Autism Spectrum Disorders
Autism spectrum disorders (ASDs) are lifelong, complex developmental disorders characterized by intellectual, social, and communication deficits. Autism is not actually a disease, but a syndrome of specific behaviors that vary widely, thereby making it difficult to diagnose. The cause of autism is unknown. The ASDs are the second most common serious developmental disability after intellectual impairment.
Signs and Symptoms. Autistic children typically demonstrate a profound lack of social interaction. They do not respond to verbal stimuli and do not like to cuddle or be touched. They may show bizarre attachments to mechanical objects.
Autistic children often display repetitive or ritualistic behaviors, such as rocking, head banging, clicking of teeth, or turning the head back and forth. Impaired verbal and nonverbal communication, temper tantrums, and self-destructive behaviors also may be evident. Echolalia is one form of language impairment that may be seen. These children are believed to be preoccupied within themselves, perhaps having fixed delusions and hallucinations. They sometimes become very upset or aggressive when interrupted.
Diagnosis. Because there is no specific test or procedure to diagnose autism, recognition of symptoms at the earliest possible age is highly significant. Research has strongly demonstrated that early intervention and intensive behavioral skill therapy are very important. Other physical and emotional disorders need to be ruled out. Autism is often associated with some degree of mental or cognitive impairment. Some autistic children are profoundly impaired. However, a few may have typical autistic behaviors, but display superior intelligence in one particular area, such as math, art, or music, or have a photographic memory. These children may be referred to as an autistic “savant.”
Asperger syndrome is a type of autism with specific, often milder, symptoms. This individual typically has difficulties with social interactions. Persons with Asperger syndrome might have unconventional behaviors or interests, but they do not have language or intellectual disabilities.
Treatment. No known cure exists for autism and the prognosis varies widely, but early diagnosis and interventions help a child maximize his or her long-term potential. Psychiatric symptoms occur in approximately half of all autistic children during adolescence. Intervention requires professionals with expertise in speech, language, and behavior control. Education is a lifelong process.
Nursing Considerations. Emphasize the positive and focus on the child’s skills. Teach family caregivers to give the child immediate feedback and to continue interaction with the child using short sentences and simple commands. Remind caregivers to be concerned with the child’s safety, but to maintain normal daily routines.
Plumbism
Plumbism is lead poisoning. Lead, which is toxic to the human body, is found almost everywhere—in water, old paint, contaminated dust, and dirt.
Lead poisoning can be acute or chronic. If exposure is sudden, the poisoning is acute. If the exposure occurs over a long period of time, lead poisoning is called chronic. Symptoms of either acute or chronic poisoning vary widely. Effects of lead on the body depend on the client’s age, the amount inhaled or ingested, and how long the client has been exposed to the toxin.
One of the most common causes of lead poisoning in children is the ingestion of leaded paint chips. A 1978 federal law prohibiting the use of lead in paints has reduced the number of lead poisoning cases. Individuals living in older homes, usually in inner cities, remain at risk. Many times, older homes have chipped paint and plaster. Inquisitive, inadequately nourished, or emotionally deprived children may eat paint chips as well as other inedible things.
Continual sources of lead poisoning include water that passes through old pipes that contain lead. Additional culprits of poisoning include improperly disposed of lead in public landfills and industrial sources, such as mining, smelting, and recycling processes. Burning batteries releases lead into the environment.
Key Concept Eating nonfood items is termed pica.
Nursing Alert Lead is contained in items other than paint, such as leaded pottery or dishes, home remedies, shoes, old toys, old eating utensils, old pipes and plumbing, soil containing lead from old chipped paint, sand and dirt on playgrounds, air pollution from unleaded gasoline, and family members who bring lead dust home on their clothes. A child who inhales the dust from scraped, leaded paint can suffer the same deleterious effects as the child who eats paint. The buildup of lead can occur gradually
Signs and Symptoms. Early symptoms of lead poisoning are so general that they can be easily missed or attributed to other childhood illnesses. Damage can be done to the brain, kidneys, CNS, and red blood cells (RBCs). The most severe complication of lead poisoning is lead encephalopathy, which may result in a number of CNS disorders, including seizures, cerebral palsy, cognitive impairment, and ADHD. Untreated encephalopathy usually results in severe brain damage and death.
