Prostate Surgery
Preoperative Nursing Considerations. As part of the preoperative preparation for a radical prostatectomy, alert the client to the strong possibility of postoperative erectile dysfunction. About 90% of men are impotent after surgery, except those who have the nerve-sparing procedure. Depending on the client’s age, the impotence rate with nerve sparing is only about 30%; younger men are less likely to become impotent. Because 80% of prostate cancers are androgen (e.g. testosterone) dependent, a treatment goal will also be to decrease circulating androgens, which further affect the man’s ability to achieve an erection.
Encourage the client who wishes to have children to consider sperm banking before the surgery. Review the types of available treatment options for erectile dysfunction and how they work.
Discuss the possibility that the client will have a suprapubic cystoscopy catheter and some sort of continuous bladder irrigation for approximately 2 to 3 days after surgery.
Before the prostatectomy, the client may have a catheter inserted for continuous urinary drainage to prevent accumulation of stagnant urine in the bladder. Give him plenty of fluids, with proper diet and rest. Antibiotics are often given prophylactically.
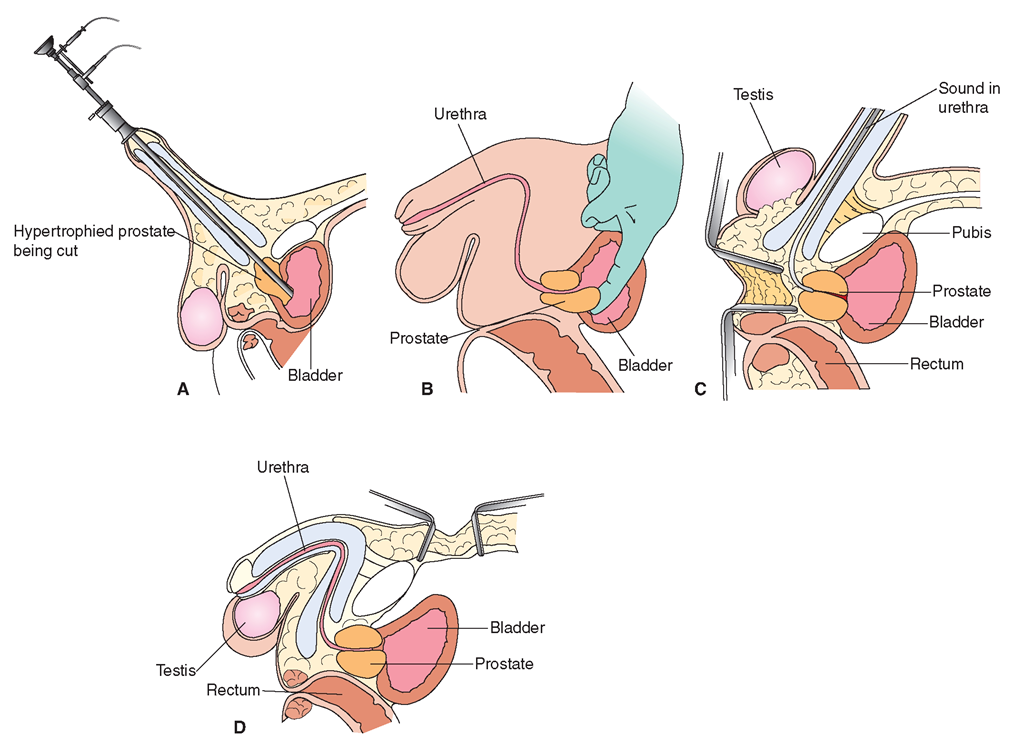
Transurethral Resection of the Prostate (TURP). This is the most common procedure, particularly for older men or those who are a poor surgical risk. Figure 90-3 illustrates common techniques. In TURP, the surgeon removes prostate tissue through the urethra by means of a resectoscope, which has a cutting edge or electric wire that slices the prostate away bit by bit (Fig. 90-3A). Because the surgeon does the operation through the urethra, no incision is necessary. Recovery after TURP is shorter than after other approaches. Complications of TURP include hemorrhage, urinary retention, stress incontinence, and erectile dysfunction.
Prostatectomy. Another surgical treatment for prostatic cancer (and also BPH) is removal of the excess or abnormal prostate tissue (prostatectomy) through various approaches. The surgeon can dissect the prostate through an incision through the bladder (suprapubic prostatectomy or suprapubic resection), a perineal incision (perineal prostatectomy or perineal resection), or an incision below the bladder (retropubic prostatectomy). Dissection is also possible using a cystoscope (resectoscope) through the urethra.
