thymus is a ductless gland in the upper chest, under the sternum. It is important in the immune response, although its function declines with age. During fetal and early neonatal life, the thymus entraps immature stem cells in its reticular structure. It sensitizes these cells so they are able to mature into a specific type of lymphocyte (eventually becoming T-cells). If the thymus fails, the person’s cell-mediated immunity is non-functioning.
System Physiology
BLOOD CIRCULATION
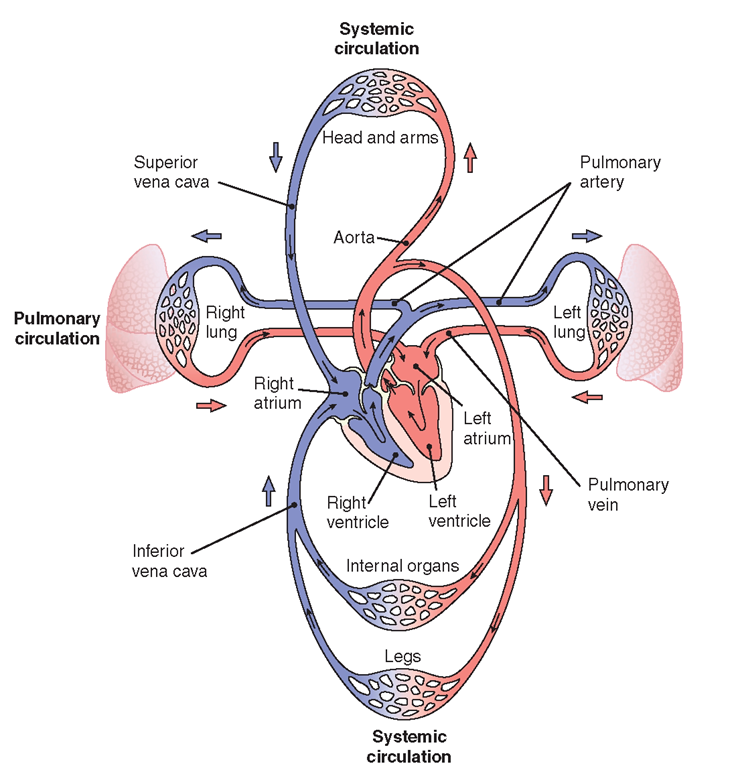
Blood flows in a circuitous route throughout the body. The blood vessels, subdivided into two circuits (pulmonary and systemic), together with the four chambers of the heart, form the closed system for the flow of blood.
Pulmonary Circulation
The phase of circulation in which blood is pumped through the lungs to get rid of waste products (particularly CO2) and pick up oxygen (O2) is called pulmonary circulation. Blood is pumped out of the heart into the lungs by the right ventricle. It enters the pulmonary artery (the only artery in the body that carries deoxygenated blood) and continues to capillaries in the lungs. Here, carbon dioxide is exchanged for oxygen. Small veins collect oxygenated blood from the lung capillaries. These veins combine eventually into four pulmonary veins, which pour oxygenated blood into the left atrium of the heart. (The pulmonary veins are the only veins that carry oxygenated blood.) From here, the blood is pumped to the rest of the body (systemic circulation). Figure 23-6 illustrates pulmonary and systemic circulation.
FIGURE 23-6 · The heart is a double pump. The pulmonary circuit carries blood to the lungs to be oxygenated; the systemic circuit carries blood to all other parts of the body.
Systemic Circulation
From the left atrium, oxygenated blood enters the left ventricle. The left ventricle pumps blood out of the left side of the heart into the general or systemic circulation. As stated, the purpose of blood circulation is to carry nutrients and oxygen to body cells and to return with accumulated waste products. As blood leaves the left ventricle, it surges into the largest artery of the body, the aorta. The aorta is further divided into the ascending aorta, aortic arch, thoracic aorta, and abdominal aorta, which is divided into smaller arteries. The blood travels through smaller and smaller arterial branches. From the smallest arteries, the arterioles, the blood enters the capillaries, where oxygen and food are exchanged for waste products.The blood then returns to the heart via capillaries, then venules, then larger veins, and finally through the inferior and superior vena cavae to the right atrium, thereby completing the circuitous route.
