Learning Objectives
1. State at least five therapeutic reasons for giving mouth care to a client.
2. In the skills laboratory, demonstrate assisting a client with oral care. Demonstrate cleaning and caring for dentures.
3. Identify the steps involved in routine eye and ear care.
4. Demonstrate caring for the client’s fingernails and toenails, addressing the therapeutic reasons for attention to each area.
5. Describe how to assist clients to shave with an electric shaver and with a blade razor.
6. List at least three reasons for performing routine hair care and describe hair care for dry, damaged, or very curly hair.
7. Describe and demonstrate giving a backrub, hand and foot massage, and foot soak.
8. State three types of cleansing baths and when each one is used. Demonstrate how to assist a client safely with each.
9. Describe reasons for careful assessment of the client’s skin on admission and frequently thereafter.
|
IMPORTANT TERMINOLOGY |
||
|
dental caries |
pediculosis |
smegma |
|
friable |
perineal care |
sordes |
|
halitosis |
periodontitis |
|
|
nits |
pyorrhea |
|
Feeling clean contributes to people’s sense of well-being, comfort, and dignity, particularly those who are ill. This topic describes how to assist clients to meet this need when they cannot do it alone.
MOUTH CARE
Frequent mouth care benefits everyone, but it is particularly beneficial to the ill person for several reasons:
• Many disease-causing organisms enter the body through the mouth.
• Food particles lodged between the teeth cause decay, breath odor (halitosis), and inflammation of the tooth sockets (pyorrhea, periodontitis). (Untreated, pyorrhea can spread to the bone and cause loss of teeth.)
• Some illnesses cause irritation, dryness, or brownish deposits (sordes) on the tongue and the mouth’s mucous membrane.
• Mouth-breathing also causes dryness and irritation.
• Some gum infections can be transmitted from one person to another.
• A mouth condition may lessen a person’s appetite and lead to nutritional deficiencies.
• Some oral conditions cause infection or pain locally or in other areas of the body.
• Breath odors or decayed teeth make people self-conscious and are often offensive to others.
Some people may not have learned good oral health habits. Therefore, teaching the client about good oral hygiene is key. The client who learns to perform good oral hygiene in the healthcare facility may continue to do so at home. Remind the client that practicing good oral hygiene is beneficial because:
• Appearance improves.
• Appetite improves and food tastes better.
• Healthy teeth and gums improve overall health.
• Discomfort is avoided.
Offer the client the opportunity to brush his or her teeth before and after each meal and in the evening. When caring for the client’s mouth, observe the condition of the gums, tongue, mucous membranes, and teeth. Record the effects of brushing. Note on the health record any factors, such as missing teeth, unusual tenderness, sensitivity to hot or cold, pain, bleeding, unusual redness, swelling, or odor. If the gums or teeth are unusually sensitive to touch or temperature changes, use “toothettes,” applicators, or a tongue depressor wrapped in gauze, rather than a toothbrush, for oral hygiene. While assisting the client, teach and encourage future self-care. In Practice: Nursing Procedure 50-1 explains how to assist the client in routine mouth care.
Key Concept If brushing the teeth is impossible, encourage the client to rinse the mouth with water or mouthwash after eating.
Flossing the Teeth
It is important to floss between the teeth, to promote healthy gums. Flossing also removes debris that could cause tooth decay (dental caries) and offensive breath odor. If the client is not able to floss the teeth, the nurse can perform the procedure (see In Practice: Nursing Procedure 50-2).
Nursing Alert It is important to make sure the client will cooperate with flossing the teeth before putting your fingers near the client’s mouth. You could be seriously injured if the client bites down.
The Client Who Wears Dentures
Ask the client on admission to the healthcare facility if he or she wears dentures (false teeth) or has a removable bridge or retainer. The presence of dentures or removable appliances should be recorded on the client’s chart. The client who wears dentures needs the same mouth care as the client who has natural teeth. Specially designed brushes and preparations for soaking dentures are available to remove deposits. Brush dentures in the same manner as natural teeth. Be sure to rinse them because the denture cleaner may have a disagreeable taste. See In Practice: Nursing Care Guidelines 50-1 for more on caring for a client who wears dentures.
