Binding Mechanism
Information about the form, depth, motion, and color of objects in a visual field is conveyed by separate neuronal pathways to the brain. This information is processed by different cell groups in the cortex. A mechanism, which has not yet been delineated, is believed to integrate the information processed by different cortical cell groups in order to build an image of an object that combines specific information regarding its form, depth, color, and motion. This mechanism is called the binding mechanism.
Visual Reflexes
Pupillary Light Reflex
Briefly, the axons of preganglionic sympathetic neurons, which are located in the intermediolateral cell column at thoracic level 1, synapse on neurons in the superior cervical ganglia. The postganglionic sympathetic fibers arising from the superior cervical ganglia innervate the radial (dilator) smooth muscle fibers of the iris. Activation of the sympathetic nervous system results in contraction of the radial muscles of the iris, which brings about mydriasis (pupillary dilatation). Interruption of sympathetic innervation to the eye results in Horner’s syndrome.
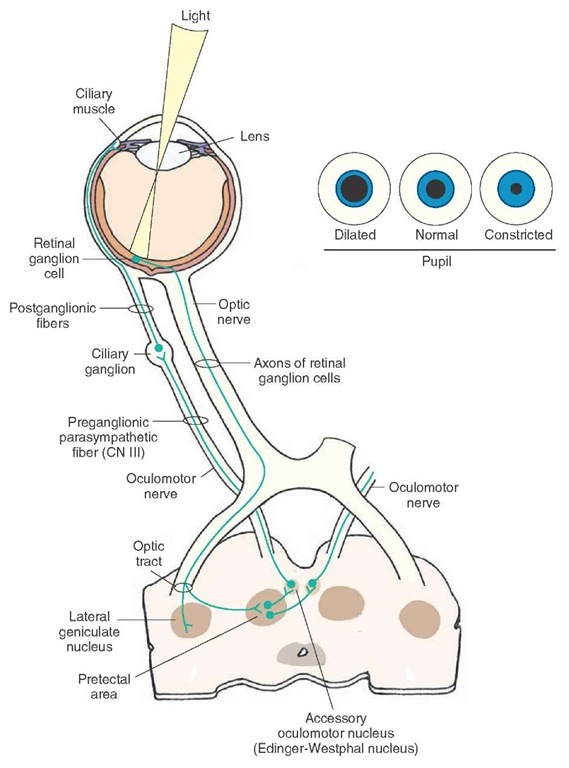
The pathways involved in the parasympathetic component of the pupillary light reflex are shown in Figure 16-11. The axons of the retinal ganglion cells project to the pretectal area via the optic tract. The pretectal area of the midbrain is located just rostral to the superior colliculus. The cells in the pretectal area send bilateral projections to preganglionic parasympathetic neurons located in the Edinger-Westphal nucleus, a component of the oculomotor nucleus.
FIGURE 16-11 Pathways mediating the pupillary light reflex. The axons of the retinal ganglion cells project to the pretectal area. The neurons in the pretectal area send projections to the preganglionic parasympathetic neurons of the ipsilateral and contralateral Edinger-Westphal nuclei. The axons of the neurons in each Edinger-Westphal nucleus exit through the ipsilateral oculomotor nerve and project to the corresponding ciliary ganglion. The postganglionic fibers of the ciliary ganglion innervate the ciliary muscle.
The axons of the preganglionic parasympathetic neurons located in the Edinger-Westphal nucleus leave the brainstem through the oculomotor nerve (cranial nerve [CN] III) and synapse on the postganglionic parasympathetic neurons in the ciliary ganglion, which is located in the orbit. The postganglionic fibers from the ciliary ganglion enter the eyeball and innervate the circular smooth muscle (sphincter muscle) of the iris and the circumferential muscles of the ciliary body. When the retinal ganglion cells are activated by bright light, the neurons in the pretectal area discharge, which, in turn, excite parasympathetic pregan-glionic cells in the Edinger-Westphal nucleus. These events finally result in an increase in the activity of para-sympathetic innervation to the smooth muscle of the pupillary sphincter, which contracts to produce miosis (constriction of the pupil) and reduce the light entering the eye. Light shone on the retina of one eye causes constriction of pupils in both eyes. The response in the eye on which the light was directed is called the direct pupillary light reflex, while the response in the contralat-eral eye is called the consensual pupillary light reflex. The consensual response occurs because the pretectal area projects bilaterally to the Edinger-Westphal nuclei. Contraction of circumferential muscles of the ciliary body results in the relaxation of the suspensory ligaments of the lens, causing it to become more convex and, thus, allowing for greater refraction of the light rays, which is more suitable for near vision. These two responses (i.e., constriction of the pupil and increasing the convexity of the lens) are included in the accommodation reflex (described in the next section).
