Adrenergic Receptors
Adrenergic receptors are divided into two major classes: alpha-adrenergic receptors and beta-adrenergic receptors. These classes have been further subdivided into alpha1- and alpha2-adrenergic receptors and beta1- and beta2-adrenergic receptors. Alpha1-adrenergic receptors are located on the membranes of postsynaptic cells. These receptors may be linked through a G protein. G proteins bind guanosine diphosphate (GDP) and guanosine triphosphate (GTP). When norepinephrine binds to an alpha1-adrenergic receptor, the receptor is activated, and second messengers inositol 1,4,5-triphosphate (IP3) and diacylglycerol (DAG) are liberated. IP3 releases Ca2+ (calcium) from its stores in the endoplasmic reticulum and is also phosphorylated to form inositol 1,3,4,5-tetraphos-phate, which opens calcium channels located in the cell membrane. Ca2+ then binds with calmodulin, and phos-phorylation of a protein occurs to elicit a cellular response. DAG activates protein kinase C, which, in turn, promotes protein phosphorylation and subsequent cellular response.
TABLE 22-2 Stimulation of Autonomic Nerves and the Responses of Different Organs
|
Organ |
Sympathetic Response |
Predominant Receptor |
Parasympathetic Response |
Predominant Teceptor |
|
Eye |
||||
|
Iris: radial muscle |
Contraction (mydriasis) |
Alpha-1 |
- |
- |
|
Iris: sphincter |
- |
- |
Contraction (miosis) |
Muscarinic |
|
Ciliary muscle |
Relaxation (far vision) |
Beta-2 |
Contraction (near vision) |
Muscarinic |
|
Lacrimal glands |
Secretion |
Alpha |
Secretion |
Muscarinic |
|
Heart |
||||
|
Sinoatrial node |
Tachycardia |
Beta-1 |
Bradycardia |
Muscarinic |
|
Atria |
Increased contractility |
Beta-1 |
Decreased contractility |
Muscarinic |
|
Atrioventricular node |
Increased conduction |
Beta-1 |
Decreased conduction |
Muscarinic |
|
Ventricle |
Increased contractility |
Beta-1 |
- |
- |
|
Arteries and Arterioles |
||||
|
Most organs |
Constriction |
Alpha-1 |
No innervation |
- |
|
Coronary artery |
Constriction |
Alpha-1 |
No innervation |
- |
|
Pulmonary artery |
Constriction |
Alpha-1 |
No innervation |
- |
|
Dilation |
Beta-2 |
|||
|
Renal artery |
Constriction |
Alpha-1 |
No innervation |
- |
|
Dilation |
Beta-2 |
|||
|
Abdominal organs |
Constriction |
Alpha-1 |
No innervation |
- |
|
Dilation |
Beta-2 |
|||
|
Most veins |
Constriction |
Alpha-1 |
No innervation |
- |
|
Dilation |
Beta-2 |
|||
|
Skeletal muscle |
Constriction |
Alpha-1 |
No innervation |
- |
|
Lungs |
Dilation |
Beta-2 |
||
|
Bronchial and tracheal smooth muscle |
Relaxation |
Beta-2 |
Contraction |
Muscarinic |
|
Stomach and Intestine |
||||
|
Motility |
Decreased |
Alpha-1 |
Increased |
Muscarinic |
|
Secretion |
Decreased |
Alpha-2 |
Increased |
Muscarinic |
|
Kidney |
||||
|
Renin secretion |
Decreased |
Alpha-1 |
No innervation |
- |
|
Increased |
Beta-1 |
|||
|
Urinary bladder |
||||
|
Detrusor trigone and sphincter |
Relaxation |
Beta-2 |
Contraction |
Muscarinic |
|
Contraction |
Alpha-1 |
Relaxation |
Muscarinic |
|
|
Ureter |
||||
|
Motility |
Increased |
Alpha-1 |
? |
- |
|
Uterus |
||||
|
Smooth muscle |
Contraction |
Alpha-1 |
Depends on circulating |
Muscarinic |
|
Relaxation |
Beta-2 |
estrogen and progesterone |
||
|
Male sex organ |
Ejaculation |
Alpha-1 |
Erection |
Muscarinic |
|
Skin |
||||
|
Pilomotor muscle |
Contraction |
Alpha-1 |
- |
- |
|
Spleen-capsule |
Contraction |
Alpha-1 |
- |
- |
|
Relaxation |
Beta-2 |
- |
- |
TABLE 22-2 Stimulation of Autonomic Nerves and the Responses of Different Organs
|
Organ |
Sympathetic Response |
Predominant Receptor |