Be alert for a client who constantly removes his or her dentures. Question the client about any possible reasons why he or she is removing them. Also, inspect the client’s mouth, looking for any irritation or redness that may suggest a problem. For example, the dentures may fit poorly or may cause pain, which may also be the reason for bad eating habits and poor nutrition. Be particularly observant of the client who is experiencing confusion.
IN PRACTICE :NURSING CARE GUIDELINES 50-1
CARING FOR A CLIENT WHO WEARS DENTURES OR OTHER MOUTH APPLIANCES
It is vital to document the presence of any removable teeth or dental appliances the client is wearing. This includes dentures, removable bridges, retainers, bite guards, or nighttime appliances to whiten the teeth or prevent grinding of the teeth. Some facilities require that removable oral appliances be removed from all persons who are unconscious, intubated, or being suctioned orally Rationale: These items could be aspirated during surgery or other treatments, such as electroconvulsive shock therapy (ECT) or colonoscopy. In addition, insertion of an endotracheal tube could break an oral appliance or dislodge a tooth. Any of these situations could cause serious complications, such as aspiration into the lungs. Death could result.
Most dentists encourage their clients to wear their dentures all the time. Rationale: If clients remove dentures for long periods, their gum lines change and their dentures will no longer fit.
If the client must remove dentures, they should never be stored in cups or glasses that are used for drinking. Rationale: The client may accidentally swallow the dentures. This could cause choking or aspiration.
Store all dentures and mouth appliances in specially marked opaque "denture cups." These containers and their lids must be clearly marked with the client’s name and other pertinent information. Store dentures out of sight. Rationale: It is vital not to lose or mix up these items. The client may change rooms, but the facility ID number stays the same. Clients may be embarrassed and not want others to see their dentures.
While dentures are being stored, they usually are kept in water Ask the client who has some other type of appliance if fluid is required for storage. Rationale: Dentures usually must be kept moist to preserve their fit and general quality.
Take extra precautions to ensure that dentures or other oral appliances do not get lost. Be sure to check the client’s food tray after meals and linens when the bed is changed. Rationale: Some clients remove dentures. They are expensive and may be very difficult for the client to replace.
Respect the client’s privacy when cleaning his or her dentures. Wash your hands before and after handling dentures and wear gloves. Handle dentures carefully; they are slippery, fragile, and expensive. To avoid breakage, place a folded washcloth in the bottom of a basin of water or sink, holding the dentures over it. Do not hold them over a hard surface. In Practice: Nursing Procedure 50-3 reviews the general steps associated with denture care. The care of other dental appliances is usually similar to that of dentures.
Nursing Alert Remove dentures if a client is unresponsive, out of control, having frequent seizures, or going to have surgery If dentures are removed, document that fact, label them carefully and store them safely
Special Mouth Care: The Dependent Client
In certain situations, clients need assistance with mouth care or require special care. For example, sordes that has collected on the tongue and teeth because of illness must be removed. In addition, special mouth care may be needed for clients who:
• Breathe through the mouth
• Are receiving supplemental oxygen or mechanical ventilation
• Are unable to take fluids by mouth or have fluids restricted
• Need to be encouraged to take food (cleansing the mouth before meals makes food more palatable)
• Are unresponsive or paralyzed
• Are very young, confused, or otherwise unable to perform independent mouth care.
Oral cleansing sometimes removes secretions and thus helps to prevent choking. In such cases, mouth care is performed frequently. For the client who is unresponsive and breathing through the mouth, for example, oral hygiene is often ordered every hour because of the extreme dryness. (Some medications may also cause dry mouth and require the client to receive frequent oral care.) Exact procedures may differ among agencies. A basic procedure is given at In Practice: Nursing Procedure 50-4.
The mouth of a client who is unresponsive may become dry and cracked, creating a portal for harmful microorganisms to enter. Keeping the mouth moist and intact is an important nursing action to prevent infection. Move the client into a side-lying position, with the head of the bed lowered, as tolerated. The client’s head may also be turned to the side. Rationale: In this position, gravity causes saliva to run out of the mouth and prevents the client from choking. This position also allows for the client to be suctioned (see Nursing Procedure 86-1 and Nursing Procedure 87-6). While giving oral hygiene, inspect the gums and the mucosa of the mouth. Also inspect the lips for dryness and cracking. Apply petroleum jelly (Vaseline) or other ointment as ordered.
