Parasympathetic Innervation
The parasympathetic preganglionic fibers arise from neurons located in the dorsal motor nucleus of the vagus, travel to the thoracic cavity in the vagus nerves, and synapse on postganglionic neurons located in the lungs (Fig. 22-5). The postganglionic fibers then innervate the smooth muscles in the bronchial tree. Stimulation of the parasympa-thetic nervous system results in bronchoconstriction and an increase in the secretion of the bronchial glands.
FIGURE 22-5 Autonomic innervation of the heart and lungs (see text for details). Red = sympathetic nervous system; Blue = parasympathetic nervous system. Solid lines = preganglionic fibers, dotted lines = postganglionic fibers. T = thoracic spinal segment; IML = intermediolateral cell column.
Gastrointestinal Tract
Sympathetic Innervation
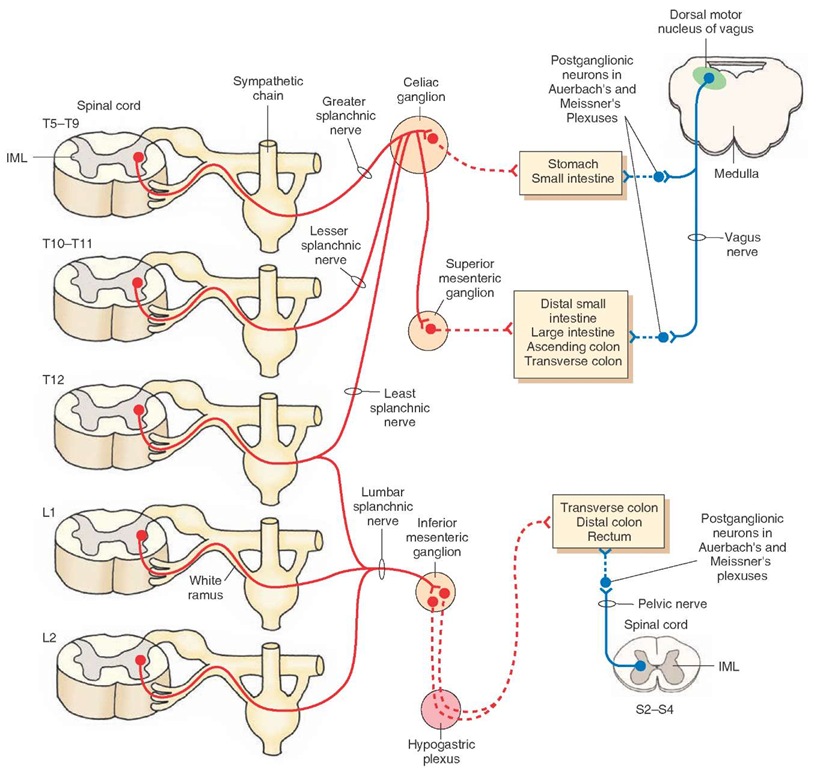
The axons from the sympathetic preganglionic neurons located in the IML at the T5-T9 level pass through the sympathetic chain without synapsing, travel through the greater splanchnic nerve, and synapse on neurons in the celiac ganglion. The preganglionic fibers arising from the IML at T10-T12 also pass through the sympathetic chain without synapsing and emerge as lesser and least splanchnic nerves. These fibers also synapse on post-ganglionic neurons in the celiac ganglion. The postgangli-onic fibers emerging from the celiac ganglion innervate the smooth muscle and glands of the stomach and small intestine. Some preganglionic fibers in the greater, lesser, and least splanchnic nerves pass through the celiac ganglion and synapse on postganglionic neurons located in the superior mesenteric ganglion. These postganglionic neurons then innervate the distal portions of the small intestine, large intestine, and ascending and transverse colon. The axons emerging from the sympathetic pregan-glionic neurons located in the IML at the T12-L2 pass through the sympathetic chain without synapsing and emerge as lumbar splanchnic nerves. These fibers then synapse on postganglionic neurons located in the inferior mesenteric ganglion. The postganglionic fibers emerging from the inferior mesenteric ganglion pass through the hypogastric plexus and innervate the transverse and distal colon and rectum (Fig. 22-6). Activation of the sympathetic nervous system, in different regions of the GIT, inhibits peristalsis and secretions of glands and contracts the sphincters.
FIGURE 22-6 Autonomic innervation of the gastrointestinal tract (see text for details). Red = sympathetic nervous system; Blue = parasympathetic nervous system. Solid lines = preganglionic fibers, dotted lines = postganglionic fibers. S = sacral; L = lumbar; T = thoracic spinal segment; IML = intermediolateral cell column.
