Male Reproductive System
Sympathetic Innervation
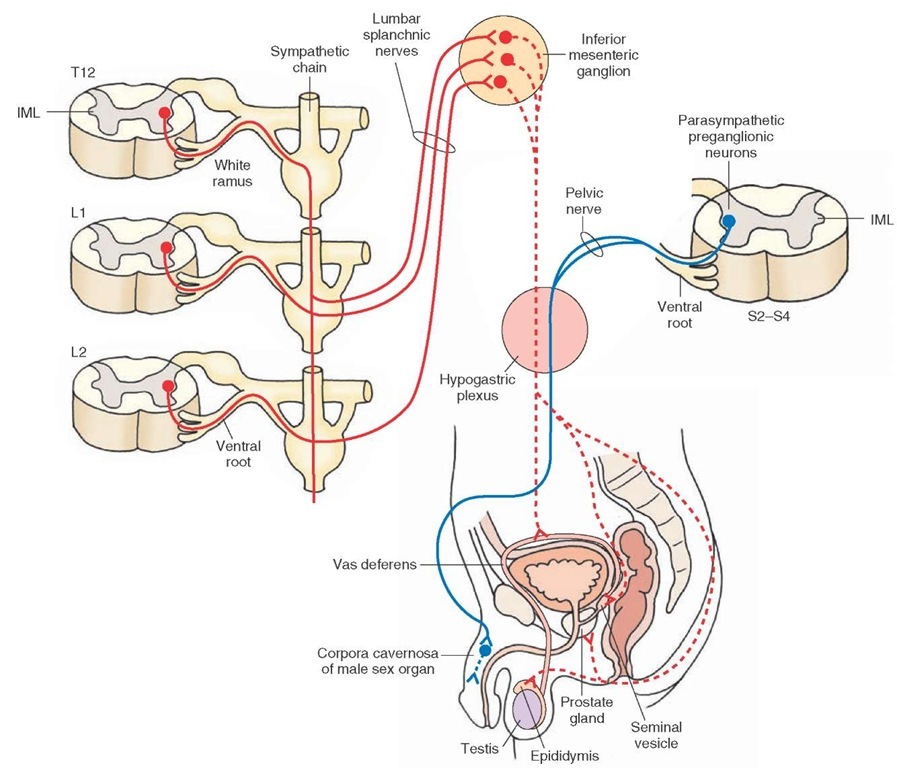
The sympathetic preganglionic neurons innervating the male reproductive system (i.e., epididymis, vas deferens, seminal vesicles, and prostate glands) are located in the IML at the T12-L2 level. Their preganglionic fibers pass through the sympathetic chain, exit in the lumbar splanchnic nerves, and synapse on the neurons in the inferior mesenteric ganglion. The axons of these postganglionic neurons reach their target tissues in the male reproductive system via the hypogastric plexuses (Fig. 22-9). Some preganglionic fibers from L1-L2 spinal segments descend in the sympathetic chain and synapse on postganglionic neurons in the hypogastric plexus. The postganglionic fibers from these neurons then innervate the male erectile tissue (penis) (Fig. 22-1). Activation of the sympathetic nervous system causes ejaculation of spermatozoa, along with secretions of the prostate and the seminal vesicles.
Parasympathetic Innervation
The parasympathetic preganglionic neurons innervating the erectile tissue (corpora cavernosa) in the male sexual organ are located in the IML of the sacral spinal cord at the S2-S4 level. The male erectile tissue is composed of many cavities. The parasympathetic preganglionic fibers exit from the ventral roots, travel in the pelvic nerves, pass through the hypogastric plexus, and are distributed to the erectile tissue (Fig. 22-9).
Male Erectile Dysfunction
Activation of the parasympathetic nervous system results in the dilation of the arteries and increased blood flow in the corpora cavernosa causing erection of the male sexual organ. In addition, nitric oxide released from nonadrener-gic and noncholinergic nerve terminals increases cyclic guanosine monophosphate (cGMP) levels in the nonvascular smooth muscle of the corpora cavernosa. Relaxation of the nonvascular smooth muscle of corpora cavernosa caused by increased levels of cGMP permits inflow of blood into the sinuses of the cavernosa. This effect contributes to the erection of the male sexual organ (penis). Disruption of any of these mechanisms causes male erectile dysfunction.