Parasympathetic Response |
Predominant Teceptor |
|
Liver |
Glycogenosis |
Alpha-1 |
- |
- |
|
Gluconeogenesis |
Beta-2 |
- |
- |
|
|
Pancreas |
||||
|
Acini |
Decreased secretion |
Alpha |
Increased secretion |
Muscarinic |
|
Beta cells |
Decreased secretion |
Alpha-2 |
- |
- |
|
Increased secretion |
Beta-2 |
- |
- |
|
|
Fat cells |
Lipolysis |
Alpha & Beta |
- |
- |
|
(thermogenesis) Inhibition of lipolysis |
Alpha-2 |
- |
- |
Alpha2-adrenergic receptors are present on the presyn-aptic membranes of adrenergic nerve terminals. Activation of alpha2-adrenergic receptors at these endings by the released transmitter (norepinephrine) inhibits further release of the transmitter. This phenomenon is called autoinhibition.Stimulation of alpha2-adrenergic receptors has been reported to inhibit ade-nylate cyclase and lower cyclic adenosine monophosphate (cAMP) levels in some effector cells. As mentioned previously,cAMP stimulates enzymes (e.g., protein kinase A), which then phosphorylate appropriate ion channels. Phosphorylation of ion channels by protein kinases results in the opening of these channels, ions flow across the cell membrane, and the cells are depolarized and rendered more excitable. Decrease in cAMP levels, therefore, elicits opposite responses.
Beta-adrenergic receptors are located in the heart; stimulation of these receptors results in an increase in heart rate and contractility.Beta2-adrenergic receptors are located in smooth muscles (e.g., bronchial smooth muscle); their activation results in the relaxation of these muscles.
The responses of some effector organs to autonomic nerve stimulation and the receptors mediating these responses are summarized in Table 22-2.
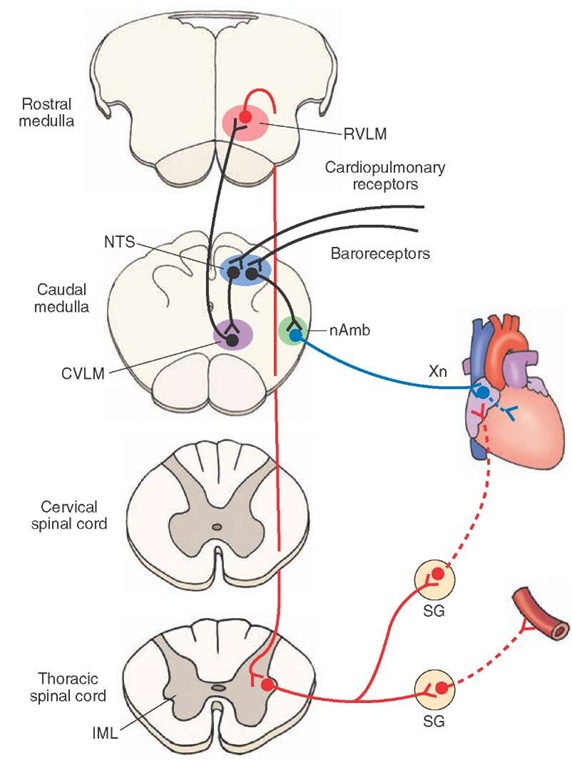
Brainstem Areas Regulating Cardiovascular Function
Regulation of the cardiovascular system is an autonomic function. Animal experiments have implicated several neuronal pools in this function. It is believed that the organization of these areas in humans is similar to that described for several animal species. The mechanisms that maintain cardiovascular function at an optimum level in healthy individuals are located in the brainstem (Fig. 22-11). However, higher integrative areas (e.g., hypothalamus and cortex) also have a profound influence on cardiovascular function. For example, specific stimulation of neurons located in different areas of the hypothalamus results in specific changes (either a decrease or increase) in blood pressure and heart rate.
The Solitary Nucleus
This nucleus consists of a column of cells on each side of the fourth ventricle. At the rostral edge of the area pos-trema, the columns of the nucleus of the solitary tract (NTS) on the two sides merge in the midline to form the commissural subnucleus of the NTS.Recall that the area postrema is a circumventricular organ (i.e., it lacks a blood-brain barrier) that is located in the caudal region of the floor of the fourth ventricle.Medial and commissural subnuclei in the caudal regions of the NTS are the sites where the central terminals of baroreceptor, chemoreceptor, and cardiopul-monary sensory neurons make their first synapse. Barore-ceptor neurons sense changes in blood pressure, chemoreceptor neurons sense changes in blood gases and pH, and cardiopulmonary receptor neurons are activated by noxious chemicals in the cardiopulmonary circulation. The role of the NTS in mediating the reflex cardiovascular responses to baroreceptor, chemoreceptor, and cardiopul-monary receptor activation is discussed in the following sections.
