Other Complications
Infection. A temperature elevation occurring 2 or 3 days after surgery, severe pain, redness or swelling around an incision, or an elevated white blood count (WBC) are usually signs of infection. The nurse should observe for, and teach the client the signs of, infection to prevent complications. Observe the condition of the client’s incision at least every 4 hours and document your findings. Compare the condition of the incision with previous observations. Sterile technique and careful handwashing are important when changing dressings. Wear gloves and carefully dispose of all waste materials according to the agency’s protocol. These activities help to prevent infections and the spreading of existing infections to others.
Key Concept All used dressings are considered grossly contaminated if there is any drainage.They must be disposed of in a red marked biohazard bag, according to agency protocol.
Treatment of infection includes administration of antibiotics, increased fluids, rest, and an adequate diet to build up resistance. If necessary, the wound is drained. In some cases, the wound is cleaned or flushed with a solution (wound irrigation).
A serious situation is the development of an infection caused by an antibiotic-resistant organism. Notable is the methicillin-resistant Staphylococcus aureus (MRSA), which is very difficult to treat because it does not respond to penicillin and related drugs.Other organisms are developing resistance to antibiotics, making it necessary to continue to develop newer, stronger, and more broad-spectrum antibiotics.
Key Concept An infection acquired in the hospital is known as a nosocomial infection. Because most postoperative clients return home soon after surgery it is vital to instruct the client and family about signs and symptoms of an infection. They should be instructed to report any problems immediately
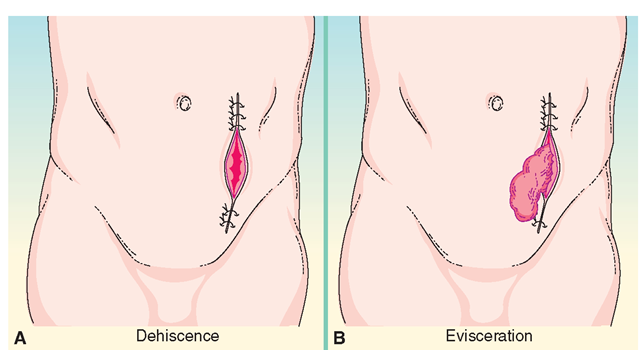
Dehiscence and Evisceration. Dehiscence is the splitting open or separation of the surgical incision. If the incision opens enough so that abdominal organs (viscera) protrude, this is known as evisceration (Fig. 56-8). Clients at risk for evisceration include those with poor wound healing (e.g., diabetic clients), older adults with friable (fragile) skin, morbidly obese individuals, and persons with invasive abdominal cancer or a postoperative infection. Violent coughing, vomiting, or excess movement also can cause dehiscence or evisceration.
Usually, the client describes this sensation by saying “something gave.” The condition is uncommon, but the nurse should be prepared to deal with it. This is an urgent situation. Wear gloves (sterile ones if possible). Cover protruding structures with sterile large abdominal (ABD) pads that have been moistened with sterile normal saline. Report the incident immediately. The greatest dangers from dehiscence and evisceration are infection, intestinal strangulation, and hemorrhage.
Additional Supportive Measures
Providing Adequate Nutrition
The client should return to oral intake of adequate food and fluids as soon as bowel sounds return. Most people who have had uncomplicated surgery can function on IV therapy for a short time, but should resume oral intake as quickly as possible.
Usually, the client starts with a progressive diet to avoid abdominal distention that may occur if peristalsis is sluggish. On the physician’s orders, offer the client a clear liquid diet first. Progress to a full liquid diet, and finally a soft or general diet.Usually, the sooner the client tolerates food, the sooner he or she recovers overall. This progression is often ordered as DAT (diet as tolerated).
Key Concept In many cases, a nutritional drink, such as Boost or Ensure, is given with meals after surgery to supplement solid foods. Many clients find that they are able to drink, even if it is difficult to take solids.
Certain clients require more extensive diet therapy and should be evaluated by a dietitian, in cooperation with the physician. Special attention is needed for clients who are:
• Frail and/or older
• Obese
• Severely underweight
• Diabetic
• Suffering from malabsorption disorders, anorexia nervosa, or bulimia
• Vegan or strict vegetarian (particularly if no eggs or dairy products are used)
FIGURE 56-8 · Serious postoperative complications. (A) Dehiscence is the splitting open or separation of the surgical incision. (B) Evisceration is dehiscence with the protrusion of viscera. Both are emergency situations.
• Diagnosed as having a defect in digestion or absorption
• Running a high fever for any length of time
• Experiencing severe trauma or amputation
• Suffering from a large infection
• Severely burned
• Experiencing extensive drainage from any body orifice or wound
• Suffering from severe diarrhea or constipation
• Unable to resume oral intake within 8 to 10 days
• Vomiting for an extended period
To rebuild tissue after the trauma of surgery, the client requires nutrients in excess of normal body needs. Protein is particularly necessary to rebuild wounded or diseased tissue.
