THYROID GLAND DISORDERS
The thyroid gland secretes the hormones thyroxine (T4) and triiodothyronine (T3), which regulate metabolism by stimulating catabolism (the breakdown of cells and foods, with release of energy). Too much of these hormones makes tissues burn oxygen rapidly; too little causes the reverse. The thyroid gland requires iodine to produce these hormones. Thyroid-stimulating hormone from the anterior pituitary gland influences the secretion of T3 and T4. In addition, the thyroid gland produces calcitonin, which helps to maintain calcium balance in the plasma (see Tables 79-1 and 79-2).
Hyperthyroidism
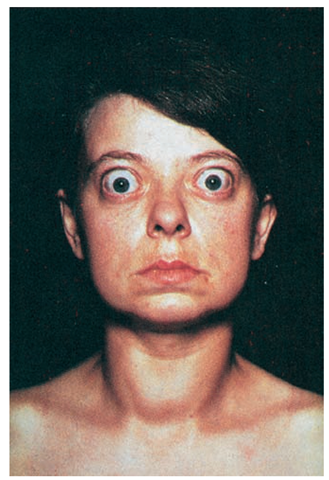
Hyperthyroidism involves the overproduction of T4, which leads to an increase in metabolic rate. Graves’ disease or exophthalmic or toxic diffuse goiter (enlargement of the thyroid gland) is the most common type of hyperthyroidism (Fig. 79-1). The exact cause of this overactivity is unknown, but it may result from infection, physical or emotional strain, or changes related to puberty or pregnancy. Current theories point to an autoimmune origin, in which the person forms antibodies against thyroid cells, specifically the TSH receptor cells. Hyperthyroidism occurs most frequently in women.
Signs and Symptoms
The client is highly excitable and overactive and may have tremors that make eating impossible without help. The pulse is rapid; the person may have heart palpitations and an increased incidence of arrhythmias, which will cause damage if left untreated. The systolic blood pressure is elevated. The person feels hot, and eats voraciously—yet loses weight—because he or she burns calories so rapidly. The skin takes on a characteristic salmon color. In women, menstruation may cease.
FIGURE 79-1 · A woman with Graves’ disease. Note the exophthalmos and enlarged thyroid gland.
Another common symptom is bulging eyes (exophthalmos). The cause of this symptom is not fully understood. It can lead to blindness caused by stretching of the optic nerve or corneal ulceration. The neck is swollen, and pressure from the thyroid gland may cause hoarseness or difficulty swallowing.
If untreated, this disorder may cause intense nervousness, delirium, and finally death as a result of persistent cardiac overload.
Treatment
Treatment for hyperthyroidism may be medical or surgical. Medical treatment consists of prescribing antithyroid agents, such as propylthiouracil (PTU) or methimazole (Tapazole), which block secretion of the thyroid hormone. They may be also be given as preparation for surgery. If prescribed as medical therapy, these drugs are given daily, generally over a long time. They may have toxic effects—fever, skin rash, and enlarged lymph nodes, with an increase in white blood cells. Therapeutic doses of radioactive iodine (RAI) may also be prescribed. RAI is administered as an oral solution absorbed through the gastrointestinal tract. The radioactive iodine is transported to the thyroid gland, where it destroys the gland’s ability to make T4 and T3.
Thyroidectomy, removal of the thyroid gland, is no longer the treatment of choice and is done only after antithyroid drugs and radioactive iodine have proved unsuccessful, or when the goiter is so large that it constricts structures in the neck region.
Nursing Considerations
Nursing care focuses on minimizing overactivity, improving nutritional status, maintaining a normal body temperature, and improving self-esteem. Assist in providing a calm environment and minimizing the client’s expenditure of energy by helping with activities and encouraging alternating periods of rest and activity. Provide increased calories and nutritional support to help improve the client’s nutritional status. Diet therapy usually consists of increased caloric and protein needs, vitamins (especially B complex and D), minerals (especially calcium), and fluids. If exophthalmos is present, the client can use eye protection, such as patches, drops, or artificial tears. If body temperature is elevated, give acetaminophen (Tylenol) as ordered and use cooling blankets to reduce body temperature. Because the client is experiencing changes in appearance, appetite, and weight along with overactivity, convey understanding, concern, and willingness to help.
Hypothyroidism
Hypothyroidism occurs when a deficiency of T4 slows down metabolic processes. It may be due to removal of the thyroid gland or to a decrease in its activity. It is more likely to affect women than men. The congenital form of this deficiency causes a condition called congenital hypothyroidism. Advanced hypothyroidism in the adult is called myxedema.
