Surgical Mask and Eye Protection
In strict sterile situations, such as in the OR or with protective isolation, the mask covers the mouth and nose. The purpose of the mask is to form a barrier to stop the transmission of pathogens. In the OR or during other sterile procedures, the mask prevents harmful microorganisms in your respiratory tract from spreading to the client. When the client has an infection, the mask protects you from his or her pathogens.
Key Concept Remember that the mask is considered contaminated because it touches the nurse’s face. Do not touch the mask with sterile gloves. If the mask becomes wet, it needs to be changed, because it is no longer effective.
Eye protection is often worn in the operating room or in other areas, such as the dental office, Emergency Department, or acute psychiatric services. The nurse’s eyes must be protected from splashing of body fluids.
Sterile Gown
A sterile gown is commonly worn in the OR, with protective isolation, and sometimes in the delivery room. The hands touch only the parts of the sterile gown that will touch the body after the gown is in place. Thus, touch only the inside of the gown. Someone else must tie the strings. The back of the gown is considered contaminated, even though it was sterile when put on. Any part of the gown below waist level and above nipple level is also considered contaminated. When wearing a sterile gown be careful not to touch anything that is nonsterile. If you are required to wear a sterile gown, inservice education must be obtained.
Sterile Gloves
For some procedures, sterile gloves are worn. Practice is required in order to put on sterile gloves without contaminating yourself or anything else in the sterile area. Remember that once gloves are put on, touching anything nonsterile contaminates them. Therefore, make all preparations before putting on sterile gloves.
Key Concept Be sure to keep the hands between the waist and nipple levels whenever sterile gloves are worn. This is true whether or not a sterile gown is worn at the same time.
In Practice: Nursing Procedure 57-2 describes a method of gloving called open gloving. A procedure called closed gloving is often performed when a sterile gown is also used. You will learn that procedure if you work in an operating room, short-stay surgery, or assist with minor surgery in a physician’s clinic.
Key Concept Whenever the cover on a sterile tray or a gown, mask, dressing, drape, or other sterile cloth or paper item becomes wet, it is contaminated.
Removal of Sterile or Nonsterile Gloves
To remove gloves, whether they are sterile or clean, pull one glove down over the other. Place the gloved fingers of your first hand only under the outside cuff of the glove being pulled off (Fig. 57-2A). Rationale: This keeps your hand and arm away from any contamination that might be on the glove.
FIGURE 57-2 · Safe removal of gloves. (A) Touch only the outside of the contaminated glove (inside a folded-down cuff) with gloved fingers. (B) Touch the skin only with bare fingers. Roll gloves together; with contaminated areas inside the roll and discard appropriately. Wash hands carefully
The glove that was pulled off is held in the gloved hand. Then, slide the ungloved fingers of the other hand inside the second glove, pulling it off and over the first glove. This time, put your fingers inside the glove and avoid touching the outside of the gloves with your ungloved fingers. Keep the outsides of the gloves inside the rolled-up gloves (Fig. 57-2B). Rationale: By doing this, if there is contamination on the gloves following a procedure, most of the contamination will be contained within the gloves. Discard gloves in the designated receptacle and carefully wash your hands. Remember: Handwashing is your most important defense against the spread of microorganisms.
PROCEDURES REQUIRING STERILE TECHNIQUE
A number of procedures require the use of sterile equipment and/or sterile technique. Several of these are described elsewhere in this topic. They include:
• Care of the indwelling catheter.
• Surgical intervention and invasive procedures—discussed in this topic
• Sterile dressing change.
• Suture and staple removal.
• Administration of parenteral medications.
• Venipuncture and Management of IVs.
Urinary Catheterization
The bladder is the reservoir for urine. Normally, when about 250 to 300 mL of urine collects in the bladder, the urge to void (urinate) occurs. If the bladder cannot empty normally, it becomes distended (enlarged or stretched out) as urine collects. Urine may dribble from the urethral opening, and chronic kidney disorders can result.
Urinary catheterization is the procedure of inserting a tube (a catheter) through the urethra into the bladder to remove urine. Although urinary catheterization is related to elimination of urine, it is placed in this topic because it is an important sterile procedure. (Other procedures related to elimination of body wastes do not use sterile technique.) Urinary catheterization is performed under sterile conditions to help ensure that foreign microorganisms are not introduced into the bladder. Only disposable sterile equipment is used. A straight catheter is used for one sample only and removed. A retention catheter (e.g., Foley catheter) remains in the bladder. The Foley-type catheter is also called an indwelling catheter. Other types of indwelling catheters are the mushroom, the Malecot, and the Pezzer. A special type of catheter, called a coudé-tip catheter, is used in male catheterization if there is prostate enlargement or in the female if there is abnormal placement of the urinary meatus.
At one time, catheterization was considered necessary to obtain an uncontaminated urine specimen. Today most providers recommend midstream and clean-catch methods of urine collection in nearly all cases.Catheterization may be required to obtain the amount of urine residual after voiding or for certain studies of the urinary system. The need for catheterization after surgery has diminished, because early ambulation for surgical clients has increased (which helps all body systems to return more rapidly to normal functioning).
Generally, no more than 750 to 1,000 mL of urine can be safely removed from the bladder at any one time, particularly if the client has had retention or distention for a long period. If urine flow seems undiminished after withdrawal of this quantity, clamp or remove the catheter and report the findings to the primary care provider. (If there is a clamp on the catheterization drainage setup, close it to clamp the flow of urine. If there is no clamp, you will need to be prepared with a surgical clamp for this purpose.) The procedure for removal of the retention/indwelling catheter is explained later in this topic.