Wound Irrigation
Many clients have wounds that must be irrigated. The healthcare provider will order the type of solution to use and may suggest a particular irrigation method. Otherwise, check the facility’s policies and procedures to determine the method of wound irrigation. In some cases, irrigation follows sterile technique; in others, the procedure is clean.
Dressing Changes
A dressing reinforcement is the application of additional dressing materials to an already existing dressing. A dressing change is removing the dressing entirely and replacing it with a fresh one. Depending on the institution’s policy and the surgeon’s orders, nurses can reinforce a dressing without a specific order. A physician’s order usually is needed to change a dressing. Use aseptic (sterile) technique and always follow Standard Precautions when changing dressings.
Key Concept The surgeon usually does the first postoperative dressing change, so the wound can be carefully inspected. After that, there may be an order for nurses to perform this task.
Suture and Staple Removal
Sometimes, there is an order for the nurse to remove sutures (stitches) or staples. This is more common in the physician’s clinic than in the hospital. In many cases, the nurse will assist with this procedure.
In assisting with or performing suture removal, a disposable suture removal kit is used. Sutures are readily removed. Sterile scissors are used to cut the suture, and sterile tweezers are used to pull out the thread. It is important to pull on the side next to the knot. Rationale: Pull on the side next to the knot, to prevent pulling the knot through the wound. This might rip open the suture line and would be more painful. Often, sterile adhesive skin closures (Steri-Strips) are applied after sutures are removed, to reinforce wound healing. A dressing may be applied after suture removal, but often, the wound heals faster if exposed to the air. Staples are used frequently to close surgical incisions because they are inert, do not cause infection, and are quickly inserted. A special staple remover is required to remove staples.
IV Therapy
Most clients leave the operating room with an IV infusion running. Several types of IV solutions are commonly used. These include dextrose 5% and water (D5W) and dextrose 5% and normal saline (D5NS). Normal saline is identified as 0.9% sodium chloride, NaCl, and is considered to be iso-tonic—of the same concentration as the fluids surrounding normal body cells. Another commonly used solution is dextrose 5% in half-normal saline (D5 /2NS—0.45% NaCl). Often, antibiotics and other medications and/or several electrolytes are added to the IV. In most cases, the IV will be regulated by an electronic pump or controller.
It is important for the nurse to know the techniques necessary when giving daily care, ambulating the client, and positioning the client who has an IV in place. It is important to recognize when the IV line has infiltrated (moved out of the vein) and to know how to discontinue it safely. Observe and monitor the infusion site at least once per hour and make sure the infusion is running. The IV fluid infused is recorded as part of the client’s total I&O.
Venous Access Lock. Almost all clients will have an IV in place during surgery. Some clients will return to the nursing unit with a saline lock (venous access lock) in place. In this case, fluids and medications can be given via the lock. They may be given with a needle and syringe, a needleless system, or by using an IV bag and tubing. In this case, the tubing is disconnected and the lock remains in place so that it is available to be used again without restarting the IV. The venous access lock is often used postoperatively to administer antibiotics.
Most facilities require venous access locks to be flushed one to three times per day, to keep them patent (open). The solution most often used to flush the venous access lock is sterile normal saline, although heparin may also be ordered. Removal or discontinuance of the venous access lock is the same as for an IV.
Key Concept The client who is having surgery needs both physical preparation and kind and gentle emotional support. The nurse is in a unique position to provide that support. Remember that the client’s family caregivers are vital members of the healthcare team because they will be assisting the client when he or she goes home. They need careful instruction and support because the client will be doing most of the recuperation at home.
KEY POINTS
• Preoperative teaching is the first line of defense against postoperative complications. Teaching also helps clients to feel more at ease during this stressful time.
• Surgery may need to be cancelled if the client has a cold or other illness, or if the client is extremely apprehensive.
• Before giving any pre- or postoperative medication, always check the client for drug and/or latex allergies.
• All permits must be signed before any preoperative medications are given.
• Use of narcotics and sedatives can cause serious side effects. Watch carefully for these side effects, especially respiratory depression.
• Early postoperative complications include hemorrhage, hypotension and shock, hypoxia and hypoxemia, hypothermia, and neurologic complications. Be alert for early indications of these complications and respond to them quickly.
• Postoperative discomforts may include pain, thirst, abdominal distention, nausea, urinary retention, constipation, restlessness, and sleeplessness. Try to anticipate client needs and take appropriate steps to prevent or alleviate these discomforts.
• Other later postoperative complications include circulatory complications, such as thrombophlebitis and/or DVT, infection, and dehiscence or evisceration. The nurse must report signs of any of these complications immediately.
• Pulmonary hygiene is extremely important in the prevention of later postoperative respiratory complications.
• Early postoperative mobility helps to decrease the possibility of respiratory or circulatory complications.