Suprapubic Prostatectomy: The surgeon usually performs the suprapubic procedure if the client’s gland is greatly enlarged (>100 g). Surgery may be done in two stages. First, the surgeon performs a cystostomy (incision into the bladder) to relieve urinary retention; second, he or she removes the prostate tissue (Fig. 90-3B). After the two-stage suprapubic operation, the client returns with two indwelling catheters in place, one in the urethra and the other in the suprapubic wound (a suprapubic Cystocath). These catheters are attached to separate drainage containers, allowing for more accurate output measurement. The urethral catheter is attached to a closed drainage system, and the wound catheter is attached to an irrigation apparatus. (The surgeon may prefer that any bladder irrigation be done through the urethral catheter.)
Perineal Prostatectomy: If the surgeon removes gland tissue through an incision in the perineum, catheter drainage is through the perineal incision only (Fig. 90-3C). In this case, the client will find sitting up to be difficult. Fecal contamination of the incision may occur because of its location. Nerve-Sparing Radical Prostatectomy (Retropubic Prostatectomy): Nerve-sparing radical prostatectomy removes the prostate through an incision below the umbilicus and above the symphysis pubis (Fig. 90-3D). This procedure causes less erectile dysfunction, incontinence, and bleeding than do other methods.
Radical Prostatectomy: A radical prostatectomy (removal of the prostate gland, seminal vesicles, and part of the urethra) sometimes cures prostatic cancer that has not metastasized. A radical prostatectomy is an open procedure because an abdominal incision is necessary. Complications of radical prostatectomy include stress incontinence, epididymitis, urethral stricture, fistula, and erectile dysfunction.
Cryosurgery. A less-invasive procedure used to remove prostatic cancer is cryosurgery. An incision is made in the perineum and a special tool is inserted to the area of the prostate cancer to freeze the tissue. This procedure is believed to kill the cancer. The risks involved in cryosurgery are similar to those for other prostate-removal procedures. The success of the procedure is still under investigation.
Postoperative Nursing Considerations. The client will require routine postoperative care, such as antiembolism stockings, early ambulation, and incentive spirometry (see In Practice: Nursing Care Plan 90-1). Encourage fluid intake and monitor intake and output. Give stool softeners, as ordered. Help the client and his partner deal with any psychological and emotional problems. In Practice: Educating the Client 90-1 provides pertinent instructions for discharge and home care.
FIGURE 90-3 · Types of prostatectomy. (A) In a transurethral resection of the prostate (TURP),the surgeon connects a wire to a loop of current that is rotated in a cystoscope to remove shavings of the prostate. (B) In suprapubic prostatectomy, the surgeon enters through the client’s abdomen, and uses his or her fingers to shell out the prostate. (C) In perineal prostatectomy, the surgeon uses retractors to view the prostate. (D) In retropubic prostatectomy, the surgeon makes a low abdominal incision and, working behind the pubic bone, removes the prostate.
A urethral catheter is left in place for about 2 weeks after a radical prostatectomy. The catheter helps put pressure on the vesicoureteral (bladder and ureter) incision to control bleeding. Keep the catheter straight to avoid obstruction of urine flow. Accidental catheter removal may require the client to return to surgery for its reinsertion.
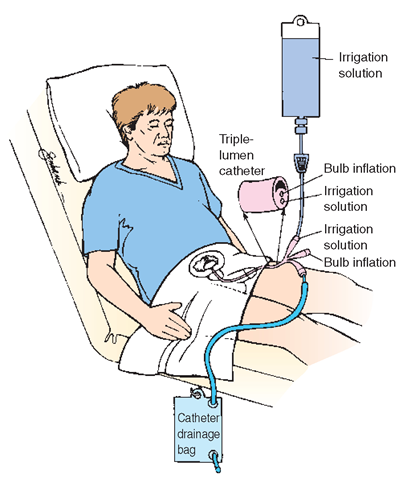
After TURP, the client will return from the Operating Room with a bladder irrigation in place. (This procedure may also be used after other genitourinary procedures.) The surgeon inserts a triple-lumen catheter (with three separate tubes or openings) immediately after the prostate is removed in the Operating Room. One lumen inflates the balloon that holds the catheter in place, whereas a second lumen drains the bladder into a drainage bag (similar to a Foley catheter). The third lumen is used to instill a bladder solution that irrigates the bladder.