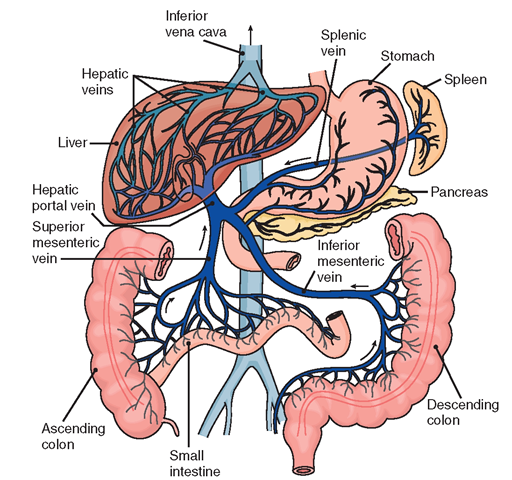
Hepatic-Portal Circulation. The hepatic-portal circulation is a subdivision of systemic circulation. It is an efficient detour in venous return, directed at transporting raw materials (carbohydrates, fats, and proteins) from the digestive organs and spleen to the liver. The hepatic-portal circulation is unique because it begins and ends with capillaries (Fig. 23-7). The capillaries from the stomach, intestine, spleen, and pancreas empty into veins. These veins drain into a common vessel, the portal vein, which leads into the liver.
In the liver, blood again enters capillaries, called sinusoids. Here, the liver extracts appropriate materials and chemically modifies them. The liver synthesizes, stores, detoxifies, regulates, and transforms these raw materials into useful substances to meet body needs. The useful substances and blood then empty into the hepatic vein which leads to the inferior vena cava.
FIGURE 23-7 · Hepatic -portal circulation.
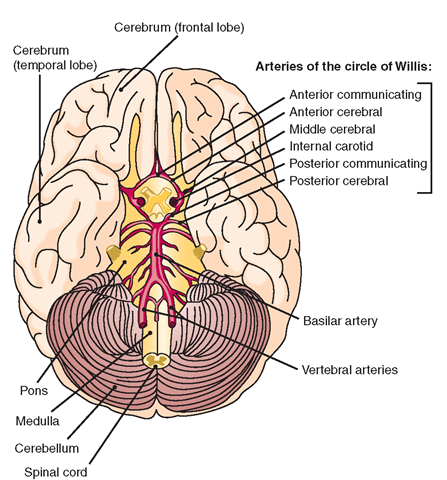
Cerebral Circulation
Circulation to the brain is vital in maintaining life and the ability to function. Anteriorly, one branch of the common carotid artery is the internal carotid artery. The internal carotid anastomoses (connects) with the circle of Willis, thus providing oxygenated blood to the brain. Oxygenated blood also arrives at the brain by another route. The right vertebral artery and left vertebral artery branch from the subclavian artery at the posterior aspect of the brain. These two vertebral arteries join at the brainstem and create the basilar artery. From here, blood is transported to the circle of Willis. The circle of Willis (cerebral arterial circle) is formed by the anterior communicating artery, posterior communicating artery, anterior cerebral artery, posterior cerebral artery, and internal carotid artery. Figure 23-8 shows the arteries that supply the brain, including the arteries of the circle of Willis. All these arteries supply different areas of the brain with blood. Blood returns to the heart via venous sinuses that transport blood to the internal jugular veins and back to the heart.
Cerebral blood flow is 10%-15% of total cardiac output. Blood pressure is one factor that has an impact on blood flow. Adequate cerebral perfusion (blood flow to the brain) is required. The mean arterial blood pressure (MABP) is calculated based on the relationship between the systolic and diastolic BPs. The brain requires a continuous flow of blood because it requires a constant supply of oxygen and nutrients (specifically glucose) to survive. The brain does not have the ability to create a collateral circulation as the heart does in some cases.
The circle of Willis is important because it allows blood to continue to flow in the brain if one of the arteries that supplies the circle of Willis is blocked. (An embolus is a clot that can lodge in an artery, thereby causing a blockage.) In the brain, the middle cerebral artery branch is the most likely location for emboli (Porth, 2009). A disruption of blood flow for any reason, for even a short period of time, can cause unconsciousness. Brain damage or death can occur if the disruption lasts for more than a few minutes (due to brain cell death).
FIGURE 23-8 · Arteries that supply the brain, viewed from behind. The arteries that make up the circle of Willis are shown in the center of the brain.
Blood-Brain Barrier. The blood-brain barrier (BBB) is an “adaptation of the circulation” that protects the brain. Specialized cells in brain capillaries allow only certain substances from the blood to enter the brain. Capillaries in the brain are less permeable and much tighter than other capillaries in the body, thus limiting what substances are admitted into the cerebral circulation and to brain tissue. Also, specialized brain neuroglia called astrocytes assist in creating selective permeability in the brain.
Key Concept The blood-brain barrier works to protect the brain from harmful substances.