Parasympathetic Innervation
The preganglionic neurons providing parasympathetic innervation to the stomach, small and large intestine, and colon are located in the dorsal motor nucleus of the vagus. These preganglionic fibers descend in the vagus nerves and synapse on postganglionic neurons located in the myenteric (Auerbach’s) and submucosal (Meiss-ner’s) plexuses in these regions of the GIT. The post-ganglionic fibers from these plexuses then innervate the smooth muscle and glands of the stomach, small and large intestine, and ascending and transverse colon (Fig. 22-6). The parasympathetic preganglionic neurons innervating the transverse and distal colon and rectum are located in the IML of the sacral spinal cord at the S2-S4 level (Fig. 22-6). Their preganglionic fibers exit through the ventral roots, enter the pelvic nerves, and reach the myenteric (Auerbach’s) and submucosal (Meissner’s) plexuses. The postganglionic fibers arising from these plexuses innervate the smooth muscle and glands in these regions of the GIT. Stimulation of the parasympathetic nervous system, in this and other regions of the GIT, elicits peristalsis and secretion of glands and relaxes the sphincters.
As stated earlier, the enteric division of the autonomic nervous system, consisting of the myenteric (Auerbach’s) and submucosal (Meissner’s) plexuses, regulates gastrointestinal motility and secretion. This intrinsic system can be modulated by the extrinsic control of the GIT via sympathetic and parasympathetic innervation.
Adrenal Medulla (Suprarenal Gland)
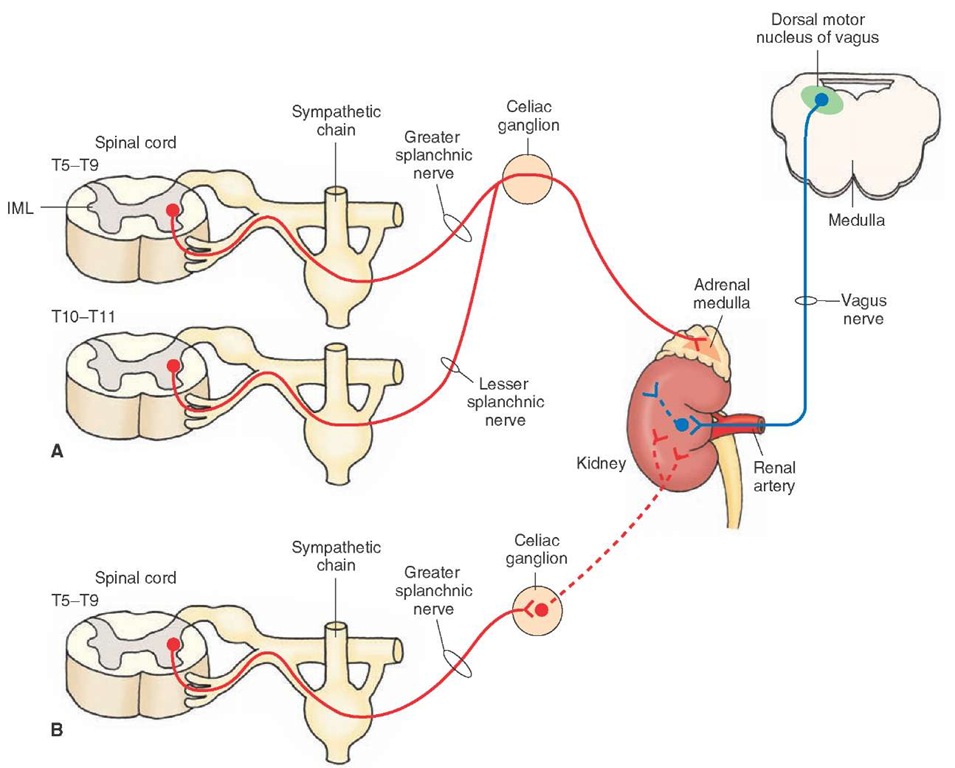
The adrenal medulla is functionally analogous to a sympathetic ganglion; the adrenal medullary cells are directly innervated by the sympathetic preganglionic neurons that are located in the IML at the T5-T9 level. The pregangli-onic fibers pass through the sympathetic chain, exit through the greater splanchnic nerve without synapsing on neurons in the celiac ganglion, and innervate the adrenal medulla. The preganglionic fibers arising from the neurons located in the IML at T10-T11 also contribute to the sympathetic innervation of the adrenal medulla. These preganglionic fibers pass through the sympathetic chain, exit through the lesser splanchnic nerve without synapsing in the celiac ganglion, and innervate the adrenal medulla (Fig. 22-7). Acetylcholine is the transmitter released at the sympathetic preganglionic terminals innervating these cells. These cells secrete epinephrine (about 80%) and a small percentage (about 20%) of norepinephrine directly into the blood stream.
FIGURE 22-7 Autonomic innervation of the adrenal gland and kidney (see text for details). Red = sympathetic nervous system; Blue = parasympathetic nervous system. Solid lines = preganglionic fibers, dotted lines = postganglionic fibers. T = thoracic spinal segment; IML = intermediolateral cell column.