Nursing Alert A client can go into shock if too much urine is removed from the bladder too quickly Check the policy of your facility before performing catheterization, to determine the maximum amount of urine to be removed at one time.
Self-Catheterization
Some clients are taught to catheterize themselves on a regular basis, usually with a straight catheter. This may be done in the paraplegic client or in the client with chronic neurologic bladder atony (lack of muscle tone). In this case, the procedure may continue at home, using clean technique, rather than sterile technique, because the catheter is contaminated only to the client.
Nursing Alert Before performing any catheterization, make sure the client is not allergic to latex. Although catheters today usually are not rubber (latex), the client with a latex allergy could have a severe reaction to another type of catheter A special nonallergenic catheter must be used. If the client’s allergy is severe, specific allergy testing must precede the catheterization.
Catheterizing the Female Client
Placement of a retention catheter may be necessary when a woman has had pelvic surgery or bladder tumors. In Practice: Nursing Procedure 57-3 summarizes steps for catheterizing the female client.
The Side-Lying Position
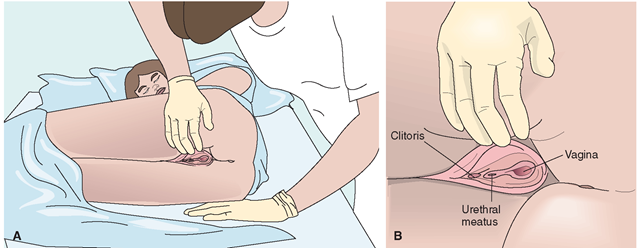
If the client is unable to lie on her back for the procedure or if she cannot relax her legs because of contractures, use the side-lying position for catheterization (Fig. 57-3). Many women are more comfortable in this position than on the back. Some nurses prefer to use this position when catheter-izing all female clients. The side-lying position makes maintaining sterile technique easier because the nurse needs to hold only one side of the labia in position. Contamination of the catheter is less likely because the client maintains this position well, and the nurse does not have to reach over the client’s leg.
The client lies on her side with her knees drawn up to her chest. If the nurse is right-handed, the client should lie on her left side, and vice versa. Remember to raise the level of the bed to a comfortable height for you. The client’s buttocks should be near the side of the bed where you are standing and the client’s shoulders should be near the other side of the bed. Stand behind the client, near her buttocks. Follow the same sterile technique and general steps as those for inserting a catheter for the client lying in the supine position.
FIGURE 57-3 · The side-lying position for female catheterization. Shown here is the position for the left-handed nurse. (A) The client is positioned on her side. After the client is positioned, the nurse must put on sterile gloves (because these gloves were contaminated during positioning). (B) The urinary (urethral) meatus is exposed and the catheter inserted.
Catheterizing the Male Client
Catheterization of the male client may offer additional chal lenges for the nurse because the man’s urethra is longer and more curved. In addition, sometimes an enlarged prostate gland constricts or obstructs the urethra. Previous urethra infection can also cause strictures. In Practice: Nursing Procedure 57-4 describes the steps for male catheterization.
Caring for the Client After Catheterization
After any client is catheterized, reposition the client to ensure that he or she is comfortable and the signal cord is within reach. Be sure that the balloon of an indwelling catheter is inflated and the catheter tubing is secured externally to avoid pulling and discomfort. Use hypoallergenic tape to hold the catheter to the man’s abdomen or thigh or to the woman’s thigh. Explain to the client that he or she may feel the urge to void because of the catheter’s presence in the urethra, particularly within the first 30 minutes of insertion This feeling should diminish and usually goes away within an hour.
Nursing Alert If the client continues to feel a very strong urge to void or severe discomfort after insertion of the catheter, report this to the primary care provider
The drainage tubing extends straight down from the bed level to the bag (straight drainage) with extra tubing placed on the bed with the client, so movement is possible. Rationale: Loops hanging down can promote urinary stasis and infection. If a retention catheter is left in place, attach the drainage apparatus to the bed frame (not the side rails), maintaining its sterility.
Key Concept The drainage bag must always be lower than the clients bladder for the urine to drain properly and to help prevent infection.
Removing the Retention Catheter
Removing a retention catheter is a simple procedure. The balloon is deflated and the catheter is gently pulled out. Take care to prevent urethral trauma. In Practice: Nursing Procedure 57-5 lists actions for removing the retention catheter. In Practice: Educating the Client 57-2 lists important self-care points for the client.
Nursing Alert A catheter is never cut for removal. This could cause the catheter to be pulled back into the urethra or bladder In that case, surgical removal would probably be necessary This would also be a prime source for introducing pathogenic organisms into the urinary bladder
IN PRACTICE EDUCATING THE CLIENT 57-2
AFTER CATHETER REMOVAL
Client education encourages cooperation and lessens anxiety Teach the client to:
• Drink plenty of fluids (to facilitate voiding).
• Report the urge to void for the first time after catheter removal.
• Understand that some discomfort may be felt with the first voiding.
• Report any severe pain or blood in the urine.
KEY POINTS
• Clean applies to medical asepsis. It means the removal of all gross contamination and many microorganisms.
• Sterile means that the item is free of all microorganisms and spores.
• When a sterile item touches anything unsterile, the sterile item becomes contaminated.
• If a sterile item becomes contaminated or if there is uncertainty whether or not it is contaminated, the item is considered contaminated and must be discarded.
• Catheterization is the procedure of inserting a flexible tube through the urethra into the bladder to remove urine. This aseptic procedure requires sterile equipment and technique.
• The balloon is deflated when removing a retention catheter. The catheter is never cut for removal.
• Client and family teaching is vitally important, especially if the client or family will need to perform sterile procedures such as IV therapy or catheter care after discharge.