Long-term residual effects of plumbism include intellectual impairment, learning disabilities, or seizures. Early recognition of symptoms helps alleviate the long-term consequences of chronic lead poisoning. Damage that is done by lead poisoning cannot be reversed.
The signs and symptoms of plumbism include:
• Blue or blue-black line on the gums near the teeth
• Hyperirritability
• Anorexia, nausea, and vomiting
• Intermittent vomiting (lead colic)
• Abdominal pain
• Joint pain
• Headache
• Fatigue and decreased play
• Anemia, pallor, and decreased RBCs
• Constipation
• Behavior changes (sudden changes may indicate acute lead poisoning)
• Ataxia (unsteady gait), weakness, or clumsiness
• Decrease in intellectual and mental abilities (e.g., memory loss and poor school performance)
• Impaired level of consciousness
• Seizures
• Coma
• Encephalopathy (brain degeneration)
Diagnosis. Blood lead level (BLL) should be obtained from children who are at high risk or who demonstrate symptoms. Other disorders need to be eliminated as causes of symptoms.
Treatment. The individual first must be removed from the lead source. If the case is mild, the child is treated symptomatically. Anemia is treated with diet and iron supplements; seizures are treated with antiseizure medications.
High-risk children should be screened for elevated BLL. This includes children who live in homes built before 1950, have iron deficiency anemia, are exposed to contaminated dust or soil, or have developmental delays. Chelation is the administration of medications that bind to lead to remove it from the body. The drug of choice for chelation is edetate acid (EDTA) given intravenously (IV) and the heavy metal antagonist dimercaprol (BAL in Oil) given deep intramuscularly.
Nursing Considerations. Plumbism may easily be missed as a possible cause of childhood disorders. During well-baby and well-child checkups, the nurse should consider plumbism if the child is at risk or demonstrates symptoms. Changes in play activities, new aches and pains, and altered intellectual abilities may be seen by parents, but not reported to healthcare providers. The source of lead must be eliminated.
Key Concept Public education and prevention are the most effective approaches for eliminating the problem of lead poisoning.
LONG-TERM NEUROMUSCULAR DISORDERS
Cerebral Palsy
Cerebral palsy (CP) is a general term used to describe movement and coordination disorders in children that are the result of some form of brain damage. It may be accompanied by intellectual and learning deficits. Unlike other movement disorders, CP is not progressive. Symptoms may appear at any time before age 2 years. It is the most common permanent physical disability developed in childhood.
The brain damage of CP has many causes. During the months of pregnancy, the causes include maternal infection, excess radiation, fetal anoxia, pregnancy-induced hypertension, maternal diabetes, abnormal placental attachment, and malnutrition. The premature or very low-birth-weight infant (<3.3 pounds or 1,500 grams) is at higher risk for developing problems that lead to CP than is the full-term, infant of normal birth weight. Postnatal causes include birth trauma, prolonged anoxia during childbirth or in very early infancy, brain infections (e.g., meningitis or encephalitis), head trauma, brain tumor, and cerebral hemorrhage or clot. Severe jaundice or kernicterus in the postnatal period owing to high levels of bilirubin can cause CP because the high bilirubin levels damage the infant’s delicate brain. Hearing loss and mental retardation can also result from kernicterus.
