Central Pathways
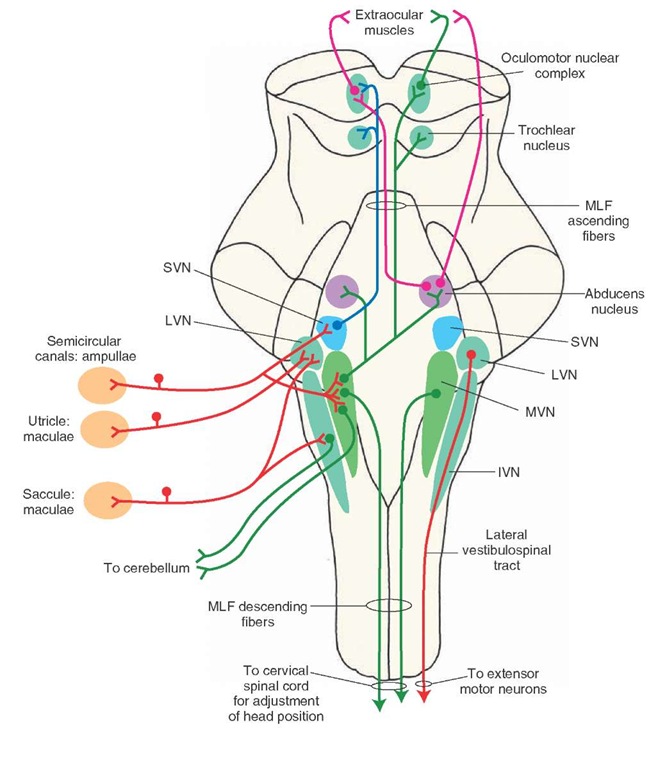
Although the vestibular (Scarpa’s) ganglion is referred to as a single ganglion, two vestibular ganglia are actually present (Fig. 17-8). The peripheral processes of the neurons located in the vestibular ganglion innervate the receptors (hair cells) in the vestibular labyrinth (maculae of the utricle and the saccule and ampullae of the semicircular canals). The central processes of these neurons travel in the vestibulocochlear nerve. The afferents from the vestibular labyrinth project to each of the vestibular nuclei located in the rostral medulla and the caudal pons. Afferents from the ampullae of the semicircular canals project to the superior vestibular nucleus (SVN) and rostral portion of the medial vestibular nucleus (MVN). Afferents from the maculae of the utricle and saccule terminate in the lateral vestibular nucleus (LVN). Some afferents from the macula of the saccule project to the inferior vestibular nucleus (Fig. 17-11). The excitatory neurotransmitter released at the terminals of the primary afferents from the vestibular labyrinth is believed to be glutamate or aspartate.
Ascending Vestibular Pathways
The ascending axons of the neurons located in the SVN enter the medial longitudinal fasciculus (MLF) rostral to the abducens nucleus and project ipsilaterally to the troch-lear and oculomotor nuclei. Fibers from the neurons located in the medial vestibular nuclei also ascend in the MLF and project bilaterally to the abducens nucleus, contralaterally to the trochlear and oculomotor nuclei (Fig. 17-11).
Cerebellar Afferent and Efferent Projections
An important source of inputs to the cerebellum arises from the vestibular system. Afferents can reach the flocculonodular lobe directly from the vestibular apparatus (direct vestibulocerebellar fibers) or indirectly mainly from the medial and inferior vestibular nuclei. Larger numbers of fibers reach the cerebellum via this indirect route. The LVN also receives both excitatory and inhibitory signals from the cerebellum. Excitatory inputs originate from the fastigial nucleus and inhibitory inputs to the LVN arise from Purkinje cells of the anterior lobe of the cerebellar cortex.
Vestibulocortical Pathway
It is believed that some axons from the secondary neurons located in the superior and lateral vestibular nuclei can communicate with the cerebral cortex. This may be achieved through bilateral projections of these nuclei via the MLF to the ventro-basal complex of the thalamus, and from these thalamic nuclei to the cortex (area 3a, which is adjacent to the primary motor cortex). This represents a possible pathway from the dorsal column-medial lemniscal system by which conscious perception of the position of the body in space and the sensation of movement is mediated. However, the precise sites in the cortex where conscious perception of vestibular sensation takes place have yet to be identified.