Accommodation Reflex
The accommodation reflex comes into play when the eye has to focus from a distant object to a near one. The reflex involves the following three events: (1) convergence of the eyes, (2) constriction of the pupil, and (3) fixation of the lens for near vision (i.e., by making it more convex). Convergence of the eyes takes place as a result of direct or indirect cortical projections to somatic components of the Edinger-Westphal nucleus, which activate the medial rectus muscles bilaterally. As mentioned earlier, pupillary constriction, which is necessary for the near object to be in focus, results from activation of a parasympathetic pathway from the Edinger-Westphal nucleus to the ciliary ganglion and postganglionic fibers to pupillary constrictor muscles. Fixation of the lens for near vision is brought about by activation of the parasympathetic component of the third nerve. Preganglionic fibers project to the ciliary ganglion, which, in turn, send postganglionic fibers to the circumferential muscle fibers of the ciliary body. Contraction of these muscles reduces tension on the suspensory ligament, allowing the lens to become more convex.
Prominent Defects in Vision
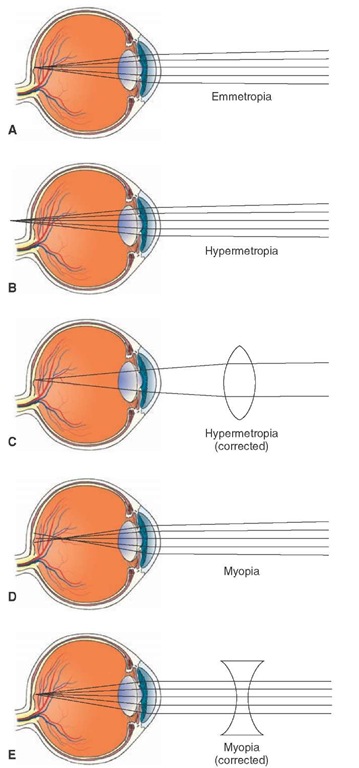
In a normal eye (emmetropic eye), parallel rays of light from a distant object are focused sharply on the retina when the ciliary muscle is completely relaxed. To be able to focus a near object on the retina in an emmetropic eye, the ciliary muscle must contract and accommodate for near vision (Fig. 16-12A).
Hypermetropia
In hypermetropia (hyperopia; far-sightedness), either the eyeball is too small or the lens system is too weak so that parallel light rays from an object are not bent sufficiently and are focused behind the retina when the ciliary muscle is completely relaxed (Fig. 16-12B). This condition can be corrected by placing a convex lens of appropriate strength in front of the eye; after this correction, the parallel light rays coming from a distant object are converged and focused on the retina (Fig. 16-12C).
Myopia
Myopia (near-sightedness) is usually caused by the increased length of the eyeball or, occasionally, by increased power of the lens system. When the ciliary muscle is completely relaxed, the light rays coming from a distant object are focused in front of the retina (Fig. 16-12D). This condition can be corrected by placing a concave lens of an appropriate strength in front of the eye; in this manner, parallel light rays coming from a distant object are diverged by the concave lens and, thus, focused on the retina (Fig. 16-12E).
Astigmatism
Astigmatism usually occurs when the shape of the cornea is oblong. Because of this shape, the curvature of the cornea in one plane is less than the curvature in the other plane. Accordingly, the light rays coming from an object are bent to a different extent in these two different planes, preventing the light rays from coming to a single focal point. This condition is corrected by placing a cylindrical lens in front of the eye.
FIGURE 16-12 Errors in refraction. (A) Normal (emmetropic) eye. (B) In hypermetropia (hyperopia, far-sightedness), light rays are focused behind the retina when the ciliary muscle is completely relaxed. (C) Hypermetropia can be corrected by placing a convex lens of appropriate strength in front of the eye. (D) In myopia (near-sightedness), the light rays coming from a distant object are focused in front of the retina when the ciliary muscle is completely relaxed. (E) Myopia can be corrected by placing a concave lens of an appropriate strength in front of the eye.
Strabismic Amblyopia
Stereoscopic vision develops as early as 3 months after birth. In some infants, the visual axes of the two eyes are not parallel; this is called strabismus (squint). To avoid diplopia (double vision), the infant suppresses foveal vision in the nondominant eye that is, perhaps, mediated from the cerebral cortex. If the axes of the eyes are corrected during the first 6 months of the development, stra-bismic amblyopia is reversed. Strabismus is usually treated successfully by eye muscle training exercises and by the use of glasses with prisms that bend light rays so as to compensate for the abnormal position of the eyeball. In some cases, strabismus is corrected by the shortening of some of the eye muscles using careful surgical procedures.
Night Blindness
As noted already, the photosensitive pigments are composed of a protein (opsin) and vitamin A aldehyde (retinal). Vitamin A deficiency is, therefore, likely to reduce the amount of this photosensitive pigment in rods and cones. Even though the photosensitive pigment is depleted, daylight is able to activate the remaining pigment. Therefore, daylight vision is not significantly affected. However, light level at night is insufficient to activate the depleted pigment; therefore, the person cannot see in the dark. Oral supplements of vitamin A are helpful in night blindness (nyctalopia).