Signs and Symptoms. Characteristics of CP generally include the following to varying degrees:
• Muscle contractions
• Increased stretch reflexes
• Rapid alteration of muscle contractions and relaxations
• Muscle weakness
• Difficulty sucking or feeding
• Dysarthria (speech abnormalities)
• Visual and hearing abnormalities
• Contractures
• Limited range of motion
• Scissors-like gait, such as crossing one foot in front of the other to walk
• Walking on toes
• Seizures
• Delayed motor development, such as with sitting, crawling, or walking
• Learning disabilities
• Mental abilities that range from very intelligent to severe mental retardation
• Hypertension
• Underdevelopment of affected extremities
Classifications. There are four major classifications of CP.
1. Spastic cerebral palsy is the most common type of CP, representing 70%-80% of cases. Symptoms include increased muscle tone or spasticity, which may affect one or more limbs. The client’s muscles are stiff and movements awkward. Paralysis may be full or partial. Sensory abnormalities, such as speech, hearing, and vision deficits, may also be present. The condition is usually defined by a description of the parts of the body that are affected. These descriptions include spastic hemiplegia, which involves one side of the body; spastic diplegia, which involves both legs; and spastic quadriplegia, which involves the whole body (face, trunk, both arms and legs).
2. Dyskinetic (or athetoid) cerebral palsy involves about 10%-20% of clients with CP. This type of CP is characterized by slow, writhing involuntary movements, such as twisting, grimacing, and sharp jerks. These movements disappear during sleep and increase with stress. The child may have difficulty talking because of involuntary facial and tongue movements.
3. Ataxic cerebral palsy involves about 5%-10% of clients with CP. Tremors cause these clients to have difficulty controlling their hands and arms when they reach for an object. Typically, they have an unsteady gait, muscle weakness, a lack of coordination, and problems with depth perception and balance. Nystagmus (rapid, repeated movements of the eyeball) may be seen. During infancy, there may be a lack of leg movements. When the child begins to walk, he or she holds the feet far apart, causing a wide gait. The child with ataxic CP is unable to make fine or sudden movements.
4. Mixed cerebral palsy: About 20% of CP cases are combinations of more than one type of CP. The most commonly seen type of mixed CP has spasticity and athetoid movements.
Diagnosis. Cerebral palsy is diagnosed primarily by symptoms the child demonstrates during infancy. Certain critical observations can direct the healthcare practitioner to look closely for other symptoms. The infant who has difficulty sucking or has arm or leg tremors with voluntary movement should be checked for CP.
In children with CP, infantile primitive reflexes persist past the expected age of disappearance. The infant who crosses the legs when lifted from behind, rather than pulling them up, is also of concern. Another sign of CP is difficulty in diapering because the legs are hard to separate. The child tends to use the arms and hands, but not the legs.
Other disorders are ruled out by MRI, CT, EEG, and nutritional studies. Hearing and visual screening are necessary to determine the extent of disability.
Treatment. There is no cure for CP. Preventative measures, such as using car seats and wearing bike helmets, help minimize accidental head trauma. Disabilities associated with CP are permanent; treatment is multidisciplinary and aimed at preventing complications and maximizing the child’s potential. Helping the child learn self-care activities is a continuing goal. Improving communication through speech therapy and appropriate educational assistance is important.
Physical and occupational therapy help maintain the child’s muscle strength and assist with adaptive measures (Fig. 74-3). Braces, splints, or walkers may aid in ambulation. Orthopedic surgery is sometimes used to correct severe contractures.
Nursing Considerations. Cerebral palsy does not necessarily affect the length of life, but it does profoundly affect the quality of life. Adaptive care devices, such as hearing aids, glasses, vision-enhancing equipment, braces, and walkers, help with mobility and ADL. Education needs to be adapted to the needs and capacities of the child. In severe cases, institutionalization may be used instead of home care. Medications are supportive and used symptomatically. Muscle relaxants can reduce tremors and spasticity. Seizures can be controlled with anticonvulsants. Surgical interventions require that the nurse provide individualized pre- and postoperative care, keeping in mind the mental and physical abilities of the client, as well as the capacities of the family. Client and family teaching are very important. Care is necessary for the child as well as the adult who has CP. The family and the child will need much emotional support.