Irrigation may be continuous to intermittent after surgery. Continuous irrigation washes out blood before it can form clots; intermittent irrigation washes out clots that plug the catheter. When the catheter becomes clogged, overdistention of the bladder may cause the client great discomfort. In many cases, a pump or controller regulates the flow of irrigant. Figure 90-4 illustrates TURP irrigation, which is used after the procedure. In Practice: Nursing Care Guidelines 90-1 provides information related to TURP irrigation.
Nursing Alert When caring for a client with a continuous TURP bladder irrigation, shut off the irrigation if
• The client complains of bladder fullness, urinary urgency, or bladder or flank pain.
• Drainage from the TURP tube stops.
Check to see if an order exists for a manual irrigation.
Carefully monitor intake and output in the immediate postoperative period. Pay particular attention to the color of the draining urine. The postoperative client will have bloody drainage, which should steadily decrease. Because hemorrhage is a major postoperative complication, report and document any sudden increase of blood in the drainage. If urinary flow slows or stops, the catheter may require irrigation to
IN PRACTICE :NURSING CARE PLAN 90-1
THE CLIENT WITH ERECTILE DYSFUNCTION FOLLOWING A RADICAL PROSTATECTOMY
Medical History: F.O., a 63-year-old married man who presented with urinary hesitancy and straining, decrease in size and force of stream and frequency, and nocturia was diagnosed with prostate cancer. A radical prostatectomy was performed about 8 to 9 months ago. The client comes to the healthcare provider’s office for an evaluation. During the history the client reports that he is having difficulty experiencing erections.
Medical Diagnosis: Erectile dysfunction; post-radical prostatectomy for prostate cancer
DATA COLLECTION/NURSING OBSERVATION
Client is a well-nourished male accompanied by his wife. Client expressing concerns regarding his sexual inability in relation to his marriage and fears of the cancer recurring. Upset with eyes visibly tearing, the client stated, "My wife and I have always been very close, both physically and emotionally It’s so frustrating for me; I’m not a man anymore. I feel like such a failure.” (Although other nursing diagnoses may be appropriate, a priority nursing diagnosis is addressed below.)
NURSING DIAGNOSIS
Situational low self-esteem related to effects of surgery as evidenced by client’s statements of being a failure and not being a man.
PLANNING
Short-term Goals
1. Client will verbalize positive statements about himself.
2. Couple will identify impact of erectile dysfunction on their relationship.
3. Couple will identify measures to cope with erectile dysfunction. Long-term Goals
4. Couple will participate in plan to manage erectile dysfunction, ultimately achieving satisfaction with method chosen.
IMPLEMENTATION
Nursing Action
Encourage the client to verbalize his concerns and sexual needs— listen to his comments about the situation and what it means for him. Have him describe himself, noting how he sees and how he believes others see options. Be aware of the client’s self-concept in relation to cultural or social values. Rationale: Verbalization allows client to express his feelings openly, helping to provide a clear indication of the client’s perception of himself and his problem.
Nursing Action
If client is agreeable, engage client’s wife in the discussion, allowing her to verbalize her concerns, feelings, and beliefs about the situation. Correct or clarify any misconceptions or inaccuracies. Rationale: Allowing the wife to participate fosters a sense of cooperation between the husband and wife. Clarifying aids in learning and strengthening understanding.
EVALUATION
Client able to state that he is a good provider and supportive person. Wife reinforced these statements. Client and wife beginning to discuss effect of erectile dysfunction on their life and relationship. Goal 1 met; progress to meeting Goal 2.
Nursing Action
Allow the client to go through the grieving process; be open and receptive to behavior changes during this time. Expect some expression of negative feelings. Rationale: Each client grieves in his own way and time.
Nursing Action
Recognize behaviors indicating over concern with the body and its processes. Assist with setting appropriate limits and in helping the client learn how to deal with his feelings and release his emotions in a positive manner. Rationale: Limits provide structure and direction.
Nursing Action
Observe the interactions between the client and his wife. Encourage continuation of open communication of their feelings with each other. Rationale: Open, effective communication is necessary for a good relationship.
EVALUATION
Client and wife openly discussing feelings. Wife offering positive support to client. Client verbalizing desire to learn about options for treating dysfunction. Goal 2 met; progress to meeting Goal 3.