In recent years, oral administration of sildenafil (Viagra) has been used to treat male erectile dysfunction. This drug inhibits an enzyme, phosphodiesterase-5, which is responsible for the breakdown of cGMP, and increases cGMP levels in the smooth muscle cells of corpora caver-nosa. The blood flow in corpora cavernosa increases, causing it to swell up and produce an erection. The mechanism of action of vardenafil (Levitra) and tadalafil (Cialis), which have recently become available for oral treatment of male erectile dysfunction, is similar to that of sildenafil. It is important to note that currently available drugs used for the treatment of male erectile dysfunction should not be used by individuals who take nitrates and alpha-adrenergic receptor blockers for the treatment of other disorders because all of these drugs lower blood pressure and their combined use may reduce blood pressure to dangerous levels.
FIGURE 22-9 Autonomic innervation of the male reproductive system (see text for details). Red = sympathetic nervous system; Blue = parasympathetic nervous system. Solid lines = preganglionic fibers, dotted lines = postganglionic fibers. L= lumbar; S = sacral; T = thoracic spinal segment; IML = interme-diolateral cell column.
Female Reproductive System
Sympathetic Innervation
In the female reproductive system, the sympathetic pregan-glionic neurons innervating the smooth muscle of the uterine wall are located in the IML at the T12-L2 level.
Their preganglionic fibers pass through the sympathetic chain, exit in the lumbar splanchnic nerves, and synapse on postganglionic neurons in the inferior mesenteric ganglion. The postganglionic fibers from these neurons pass through the hypogastric plexus and innervate the female sexual organ (vagina) and the uterus (Fig. 22-10). Some preganglionic fibers from L1-L2 spinal segments descend in the sympathetic chain and synapse on postganglionic neurons in the hypogastric plexus. The postganglionic fibers from these neurons then innervate the female erectile tissue (clitoris [Fig. 22-1]). Activation of the sympathetic nervous system results in contraction of the uterus.
Parasympathetic Innervation
The location of the parasympathetic preganglionic neurons and the pathways they follow to innervate the uterus and female sexual organ are similar to those described for the male sexual organ (Fig. 22-10). The mechanism of vasodilation in the female erectile tissue (clitoris) is similar to that described for the male sexual organ.
FIGURE 22-10 Autonomic innervation of the female reproductive system (see text for details). Red = sympathetic nervous system; Blue = parasympathetic nervous system. Solid lines = preganglionic fibers, dotted lines = postganglionic fibers. The green lines indicate pain afferents. L= lumbar; S = sacral; T = thoracic spinal segment; IML = intermediolateral cell column.
Parasympathetic stimulation causes stimulation of the female erectile tissue and relaxation of the uterine smooth muscle. The relaxation of the uterine smooth muscle may be variable due to hormonal influences on this muscle.
The pain-sensing neurons innervating the uterus are located in the dorsal root ganglia at T12-L2 and S2-S4. Their peripheral axons pass through the hypogastric plexus and terminate in the uterus, while their central terminals synapse in the substantia gelatinosa at the T12-L2 and S2-S4 levels. The secondary pain-sensing neurons then project to the cerebral cortex via the thalamus.
Blood Vessels
Sympathetic Innervation
Sympathetic innervation to the blood vessels in most of the organs located in the head and chest cavity is provided by the postganglionic fibers emerging from the cervical ganglia (superior, middle, and inferior) and first four thoracic paravertebral ganglia. The blood vessels in most of the organs in the abdominal cavity are provided sympathetic innervation by postganglionic fibers emerging from the prevertebral ganglia (e.g., celiac, superior mesenteric, and inferior mesenteric ganglia). As mentioned previously, sympathetic preganglionic fibers that synapse on the post-ganglionic neurons located in these prevertebral ganglia pass without synapsing in the paravertebral ganglia in the sympathetic chain.