FIGURE 17-11 Central vestibular pathways. The afferents from the vestibular labyrinth project to each of the vestib-ular nuclei located in the rostral medulla and the caudal pons. Afferents from the ampullae of the semicircular canals project to the superior vestibu-lar nucleus (SVN) and rostral portion of the medial vestibular nucleus (MVN). Afferents from the maculae of the utricle and saccule terminate in the lateral vestibular nucleus (LVN). Some affer-ents from the macula of the saccule project to the inferior vestibular nucleus (IVN). See text for a description of ascending and descending pathways. MLF = medial longitudinal fasciculus.
Descending Vestibular Pathways
The lateral vestibulospinal tract arises from the LVN, descends through the brain-stem, and terminates in the ventral horn of both cervical and lumbar levels of the spinal cord. Lateral vestibulospi-nal fibers descend ipsilaterally and powerfully facilitate extensor motor neurons, using acetylcholine as the transmitter. Projections from the MVN descend bilaterally in the MLF as the medial vestibulospinal tract, terminate in the cervical spinal cord, and serve to adjust the position of the head and neck (Fig. 17-11).
In experimental animals, transection of the brain at the intercollicular level results in decerebrate rigidity. This condition is characterized by hyperactivity of extensor muscles of all limbs. Traumatic injuries, vascular disease, or tumors in the midbrain can cause similar symptoms in humans. The corticospinal, corticorubral, corticoreticular, and rubrospinal tracts are interrupted, whereas the facilitatory influences from the reticular formation and vestibulospinal tract on muscle tone remain intact in this situation. However, the inhibitory influences on muscle tone from the reticular formation are removed because they are dependent upon the descending impulses from higher centers. The net result of these alterations upon excitatory and inhibitory influences is an increase in the tone of antigravity muscles.
Vestibular System and Control Of Eye Movements
Briefly, the abducens nerve (CN VI) is involved in the lateral movement of the eye (i.e., abduction of the eye). The trochlear nerve supplies the superior oblique muscle, the primary action of which is to move the eye downward when it is located in a medial position. The oculomotor nerve (CN III) innervates the superior, medial, and inferior rectus muscles as well as the inferior oblique muscles. The action of the medial rectus muscle is to move the eye medially; the superior and inferior rectus muscles move the eye up and down, respectively; and the inferior oblique muscle elevates the eye when it is in the medial position. Besides CN III, IV, and VI, other brain structures are also involved in the control of eye movements.Movements of the eyes are influenced by ves-tibular nuclei that send projections to cranial nerve nuclei (the abducens, trochlear, and oculomotor nuclei).
Summary of the Functions of the Vestibular System
Movements of the head (e.g., tilting) trigger impulses (i.e., activates the hair cells in the maculae of the utricle and the saccule) that pass centrally in primary vestibular affer-ents to the vestibular nuclei and monosynaptically activate these neurons. The ascending and descending vestibular projections arising from vestibular neurons serve to coordinate the movements of the eyes, neck, and trunk in response to signals from vestibular afferents. These adjustments require contraction of some antigravity muscles, relaxation of other (flexor) muscles, with modifications of the head and eyes. These effects are achieved via projections of vestibular nuclei that innervate: (1) CN III, IV, and VI, mediating appropriate adjustment of the eyes in response to change in posture; (2) ventral horn cells of the cervical cord whose axons innervate head and neck muscles, producing changes in the position of the head;
(3) motoneurons of the cervical and lumbar cord, causing powerful excitation of the extensor musculature; and
(4) the flocculonodular lobe of the cerebellum, producing modulation of the descending pathways from the vestibu-lar nuclei and reticular formation, which control posture and muscle tone.