Signs and Symptoms
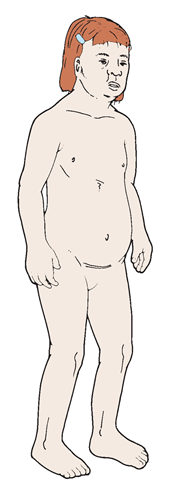
Untreated congenital hypothyroidism results in arrested physical and mental development and dystrophy of bones and soft tissues (Fig. 79-2). The person is dwarfed and has a large head, short arms and legs, puffy eyes, and a protruding tongue. The person also has dry skin and movements that are uncoordinated; sterility occurs in almost all cases. Intellectual impairment ranges from moderate to severe.If discovered early, this condition can often be successfully treated with administration of T4 replacement, which must continue for life.
In adults, myxedema is evidenced by a slowing of physical and mental activity, accompanied by forgetfulness and chronic headache. The client’s expression becomes masklike. The skin is dry; the voice is hoarse and low; hair is coarse and tends to fall out; and the client gains weight. The client may become chronically constipated and anemic, and heart rate may be affected. The RAIU uptake rate will almost always be normal; menorrhagia (excessive menstrual flow) may occur.
Treatment
Oral thyroid extract, such as thyroglobulin (Armour Thyroid), may be ordered. More commonly, synthetic thyroid hormones such as levothyroxine sodium (Levothroid) or liothyronine sodium (Cytomel) are given to supply the hormone deficiency. The results are dramatic. The client becomes more alert and the appearance becomes normal. Replacement therapy must be done gradually because a rapid change can be dangerous; for example, the heart rate may increase too rapidly and show signs of strain from increased activity.
FIGURE 79-2 · A client with congenital hypothyroidism.
Nursing Considerations
Nursing care focuses on the client’s improvements in activity tolerance and independence, resuming normal bowel function, improving mental activity, and adhering to the medical regimen. Anyone with a thyroid deficiency is susceptible to respiratory depression from sedatives or hypnotics. Some people must take thyroid replacement preparations all their lives, but with regulated treatment, they remain well and healthy. Follow-up visits with healthcare providers for periodic examinations are essential.
Nursing Alert Do not give sedatives, narcotics, and hypnotic drugs to the person with hypothyroidism or give them in very small doses. Rationale: The client’s respiratory and heart rates are already slow; additional depressants could cause respiratory or cardiac arrest.
Be alert for signs of myocardial infarction (MI). Rationale: Mi could result from the long period of slowed circulation to heart muscle.
Immediately report any complaints of anginal pain, which can occur when thyroid hormone therapy begins. Teach the client signs and symptoms of angina. Rationale: This pain can be the first sign of an Mi. A clot may block a portion of the coronary circulation.
Long-term untreated hypothyroidism can result in myxedema coma, a medical emergency necessitating immediate but careful administration of thyroid hormone. Treatment of any depressed respiratory function that occurs and close monitoring of cardiac function are essential.
Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is hypothyroidism believed to be autoimmune in origin. It is of the type of autoimmune disorders known as organ specific because the body builds up antibodies against thyroid tissue only.
Simple Goiter
Sometimes the thyroid gland, even though enlarged, does not cause toxic symptoms, in which case it is called a colloid goiter or a simple goiter. The thyroid gland enlarges and the distended spaces are filled with colloid, a gelatinous material. No symptoms of T4 deficiency are noted. (If symptoms of too much T4 occur [hyperthyroidism], the goiter is referred to as a toxic goiter.)
Simple goiter affects women more commonly than men and may appear during pregnancy, adolescence, or infection. Except for its appearance, a simple goiter usually has no harmful effects on health, unless it becomes so large that it interferes with swallowing or breathing.
Usually, a dietary deficiency of iodine causes simple goiter. The thyroid gland must have iodine to produce thyroid hormones. If a sufficient iodine supply is unavailable, the gland enlarges. Sea (salt) water, some soils, and inland drinking water contain iodine. Noncoastal areas—such as mountainous areas, the Pacific Northwest, and the Great Lakes region—are deficient in iodine.
Treatment
Goiter is treated by giving iodine to the client for a period of 2 to 3 weeks and repeating the treatment three or four times during the year, if dietary iodine intake is deficient. Administration of iodine does not cure simple goiter; it prevents it or stops its progression.
The most economical, suitable, and reliable goiter prevention program is the use of iodized table salt. Reinforcing the body’s supply of iodine is simple because the thyroid needs a very small amount. Surgery may be necessary if a goiter causes excessive pressure.
Thyroid Neoplasms
A liquid or semisolid cyst sometimes forms in the thyroid. It can be located by ultrasound. A simple cyst can be aspirated. A semisolid cyst is most often malignant and must be surgically removed. A malignant tumor can occur any time from childhood to late adulthood. If a thyroid tumor is cancerous, it must be removed surgically or treated by irradiation with radioactive isotopes. A biopsy study will tell whether such a growth is malignant. Most common thyroid cancers are slow growing, although a fast-growing adenocarcinoma may metastasize and not respond to radiation therapy.