Key Concept Be gentle when giving mouth care; the oral mucosa is fragile and may be injured if mouth care is performed too vigorously Also be sure to prevent aspiration in clients who are unable to swallow or spit out solutions. Use only a minimum of solution and make sure it is completely suctioned or drained out of the client’s mouth.
Extreme caution is required if giving mouth care to a client who has had oral surgery The procedures to be used depend on the type of surgery that has been done. If there is any question about procedures to use, consult the healthcare provider or team leader
NCLEX Alert Be alert to the reasons for pro viding basic care to the client or assisting the client with personal hygiene, such as inspection for infection, providing comfort measures, identifying adaptive devices (dentures, hearing aids, as examples) and providing the nurse with opportunities for skin evaluation. This information may be integrated into the NCLEX exam.
ROUTINE EYE CARE
Normally, tears are produced by the lacrimal glands, which are situated at the top and outer portion of each eye. Tears help protect the eyes from bacteria, viruses, and other foreign matter, and lubricate the eyes. With blinking, tears are washed across the eye and toward the lacrimal ducts located at the inner canthus of the eye.Tears continually drain into the lacrimal ducts, which in turn drain into the nasopharynx. (This is why you get a runny nose when crying.) If a client has decreased tear production, does not blink, or has blocked lacrimal ducts, eye problems can occur. Infections may be caused by an accumulation of dried secretions on eyelids and eyelashes. Eye care should be done to remove secretions by applying a cotton ball or gauze square moistened with sterile water or normal saline to the eyelids. Some clients also will need supplemental moisture in the form of eye drops, as ordered. In Practice: Nursing Care Guidelines 50-2 describes routine eye care.
IN PRACTICE: NURSING CARE GUIDELINES 50-2
CARING FOR THE EYES
• Wash your hands and put on gloves. Rationale: Handwashing and gloving help to prevent the spread of infection.
• Soak cotton balls or gauze squares in sterile water or normal saline solution. If eye care is being given as part of the bath and no infection is present, a clean washcloth may be used. Wash the eye area before washing any other part of the body, Rationale: It is important to avoid introducing harmful microorganisms into the sensitive eye tissues.
• Wipe the client’s eyelid from the inner (next to nose) to the outer canthus. Rationale: Proper wiping technique moves debris away from the eye, prevents reinfection or contamination of the eye, and protects the tear ducts.
Wipe from inner canthus outward, using a separate part of the cloth for each eye.
NURSING CARE GUIDELINES 50-2 continued
• Repeat steps on the other eye, using clean supplies. Rationale: It is important to use separate supplies for each eye. This helps prevent spreading infection between eyes.
The Client Who Wears Contact Lenses
• Determine the type of contact lenses the client wears and the client’s usual cleaning practices. Rationale: Different types of lenses require differing cleaning and storage techniques. Some contact lenses are disposable.
• Encourage the client or a family member to remove the lenses and place them in cleansing or soaking solution. (Sterile normal saline can be substituted for lens soaking solution in an emergency) Rationale: It is important that hard or semipermeable lenses do not dry out. Proper storage is necessary to maintain the integrity of the lenses.
• Be sure to label separate containers for each eye and include the client’s name and facility identification number Rationale: Contacts have a separate prescription for each eye and can be easily switched. In some cases, a small dot indicates the right eye. The containers must be labeled carefully to prevent loss.
• Notify the team leader if the client is unable to remove the lenses by himself or herself. Rationale: A suction cup or other device is available for removal of contact lenses. This must be used by a specially trained person.
• If lenses cannot be removed, notify the primary healthcare provider Rationale: Corneal damage may result if the client wears some types of contact lenses for too long a period of time, particularly if the client’s eyes are dry or if he or she cannot blink.
Special Eye Care for the Client Who Cannot Blink
• Follow the steps for routine cleaning of the eyes.