The fibers providing sympathetic innervation of the blood vessels, sweat glands, and erectile muscles of hair follicles located in the upper and lower limbs and the trunk follow a different course. For example, the sympathetic preganglionic neurons innervating the upper limb are located in the IML at T1—T8. The axons of these pregan-glionic neurons enter the sympathetic chain via white rami, ascend through the sympathetic chain, and synapse on sympathetic postganglionic neurons located in the inferior and middle cervical paravertebral ganglia. The axons of these postganglionic neurons re-enter the spinal nerves that form the brachial plexus via gray rami and are distributed to the arteries (vasoconstrictor fibers), sweat glands (sudomotor fibers), and erectile muscle of hairs (pilomotor fibers).
Sympathetic innervation to the lower limb is provided by sympathetic preganglionic neurons located in the IML at T10-L2. The axons of these neurons enter the sympathetic chain via white rami and synapse on postganglionic neurons in the lumbar and sacral ganglia. The axons of these postgan-glionic neurons join the branches of lumbar and sacral plexuses via the gray rami and innervate the blood vessels, sweat glands, and hair follicles located in the lower limb.
The postganglionic fibers that supply sympathetic inner-vation to the blood vessels, sweat glands, and hair follicles located in the trunk also re-enter the corresponding spinal nerves via the gray rami.
Parasympathetic Innervation
The parasympathetic nervous system does not innervate the arterioles in most of the organs. Some blood vessels that do receive parasympathetic innervation are located in the lacrimal and salivary glands and male erectile tissue.
Systemic Blood Pressure
An individual’s blood pressure depends on the peripheral vascular resistance, which is determined primarily by the diameter of the systemic arterioles. The tone of the vascular smooth muscle is controlled by the activity of the noradrenergic postganglionic neurons that innervate the arterioles. Increased activity of the sympathetic nervous system results in the contraction of the arteriolar smooth muscle, thus causing an increase in peripheral vascular resistance and systemic blood pressure. A decrease in the activity of the sympathetic nervous system results in a decrease in systemic blood pressure due to a decrease in the peripheral vascular resistance, caused by relaxation of the arteriolar smooth muscle.
Neurotransmitters in the Autonomic Nervous System
Preganglionic Terminals
Within the autonomic ganglia, acetylcholine (Ach) is the transmitter released at the terminals of the sympathetic and parasympathetic preganglionic fibers. The terminal branches of the preganglionic fibers contain vesicles enclosing the neurotransmitter. The terminals make synaptic contacts with the postganglionic neurons located in the ganglia.
Postganglionic Terminals
The terminals of the sympathetic and parasympathetic postganglionic neurons innervate the effector cells in the target organs. At the terminals of most sympathetic post-ganglionic neurons, norepinephrine is the transmitter, with the exception of those neurons innervating sweat glands and blood vessels of the skeletal muscles, in which Ach is the neurotransmitter. At the terminals of all the parasympathetic postganglionic neurons, Ach is the neu-rotransmitter.
To recapitulate, Ach liberated in the synaptic cleft is removed by acetylcholinesterase that hydrolyzes the transmitter. Acetylcholinesterase inhibitors are used clinically in the treatment of many diseases. For example, donepezil (Aricept) is prescribed in Alzheimer’s disease in an attempt to improve memory function.Pyridostigmine is used to improve muscle strength in myasthenia gravis.Abdominal cramps and diarrhea, due to increased levels of Ach in the GIT, are the most common side effects of acetylcholinesterase inhibitors.
Major Receptors Involved in the Autonomic Nervous System
Cholinergic Receptors
Cholinergic receptors have been divided into two main classes: cholinergic muscarinic and nicotinic receptors. These receptors located in the visceral effector organ cells (smooth and cardiac muscle and exocrine glands) are the cholinergic muscarinic receptors. Responses elicited by the stimulation of these receptors in the visceral effector organs, called muscarinic effects of acetylcholine, include decrease in heart rate, miosis, and secretions of different glands (lacrimal, salivary, and sweat glands and glands in the GIT). Cholinergic receptors located in the adrenal medulla and autonomic ganglia are the nicotinic receptors. Remember that Ach is the transmitter at the pregan-glionic terminals synapsing on epinephrine-scereting and norepinephrine-secreting cells of the adrenal medulla.