Color Blindness
Mutations in one or more cone-opsin genes encoding for red and green pigments usually results in color blindness (inability to detect a particular color). Most individuals with color blindness are red-green blind, and the majority of these are blind to green color. A minority of individuals are blue color-blind. Because red-green color blindness is inherited by an X-linked recessive gene, more males than females are affected.
Argyll Robertson Pupil
In syphilitic patients with CNS complications (tabes dor-salis or neurosyphilis), the pupils do not contract in response to light, but they do exhibit constriction as a component of the accommodation reflex. This indicates that the retina is still sensitive to light and that the pre-ganglionic and postganglionic autonomic fibers innervating the eye are intact. In these patients, the pupillary light reflex is absent because the pretectal area, which receives inputs from optic fibers that are essential for eliciting this reflex, is damaged. However, the pretectal area is not essential for eliciting pupillary constriction during the time when the accommodation reflex occurs. The precise location of the lesion is not known in Argyll Robertson pupil. However, it is hypothesized that the descending pathways from the visual cortex, which mediate pupillary constriction in the accommodation reflex, bypass the pre-tectal area and project to the Edinger-Westphal nucleus of the third nerve. These pathways are not affected in patients with neurosyphilis. Therefore, the mechanism of pupillary constriction during the accommodation reflex remains largely intact in these patients, whereas the pupillary light reflex is absent due to damage to the pretectal area.
Adie’s Pupil
In Adie’s pupil, there is a prolonged and sluggish constriction of the pupil to light. Following the pupillary constriction, the dilation of the pupil is delayed. Patients with this disorder have pathological changes in the ciliary ganglion.
Marcus-Gunn Pupil
In Marcus-Gunn pupil, one of the eyes has an optic nerve lesion. A swinging flashlight test is conducted to test the pupillary light reflex in such patients as follows. During this test, the patient sits in a dimly lit room, then the light source is moved quickly back and forth from one eye to another, and pupillary constrictions are noted. When light is shone on the normal eye, both pupils constrict (direct and consensual light reflexes). When the light is shone on the eye with the optic nerve lesion, lesser signals reach the Edinger-Westphal nucleus. This nucleus senses the lesser intensity of light and shuts off the parasympathetic response to the light stimulus, causing paradoxical dilation of both pupils.
Weber Syndrome
Weber syndrome is usually caused by an infarct that affects the rootlets of the oculomotor nerve. The symptoms include deviation of the eye downward and outward, drooping of the eyelid, and a dilated and nonresponsive pupil on the ipsilateral side, accompanied by contralateral upper motor neuron paralysis.
Parinaud Syndrome
Parinaud syndrome is caused by lesions in the pretectal area. The patient suffers from paralysis of upward gaze, a large pupil, and retraction of eyelids.
Retinitis Pigmentosa
This visual disorder encompasses a diverse group of hereditary visual defects characterized by a gradual loss of vision caused by degeneration of photoreceptors. So far mutations of about 30 genes have been linked to retinitis pigmentosa. The photoreceptors degenerate due to apop-tosis. Inflammation of the retina (as the name would seem to suggest) is not the main symptom of this disease. Common symptoms are narrowing of retinal vessels and formation of dark clumps of pigment released from the damaged retinal pigment epithelium. Usually the clumps are formed near the retinal blood vessels. Initially loss of rod photoreceptors results in night blindness. Subsequently, cones also degenerate and there is a progressive loss of vision.
Macular Degeneration
Macular degeneration is most common in those older than age 55 years. The disorder is characterized by a progressive loss of vision. Initially there is a blurring of vision and images appear distorted. Patients with this visual defect may see blurred vertical and parallel lines on Amsler grid (a chart like a graph paper that is used to test vision in these patients). The cause of the disease is not known. Multiple factors (e.g., smoking, exposure to light, cardiovascular disease, heredity) have been implicated. In some patients, abnormal blood vessels are present under the macula. Blood leaking from these vessels reaches the retina causing damage to the photoreceptors. The loss of vision in this situation is rapid. Treatment of this condition (the wet form of macular degeneration) involves administration of a light-activated drug (e.g., Visudyne) into the arm. As the drug passes through the abnormal retinal blood vessels, a low energy, non-thermal laser pulse of a particular wavelength is applied, causing a chemical reaction that destroys the abnormal blood vessels. Thus, leakage of blood into the retina is reduced or eliminated. The procedure is painless and causes little or no damage to the surrounding tissue.
In a majority of patients with macular degeneration, retinal pigment epithelium is damaged at restricted regions, causing loss of photoreceptors and loss of visual function in these areas. There is some intact visual function in these patients. At present there is no treatment for this condition (the dry form of macular degeneration). Sometimes macular degneration occurs in young individuals (less than 20 years of age). This condition is caused by genetic mutations. Most of the patients with this condition are legally blind before they are 50 years old.