Nursing Action
Ask the client and his wife to restate their knowledge regarding options for erectile dysfunction. Help them obtain information regarding coping strategies. Provide information at their level of acceptance. Rationale: Determining the couple’s knowledge level is important in developing appropriate teaching strategies. Adequate knowledge and understanding are necessary for the couple to make informed decisions about what alternatives are best for them. Providing information at their level helps to prevent them from becoming overwhelmed.
Nursing Action
Provide client and wife with educational material on various options for erectile dysfunction; contact surgeon for possible referral to a healthcare provider specializing in treatment of erectile dysfunction.
Rationale: Providing the couple with material about available options enhances their understanding and promotes informed decision making. Contacting a healthcare provider for a referral helps the couple to follow through with decision making.
EVALUATION
Client and wife are observed reading pamphlets on options available; client has an appointment in 2 weeks with a healthcare provider who specializes in the treatment of erectile dysfunction. Goal 3 met; progress to meeting Goal 4. remove obstructing tissue or clots. If the drainage becomes bright red with gushes of fresh bleeding, report to the charge nurse immediately.
After catheter removal, clients usually are incontinent until they are able to train their external urethral sphincter to do the work of both the internal and external sphincters.
Assist in sphincter retraining by instructing the client in Kegel exercises.
Sitz baths are usually ordered after a perineal prostatectomy. After a bowel movement, take care to avoid contaminating the wound. Use meticulous aseptic technique to cleanse the perineum.
IN PRACTICE :EDUCATING THE CLIENT 90-1
AT HOME AFTER PROSTATECTOMY
Priorities for Home Care
• Review discharge instructions with the client.
• Have client demonstrate measures for catheter maintenance, including cleaning and changing of equipment per instructions.
• Explain bowel maintenance program, including use of stool softeners.
• Encourage ambulation.
• Encourage fluids.
• Demonstrate wound cleaning and dressing changes and have client return-demonstrate procedure using clean technique and sterile dressing as appropriate.
• Teach client about bladder retraining and Kegel exercises.
• Assist client with setting up necessary follow-up appointments, including postoperative appointments, appointments for evaluation and treatment of erectile dysfunction (ED), when necessary, and appointments for counseling, when necessary.
• Assist client and his significant others to understand that depression is common. Often the client will benefit from psychological counseling because the reality of cancer, loss of sterility, loss of sexual function, and/or incontinence are very real and lifetime changes.
IN PRACTICE: NURSING CARE GUIDELINES 90-1
MANAGING CONTINUOUS TURP OR BLADDER IRRIGATION
• Record the amount of irrigating solution instilled into the bladder and the total output. Rationale: An accurate record of the client’s actual urinary output is needed. Subtract the amount of irrigation solution from the total output to determine urine volume.
• Carefully monitor the transurethral resection of the prostate (TURP) setup to make sure all the tubes are open and that they are not twisted or kinked. Rationale: The tubing needs to remain patent and drain freely to prevent overdistention of the bladder.
• Because many men who have TURPs are older and may become confused, make sure clients do not pull on the catheters or change rates of flow of the solutions. Catheters must remain taped in place. Rationale: Damage may occur to the operative site.
• Often, the surgeon orders that traction be placed on the penis, which is kept taped securely in place on the hip or abdomen and is not allowed to hang down. Rationale: Traction facilitates drainage and prevents clotting, but may be uncomfortable.
• It may be necessary to irrigate the catheter manually Be sure the physician surgeon has written an order There is often a standing order to irrigate the catheter as needed. Rationale: Manual irrigation helps to dislodge any clots that may be obstructing the catheter.
• Take special note if the client complains of a feeling of fullness, urgency or bladder or flank pain, or if the drainage stops flowing from the tube. In any of these situations, shut off the continuous irrigation and notify the team leader or physician surgeon immediately Rationale: The client is at risk for hemorrhage.
FIGURE 90-4 · Three-way bladder irrigation used after prostate or bladder surgery
A wound catheter may be in place following radial prostatectomy. Some urine will dribble onto dressings after removal of the wound catheter. Keep the skin clean and dry by frequent dressing changes. The wound may take a month or more to heal.
Painful bladder spasms are common after a client has had prostate surgery. Antispasmodics are administered to control this pain. Relief for incisional pain is also needed, but aspirin is avoided because of its anticoagulation effects.