Thyroidectomy
Thyroidectomy is surgical removal of the thyroid gland. Surgery to remove tissue from the thyroid was once the primary method of treating hyperthyroidism. Today, however, surgery is reserved for special circumstances, such as for pregnant women, those who are allergic to antithyroid medications, and clients with large goiters. Generally, only part of the gland is removed (subtotal thyroidectomy) so that some thyroid hormone production continues postoperatively. Before surgery, antithyroid agents may be administered until signs of hyperthyroidism are minimized. In addition, ß-adrenergic blocking agents (usually propranolol [Inderal]) may be used to reduce the heart rate. However, if these measures fail to achieve a normal thyroid state, iodine (Lugol’s solution or potassium iodide) may be given. Thyroid hormone levels and metabolic rate must be normalized before surgery to reduce the risk of thyroid storm (see discussion below).
A subtotal thyroidectomy usually prevents the recurrence of hyperthyroidism because only enough of the gland is left to maintain normal function. If a total thyroidectomy is done (because of injury or malignancy), the client requires thyroid hormone (thyroxine; T4) for life.
Postoperative Complications
Postoperatively, the client is at risk for complications, including hemorrhage, hematoma formation, edema of the glottis, and injury to the recurrent laryngeal nerve. Keep airway equipment near the client’s bedside postoperatively in case edema of the laryngeal area causes respiratory distress.
Nursing Alert Internal hemorrhage and edema following thyroidectomy are postoperative threats. Inspect dressings for excessive bleeding. Check for edema in the neck or bleeding at the back of the neck. Keep an endotracheal tube available in the client’s room, both preoperatively and postoperatively because swelling may obstruct the airway causing respiratory distress. In this event, an endotracheal tube is inserted, and the client is taken to the Operating Room for a tracheostomy
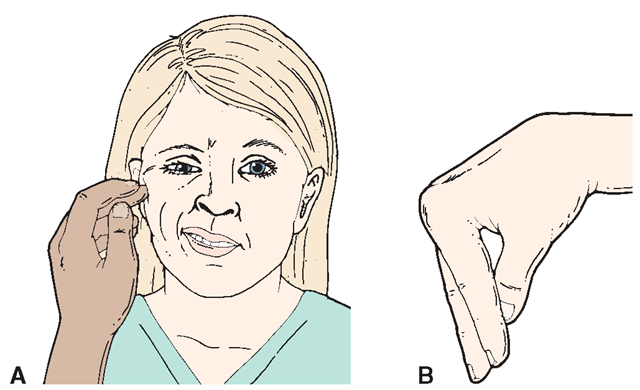
Another potential and dangerous complication is tetany, a generalized continuous muscle spasm of the entire body. It is most often caused by accidental removal of the parathyroid glands during thyroidectomy. Chvostek’s sign (abnormal spasm of the facial muscles in response to light taps on the facial nerve) and Trousseau’s sign (an abnormal carpopedal spasm induced by inflating a sphygmomanometer cuff on the upper arm to a pressure exceeding systolic blood pressure for 3 minutes) may be positive (Fig. 79-3). (Trousseau’s sign also may be seen in clients with hypocalcemia and hypomagnesemia.) Serum calcium levels also may be low. This condition may be fatal, resulting in seizures and cardiac arrhythmias. Emergency treatment of tetany is the IV administration of calcium gluconate, which must be kept available postoperatively. PTH may be administered, along with calcium gluconate, to treat the condition. If the parathyroid glands have been totally removed, administration of PTH must continue for life.
Thyroid crisis (thyrotoxicosis or thyroid storm) is another possible complication that can occur in the hospital or possibly after discharge. It is a dangerous condition caused by a sudden increase in T4. Before and after surgery, be alert for symptoms such as tachycardia, anxiety, and an abrupt increase in vital signs. This extreme form of thyrotoxicosis can cause heart failure. Treatment focuses on maintaining oxygen and glucose levels in the body cells, while reducing fever. Sedatives, tranquilizers, and cardiotonics may be prescribed. Thyroid storm is less prevalent postoperatively with the use of antithyroid drugs and iodine preparations. In some cases, corticosteroids are given.
FIGURE 79-3 · (A) Chvostek’s sign. (B) Trousseau’s sign.
Nursing Considerations
Nursing considerations include encouraging the client to rest and avoid excessive physical activity and to increase nutritional intake to ensure adequate calories, vitamin D, and calcium. Teach the client the importance of continued medication therapy and the signs and symptoms of hypofunction and hyperfunction. Reinforce the need for close follow-up after surgery. Periodically, the client will need to have thyroid function tests done as part of the follow-up.