Clinical Disorders Associated With the Vestibular System
Nystagmus
Nystagmus refers to repetitive movements of the eyes produced by movements of the visual field. As indicated earlier, movements of the eyes are influenced by the vestibular nuclei (the lateral, superior, and medial vestibular nuclei) that send projections to the cranial nerve nuclei (oculomotor, abducens, and trochlear nuclei). Movement of the head in one direction results in the movement of the eyes in the opposite direction so that the eyes are fixed on an object. When the head and the body rotate, the eyes move in a direction opposite to that of the rotation. They remain fixed on an object until it is out of the field of vision. Then, the eyes move rapidly in the same direction as the rotation (called saccadic movement) and fix on another object until the latter is also out of the field of vision. Thus, there is an initial slow movement of the eyes in a direction opposite to that of the rotation, which is followed by a rapid movement in the direction of rotation. The slow movement of the eyes is controlled by vestibular nuclei and involves the MLF, whereas the saccadic movement is controlled by the paramedian pontine reticular formation (i.e., pontine gaze center). This pattern of eye movements is called nystagmus or the vestibulo-oculomotor reflex. Nystagmus in the absence of movements of the visual field indicates the presence of a lesion in the brainstem or cerebellum.
Nystagmus characterized by equal velocity in both directions is pendular nystagmus. In jerk nystagmus, there is a slow phase of movement that is followed by a fast phase in the opposite direction. The direction of the fast phase of movement is used to specify the direction of the jerk nystagmus. Thus, if the movement of the fast phase is toward the left, it is referred to as leftward-beating nystagmus.
Disorders of the vestibulo-ocular pathways in patients complaining of dizziness or vertigo (see next section) is tested using a caloric test. For this test, first an otoscopic examination is performed to ensure that the tympanic membrane is not perforated. Then the patient is placed in a supine position, and the head is elevated 30 degrees to bring the lateral semicircular canal into the upright position. Subsequently, either warm (44°C) or cold (33°C) water is introduced into the external auditory canal for 40 seconds. The interval between the irrigation with warm and cold water is at least 5 minutes. In an individual without disorders of the vestibulo-ocular pathways, cold water produces the fast phase of nystagmus beating in the opposite side in which the water was introduced, whereas warm water produces nystagmus beating in the same side in which the water was introduced. This relationship is described by the mnemonic COWS ("cold opposite, warm same"; or "cold water produces fast phase of nystagmus beating in the opposite side, whereas warm water produces nystagmus beating in the same side"). If there is a unilateral lesion in the vestibulo-ocular pathway, nystagmus will be either attenuated or abolished on the side ipsilateral to the lesion.
Vertigo
In this condition, the person has a sensation of turning or rotation in space in the absence of actual rotation. Usually, debris from the otolithic membrane, located in the saccule and utricle, accumulates at the ampulla of the posterior semicircular canal and adheres to the cupula, making it more sensitive to angular movement. Vertigo is often accompanied by nausea, vomiting, and gait ataxia. It can be caused by peripheral vestibular lesions that affect the labyrinth of the inner ear or the vestibular division of CN VIII. It can also be caused by central lesions that affect the brainstem vestibular nuclei or their connections. Vertigo due to peripheral lesions is usually intermittent, lasts for brief periods of time, and is always accompanied by unidirectional, but not vertical, nystagmus. Vertigo due to central lesions may or may not be accompanied by nystagmus. If nystagmus is present, it may be vertical, unidirectional, or multidirectional. Some HI receptor antagonists (e.g., the piperazine derivatives, cyclizine, and meclizine) and promethazine (a phenothiazine) have proved to be beneficial in the treatment of vertigo. Promethazine has the added advantage of relieving vomiting, which commonly accompanies vertigo.
Motion Sickness
Afferents from the vestibular system activate their projections to the reticular formation of the pons and medulla. Subsequent activation of autonomic centers results in motion sickness.
Inflammation of the Vestibular Labyrinth
This condition is referred to as vestibular neuronitis. Usually, there is no hearing loss. Typical symptoms include vertigo, postural imbalance, nausea, and nystagmus. The symptoms vary in severity and last for a brief time (a few days). Treatment is the same as for Meniere’s disease, which is described in the next section.