Caudal Ventrolateral Medullary Depressor Area
This region is located in the ventrolateral medulla, ventral to the NTS (Fig. 22-11). The caudal ventrolateral medullary depressor area (CVLM) is an important relay nucleus for mediating baroreflex and cardiopulmonary reflex, but not chemoreflex, responses. It contains a population of gamma-aminobutyric (GABA)-ergic neurons that projects to the rostral ventrolateral medullary pressor area (see next section). Activation of baroreceptors and cardiopulmo-nary receptors results in an activation of these GABAergic neurons. Release of GABA at their terminals causes an inhibition of rostral ventrolateral medullary neurons, which results in a decrease in blood pressure and heart rate (see the following sections, "Baroreceptor Reflex" and "Cardiopulmonary Reflex").
FIGURE 22-11 Cardiovascular neuronal pools involved in baroreflex (see text for details). nAmb = nucleus ambiguus; Xn = vagus nerve; SG = sympathetic ganglion; IML = intermedi-olateral cell column of the spinal cord; CVLM = caudal ventrolateral medullary depressor area; NTS = solitary nucleus (also known as nucleus tractus solitarius); RVLM = rostral ventrola-teral medullary pressor area.
Rostral Ventrolateral Medullary Pressor Area
This area is located in the ventrolateral medulla rostral to the CVLM and caudal to the facial nucleus (Fig. 22-11). The rostral ventrolateral medullary pressor area (RVLM) is believed to be one of the most important regions involved in the maintenance of sympathetic tone. The tonically active, barosensitive, sympathoexcitatory RVLM neurons send direct monosynaptic projections to the IML, where the sympathetic preganglionic neurons are located.
Nucleus Ambiguus
The role of the nucleus ambiguus in regulating cardiac function has been discussed earlier in this topic.This nucleus receives direct or indirect excitatory projections from the NTS.
Intermediolateral Cell Column
The location and function of the IML has been discussed earlier in this topic.As mentioned earlier, sympathetic preganglionic neurons are located in the IML of the thoracolumbar cord, and they receive monosynaptic projections from the RVLM neurons.
Baroreceptor Reflex
The pathways and transmitters involved in the barore-ceptor reflex can be summarized as follows (Fig. 22-11). Cardiovascular responses to the stimulation of barore-ceptors are hypotension and bradycardia. Activation of baroreceptor afferents, in response to an elevation in systemic blood pressure, results in the release of an excitatory amino acid (most probably glutamate) in the dorsomedial NTS. Excitation of the second-order NTS neurons involved in the baroreflex results in the activation of an excitatory projection to the CVLM, and an excitatory amino acid is released in the CVLM. Activation of GABAergic neurons in the CVLM results in the release of GABA in the RVLM, causing inhibition of RVLM neurons. RVLM neurons normally provide a tonic excitatory input to the IML; glutamate is believed to be the transmitter released at the terminals of this projection. Therefore, inhibition of RVLM neurons results in a decrease in the excitatory input to the sympathetic pre-ganglionic neurons in the IML. When this occurs, the activity of postganglionic sympathetic innervation to the arterioles and heart is decreased. Consequently, blood pressure and heart rate are decreased. However, activation of vagal innervation plays a major role in mediating reflex bradycardia. As mentioned earlier, vagal innervation to the heart is provided predominantly by the nucleus ambiguus. The presence of an excitatory projection from the NTS to the nucleus ambiguus has been reported; this projection is activated when the activity of baroreceptors increases in response to an increase in the systemic blood pressure.
Cardiopulmonary Reflex
In experimental animals, injections of noxious chemicals (e.g., capsaicin, which is a pungent substance in hot chili peppers) via the right atrium elicit a triad of responses characterized by apnea, bradycardia, and hypotension. The receptors responding to these stimuli are located in the lungs and the heart, and the responses are mediated by vagal C-fiber afferents. The pathways involved in the cardiopulmonary reflex are identical to those described for baroreflex (Fig. 22-11). The exact physiological role of these receptors in humans has not been established. In experimental animals, injections of noxious chemicals in the right atrium are used to study the neural circuits involved in this reflex.