FIGURE 74-3 · A physical therapist works with a child with cerebral palsy to maximize mobility
Key Concept A water bed is a good idea for many disabled children.The movement of their breathing causes feedback and helps prevent joint pain and skin breakdown. The warmth often adds to comfort.
Duchenne Muscular Dystrophy
Duchenne muscular dystrophy (Duchenne-Landouzy dystrophy) is the most common degenerative muscular disorder in children. It is one of a group of X-linked, genetically transmitted disorders affecting boys and it is characterized by progressive atrophy of symmetrical groups of skeletal muscles. A lack of a protein product (dystrophin) in the muscles results in progressive muscle wasting with gradual loss of strength and increasing muscle deformities.
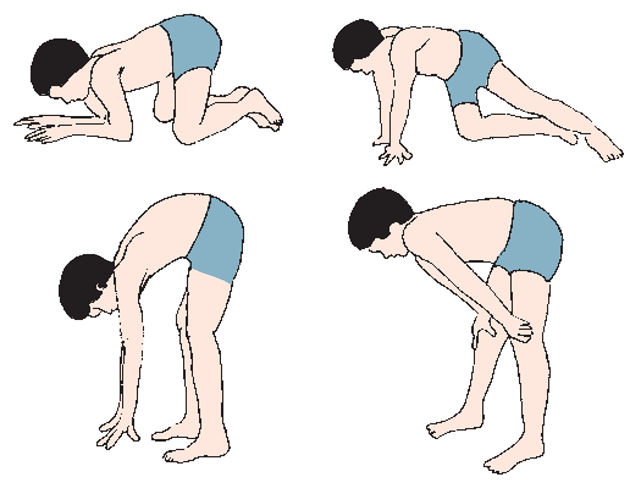
Signs and Symptoms. Symptoms begin to appear around the age of 3 years. Before this time, the child may have noticeable developmental delays. The child’s gait appears as a waddle and a positive Gowers’ sign occurs. A positive Gowers’ sign is exhibited when the child needs to use the upper extremity muscles to compensate for weak hip muscles (Fig. 74-4).
The child also may walk on the toes, fall frequently, and have difficulty hopping or running. These children often develop lordosis because of their unusual gait. Delayed intellectual development and borderline IQ may be present. Gradual muscle atrophy occurs and, by age 11 or 12 years, the child is unable to walk and becomes wheelchair bound. Contracture deformities can occur, especially of the hips and knees.
Deterioration of respiratory muscles results in cardiac problems and respiratory failure. In some cases, assisted respiratory ventilation can extend life. Muscles involved in swallowing are also affected, and tube feeding may be necessary. Clients with Duchenne muscular dystrophy rarely live beyond their 20s.
FIGURE 74-4 · Positive Gowers’ sign. The child gets up by pushing to an upright position, using the hands to climb up the legs to a standing position: The child starts at the ankles, alternating hands; he then gradually pushes to an upright position, using the legs as the climbing pole.
Diagnosis. Duchenne muscular dystrophy is diagnosed by the presence of symptoms, electromyogram, muscle biopsy, and elevated enzyme levels, such as aspartate aminotransferase (ALT, formerly SGOT) and creatine phosphokinase (CK, CPK).
Treatment. There is no cure for any of the forms of muscular dystrophy. Treatment is supportive. Wheelchairs are needed as the child loses the ability to walk. Feeding tubes may be necessary if the child can no longer swallow. As the disease progresses, supportive respiratory therapies, such as ventilators, may prolong life.
Nursing Considerations. Genetic counseling may be helpful for families who have known or suspected histories of muscular dystrophy. Grief counseling should also be considered. The goal is to maintain physical function as long as possible. This disease is devastating, and emotional support must be provided for the child and family. The mother may experience enormous feelings of guilt because she is the carrier of the defective X gene.