Meniere’s Disease
Meniere’s disease is characterized by intermittent, relapsing vertigo, which varies in severity (mild to debilitating) and duration (minutes to hours). In addition to these vestibular symptoms, the patient may suffer from hearing disorders, such as tinnitus (ringing noise in the ears) and distorted hearing. The cause of this disease is unknown. Histopathological studies have shown that there is an excessive accumulation of the endolymph, edema of the spaces containing the endolymph, and damage to the hair cells. Accumulation of the endolymph is most likely caused by poor drainage of this fluid from the membranous labyrinth. Recall that endolymph is normally drained by the endolymphatic duct into the endolymphatic sac, where it is resorbed into the cerebrospinal fluid. There is no effective treatment for this disease. In some patients, administration of steroids or diuretics relieves the symptoms probably by reducing edema of the lymphatic spaces. Treatment with HI receptor antagonists (e.g., meclizine) has also proved beneficial in this condition. In patients suffering from severe vertigo, destruction of hair cells by the antibiotic streptomycin is attempted. In other extreme cases, the affected labyrinth is surgically removed.
Clinical Case
History
Francine is a 42-year-old woman without any prior medical problems. For several weeks, she believed that she had an ear infection because she had some loss of hearing and ringing in her right ear; she felt slightly unsteady and thought that her mouth was drooping slightly on the right side. She consulted her physician and was referred to a neurologist immediately.
Examination
Upon examination,the neurologist noted asymmetry in Francine’s face.Her mouth did not elevate as much on the right side as it did on the left.There was a significant hearing deficit in the right ear. When a tuning fork was placed on her forehead, she only heard the vibration in her left ear. Bone conduction, as measured by the tuning fork, was lesser than air conduction in the right ear. There was rhythmic jerking laterally of Francine’s right eye when she was asked to look to the right. There was also some mild insensitivity to a pinprick on the right side of her face. The neurologist ordered a magnetic resonance imaging (MRI) scan of her brain.
Explanation
Francine’s MRI scan revealed a right-sided acoustic neuroma,a cerebellopontine angle tumor arising from the Schwann cells of the vestibulocochlear nerve. It causes dysfunction of the vestibulocochlear nerve, including hearing loss; nystagmus (jerking of eye movements when looking laterally); and unsteadiness, usually vertigo (a spinning or falling sensation). Because the tumorsareoften large enough to involve other structures in the cerebellopontine angle, including the fifth and seventh nerves, there is often dysfunction of these nerves as well. This is manifested in Francine’s case as Bell’s palsy or peripheral seventh nerve dysfunction including facial weakness involving the forehead. Additionally, the fifth cranial nerve is partially involved, manifesting its dysfunction as numbness on the right side of the face. The tumor may be pressing on the spinotrigeminal tract or may involve CN V directly if the tumor is large enough.