A rare catecholamine-secreting tumor of the neuroectodermal chromaffin cells is known as pheochromocytoma. These tumors occur in the adrenal medulla in a majority (85%) of these cases. Other major extra-adrenal sites where these tumors may be present include chromaffin cells associated with sympathetic nerves in the chest, abdomen, and pelvis. The tumors present in patients with pheochromocy-toma contain secretory granules that release catecho-lamines, which elicit sustained or paroxysmal hypertension. Other disorders caused by excess circulating catecholamine concentrations include stroke, myocardial infarction, cardiac arrhythmias, and shock. Pheochromocytoma can be cured by surgical removal of the tumor. Phenoxybenzamine or prazosin (alpha-adrenergic receptor blockers) or calcium channel blockers (e.g., verapamil) are used to control hypertension in these patients. Beta-adrenergic receptor blockers (e.g., propranolol) are used to prevent or treat supraventricular arrhythmias when present in these patients. For differential diagnosis of patients with primary hypertension and pheochromocytoma, an antihypertensive drug, clonidine, is administered orally. In patients with primary hypertension, plasma norepinephrine levels are decreased within 3 hours of the administration of clonidine, whereas this response is not observed in patients with phe-ochromocytoma.
Kidney
Sympathetic Innervation
The sympathetic preganglionic neurons are located in the IML at the T5-T9 level. The preganglionic fibers pass through the sympathetic chain, exit through the greater splanchnic nerve, and synapse on neurons in the celiac ganglia. The postganglionic fibers from the celiac ganglia innervate the kidney (Fig. 22-7). Sympathetic activation is believed to cause constriction of renal arteries.
Parasympathetic Innervation
The parasympathetic preganglionic fibers arising from the dorsal motor nucleus of vagus descend in the vagus nerves and enter the kidney along the renal artery (Fig. 22-7). It is believed that stimulation of these fibers causes vasodilation of the renal vascular bed.
Urinary Bladder
Sympathetic Innervation
The sympathetic preganglionic neurons innervating the urinary bladder are located in the IML at the T12-L2 level. The sympathetic preganglionic fibers pass through the sympathetic chain and emerge in the lumbar splanchnic nerves. These fibers then synapse on the postganglionic neurons located in the inferior mesenteric ganglion. The postganglionic fibers from this ganglion reach the urinary bladder through the hypogastric plexus (Fig. 22-8). Some preganglionic fibers from L1-L2 spinal segments descend in the sympathetic chain and synapse on postganglionic neurons in the hypogastric plexus. The postganglionic fibers from these neurons then innervate the urinary bladder (Fig. 22-1). Traditionally, it was believed that activation of sympathetic fibers innervating the bladder results in relaxation of the detrusor muscle and contraction of the sphincter located at the neck of the bladder. However, it is now believed that sympathetic fibers innervating the bladder are primarily distributed to the blood vessels in this organ.
The sympathetic nerves innervating the sphincter located at the bladder neck (sphincter vesicae) play a minor role in maintaining urinary continence by contracting this sphincter. However, these nerves also play an important role during ejaculation in the male. Ejaculation involves sympathetic activation. Sympathetic activation causes contraction of the sphincter vesicae during ejaculation and prevents seminal fluid from entering the bladder.
Parasympathetic Innervation
The parasympathetic preganglionic neurons innervating the bladder are located in the IML of the sacral spinal cord at the S2-S4 level. Their preganglionic axons exit from the ventral roots, travel in the pelvic nerves, pass through the hypogastric plexus, and synapse on postganglionic neurons located in the wall of the urinary bladder (Fig. 22-8). Activation of parasympathetic fibers results in contraction of the detrusor muscle of the bladder (smooth muscle of the bladder wall) and relaxation of the sphincter vesicae.
Afferent Innervation
Afferent impulses from the stretch receptors located in the bladder wall enter the spinal cord at T12-L2 levels via the hypogastric plexus. Such impulses also enter the spinal cord at S2-S4 levels via the pelvic nerve. Afferent information is transmitted to brainstem areas involved in coordination of bladder function.
Somatic Innervation
The external urethral sphincter consists of striated muscle that is innervated by alpha-motor neurons (somatic innervation) located in the ventral horn in the sacral segments S2-S4. This circumscribed region in the ventral horn is called Onuf’s nucleus (Fig. 22-8).
Micturition
During bladder filling, alpha-motor neurons in Onuf’s nucleus are active and keep the external urethral sphincter closed so that emptying of the bladder is prevented. During micturition (urination; voiding), the tonic activity of these alpha-motor neurons is temporarily inhibited, which results in relaxation of the external urethral sphincter. At the same time, parasympathetic neurons located in the IML at spinal sacral levels S2-S4, are activated to contract the detrusor muscle of the bladder wall. Thus, urination results from activation of sacral parasympathetic neurons innervating the bladder and temporary inhibition of alpha-motor neurons innervating the external urethral sphincter.
FIGURE 22-8 Autonomic innervation of the urinary bladder (see text for details). Red = sympathetic nervous system; Blue = parasympathetic nervous system. Solid lines = preganglionic fibers, dotted lines = postganglionic fibers. The green line represents somatic innervation. L= lumbar; S = sacral; T = thoracic spinal segment; IML = intermediolateral cell column.