• Instill lubricating drops in the eyes or ointment onto the lower lids as ordered by the primary healthcare provider. Rationale: Drops or ointment help to keep eyes moist.
• Close the client’s eyelids. If allowed by the agency cover the eye with a sterile eye pad and secure with paper tape. (This procedure may vary among clinical agencies; check the standards for care in your agency) Rationale: These procedures help to maintain available moisture in the eye and help prevent corneal abrasions.
• Document all procedures on the client’s record. Rationale: Documentation provides communication and coordination of care.
EAR CARE
A client’s external ears are washed routinely during the bed bath. If excessive cerumen (ear wax) is present, a special procedure may be necessary to remove it to prevent hearing difficulty. (Wax removal is usually done by irrigating the ear’s outer canal with warm water. This procedure must be ordered by the physician or advanced practice nurse. Special training is needed to perform this procedure.)
Nursing Alert Warn clients never to insert objects, such as cotton swabs (Q-Tips), toothpicks, or matches, into their ears to clean them. RATIONALE: These objects can injure the ear canal, puncture the eardrum, or push earwax further into the ear canal, making removal more difficult.
Care of a Hearing Aid
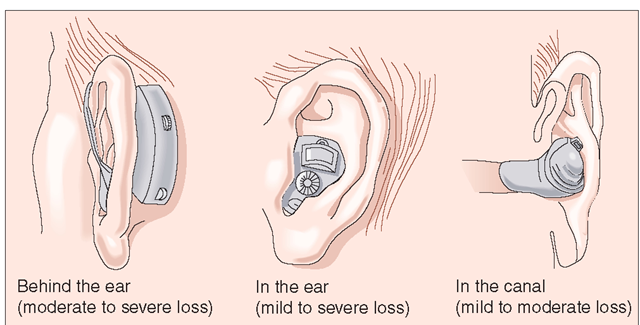
Clients who have a hearing impairment may use a hearing aid. A hearing aid is a battery-operated, sound-amplifying device that consists of an earpiece that fits into the ear canal and a power source. Hearing aids may be very small and may fit entirely into the outer ear (Fig. 50-1). They may also have a piece that fits behind the outer ear or may require a separate battery that is carried in a pocket and connected to the device by a cord or a wireless system.
FIGURE 50-1 · Several types of hearing aids. The general care and use are approximately the same for each.
The size of the device depends in part on the type of hearing loss that exists. Some types of hearing aids have a part of the device implanted within the person’s body and a part worn externally. One example is a cochlear implant.In Practice: Nursing Care Guidelines 50-3 provides information about caring for a hearing aid.
IN PRACTICE :NURSING CARE GUIDELINES 50-3
CARING FOR A HEARING AID
• Clean the earpiece regularly with saline or the prescribed solution (to prevent cerumen buildup). Do not clean with alcohol. Rationale: Alcohol may damage the delicate parts of the hearing aid. It may also be irritating to the client’s ear canal.
• Check and replace batteries regularly Teach the client to have spare batteries on hand at all times.
• Adjust the volume to meet the individual’s needs.
• Turn off the aid when the client is not using it, to preserve the life of the battery
• Remove batteries if the client will not use the aid for an extended period.
• If a hearing aid is removed from the client’s ear, place it in a plastic bag or other receptacle and carefully label it with the client’s name and other pertinent information. Store the device in a safe place. Be sure it is specified on the client’s property list.
• Avoid exposing the aid to heat and moisture.
• Turn the volume down completely before inserting the aid into the client’s ear.
• Evaluate client complaints about the hearing aid or repeated removal or refusal to use the aid.
Key Concept If a hearing aid is working properly and fits properly the client usually will be willing to wear it. Refusal to use a hearing aid or repeated removal of the aid usually indicates discomfort or malfunction of the device.
Nursing Alert Client Education It is important to teach clients and their families how to care for the teeth, mouth, eyes, and ears. They will be required to carry out this care when the client returns home.
NCLEX Alert Be alert to the examples of client/family teaching regarding hygiene, especially skin care; as clients transfer to a home setting, family members will have to assist the client in self-care and inspection for skin breakdown. Exam scenarios may include this information and you may need to select your response based on your understanding of your role in client/family teaching.