SUMMARY TABLE
Central Auditory and Vestibular Pathways
|
Receptors |
Sensory Neurons |
Pathways |
|
|
|
Central Auditory Pathways |
|
Hair cells in the organ ofCorti innervated by the peripheral processes of the bipolar neurons of the spiral ganglion |
Spiral (cochlear) ganglion |
1. Cochlear nerve (central processes of bipolar neurons in the spiral ganglion) joins the vestibular nerve to form the vestibulocochlear nerve (CN VIII) |
|
2. Vestibulocochlear nerve splits into cochlear and vestibular branches at the medullopontine angle of the brainstem; the cochlear branch enters the brainstem at the level of rostral medulla and projects to dorsal and ventral cochlear nuclei |
||
|
3. From the dorsal cochlear nucleus, some axons of the second-order neurons ascend and synapse on the ipsilateral superior olivary complex (located in the pons); other axons cross to the contralateral side in the pontine tegmentum as dorsal acoustic stria and then ascend and synapse on neurons in the inferior colliculus (located in caudal midbrain) |
||
|
4. Axons of both dorsal and ventral cochlear nuclei form the intermediate acoustic stria, which also cross to the contralateral side in the pontine tegmentum, ascend, and synapse on neurons in the inferior colliculus; axons of the second-order neurons in the ventral cochlear nucleus form the ventral acoustic stria (trapezoid body), which cross to the contralateral side in the mid-pons and synapse in the superior olivary complex; some axons of the second-order neurons in the ventral cochlear nucleus synapse in the ipsilateral superior olivary complex in the mid-pons |
||
|
5. Axons of the third-order neurons from the superior olivary complex ascend bilaterally in the lateral lemniscus (most of the axons ascend in the contralateral lateral lemniscus) and project to the nucleus of the lateral lemniscus at the level of the pons-midbrain junction; the neurons in the nucleus of lateral lemniscus project to the inferior colliculus |
||
|
6. Auditory information is relayed to the medial geniculate nucleus of the thalamus (located in the caudal aspect of the thalamus and proximal to the midbrain) |
|
Receptors |
Sensory Neurons |
Pathways |
|
|
Central Auditory Pathways |
|||
|
7. Medial geniculate nucleus relays precise information regarding the intensity, frequency, and binaural properties of the sound to the primary auditory cortex (located in the transverse temporal gyri of Heschl) of the medial aspect of the superior temporal gyrus 8. One of the secondary auditory areas includes Wernicke’s area, which is important for interpretation of the spoken word |
|||
|
Central Vestibular Pathways |
|||
|
Hair cells in the ampullae of semicircular canals and maculae of saccule and utricle |
Hair cells are innervated by the peripheral processes of the vestibular (Scarpa’s) ganglion |
1. Central processes of bipolar neurons in the Scarpa’s ganglion travel in the vestibular nerve, which joins the cochlear nerve to form the vestibulocochlear nerve (CN VIII) 2. Vestibulocochlear nerve splits into cochlear and vestibular branches at the medullopontine angle of the brainstem 3. Afferents from the ampullae of the semicircular canals project to the SVN and MVN 4. Afferents from the maculae of the utricle and saccule terminate in the LVN;some afferents from the macula of the saccule project to the IVN 5. Neurons in the SVN enter the MLF and project ipsilaterally to the trochlear and oculomotor nuclei 6. Neurons in the trochlear and oculomotor nuclei innervate the extra-ocular muscles 7. Neurons in the MVN ascend in the MLF and project bilaterally to the abducens nucleus.and contralateral^ to the trochlear and oculomotor nuclei 8. Afferents from MVN and IVN project to the flocculonodu-lar lobe of the cerebellum 9. Descending axons from the neurons in the LVN form the lateral vestibulospinal tract and project to the extensor motor neurons in the spinal cord 10. Descending axons of neurons in MVN travel in the MLF and project to the cervical spinal cord for adjustment of position of the head |
1. Movements of the head activate hair cells in the maculae (utricle and sac-cule);their afferents activate vestibular neurons 2. Ascending and descending vestibular projections arising from vestibular neurons serve to coordinate the movements of the eyes, neck, and trunk 3. These adjustments require contraction of some antigravity muscles, relaxation of other (flexor) muscles, with modifications of the head and eyes 4. These effects are achieved via projections of vestibular nuclei to (1) oculomotor,trochlear,and abducens nuclei, which mediate adjustments of the eyes in response to change in posture; (2) ventral horn cells of the cervical cord whose axons innervate head and neck muscles, producing changes in the position of the head; (3) motoneurons of the cervical and lumbar cord, causing powerful excitation of the extensor musculature; and (4) theflocculonodular lobe of the cerebellum, producing modulation of the descending pathways from the vestibular nuclei and reticular formation, which control posture and muscle tone |
CN = cranial nerve; IVN = inferior vestibular nucleus; LVN = lateral vestibular nucleus; MLF = medial longitudinal fasciculus; MVN = medial vestibular nucleus; SVN = superior vestibular nucleus.