Securing Devices
Once an endotracheal tube is placed, it is important that it be secured to keep it from moving out of the trachea. Numerous devices, such as the Thomas tube holder (Figure 23-12), are available commercially. In addition, many other ties have been used and can be equally effective. Regardless of the device or technique used to secure the endotracheal tube, it is important that the endotracheal tube not be able to move. Although taping the endotracheal tube to a patient’s face may be an acceptable practice in an operating room setting where the patient is not moved during the procedure, it is not sufficient for the prehospital environment. The risks of accidental tube dislodgment during patient movement are high. Not only is it important to secure the tube with an adequate device or technique, but it is also important to place a cervical collar to minimize neck extension and flexion.6 However the Paramedic plans to secure the neck, it is important that the equipment be prepared prior to the intubation.
Secondary Confirmation Equipment
Although the process of confirming tube placement will be described later, it is important that the Paramedic prepare his equipment for tube placement confirmation prior to beginning intubation. The three most commonly accepted methods of confirming endotracheal tube placement in the prehospital environment are auscultation, esophageal detection devices (EDD), and end-tidal carbon dioxide measurement. Visualization of the endotracheal tube passing through the vocal cords, although valuable and highly recommended, may not be possible due to other factors (e.g., traumatic airway, use of a elastic gum bougie, or nasotracheal intubation).
Figure 23-12 Thomas tube holder.
Auscultation of lung sounds, listening to the lung fields with a stethoscope, is a commonly accepted technique for assessing endotracheal tube placement. The only equipment necessary for this is a stethoscope. Therefore, a stethoscope should be immediately available. Although auscultation of the axilla alone to detect esophageal intubation is only 85% sensitive (and therefore misses 15% of esophageal intubations), the combination of auscultation over the epigastrium and in the axilla, when sounds can be well heard, has been shown to be 100% sensitive (detected all) for detecting esophageal intubation.
Esophageal intubation detection devices should also be used to confirm endotracheal tube placement. Two major styles of these devices exist: self-inflating bulbs and syringe style aspirators (Figure 23-13). These devices operate on the principle that the esophagus is composed of soft, floppy musculature while the trachea is held open by rings of cartilage. Therefore, if suction is applied to an endotracheal tube placed in the esophagus, the walls of the esophagus will collapse on the tip and prevent inflation. Conversely, the trachea will be held open by cartilaginous rings. Therefore, the esophageal intubation detection device should inflate rapidly and completely with air.
A number of studies have been performed on both the syringe type and self-inflating bulb devices. The results are encouraging for its use. In several studies,8-11 all of the esophageal intubations were detected. Although there are reports of the devices failing to detect esophageal intubations in patients with massive gastric insufflations,12 this has not been seen universally. The greatest limitation seems to be that the devices will often indicate an esophageal intubation when, in fact, the tube is actually in the trachea. This can occur when the tip of the tube is on the carina or pushed against the trachea’s wall. In addition, in patients with limited functional residual capacity—such as those in CHF, adult respiratory distress syndrome, or the morbidly obese—the devices may inflate slowly or with resistance.11,13 Therefore, the devices must be used in conjunction with other methods. To prepare the equipment, the Paramedic needs only to open the packaging.
Figure 23-13 Esophageal detector devices.
End-tidal carbon dioxide (ETCO2) measurement and monitoring has become a standard method of both confirming endotracheal tube placement and monitoring patient status, ventilation, and continuing tube placement.14 Carbon dioxide is a colorless, odorless gas that is produced during cellular metabolism. It is the primary exhaled waste product and its concentration in the exhaled respiratory gasses depends on adequacy of ventilation and circulation. End-tidal carbon dioxide measurement is used to assess endotracheal tube positioning and to monitor the adequacy of ventilation. The three classes of end-tidal carbon dioxide measurement are colorimetric measurement, capnometry, and capnography.
End-tidal carbon dioxide monitoring, in all of its forms, has been demonstrated to be a reliable and highly sensitive method for assessing endotracheal tube placement and monitoring tube placement over time.15-19 End-tidal carbon dioxide monitoring has become the gold standard of confirming endotracheal tube placement. There are, however, conditions which can limit its reliability. Therefore, it is important to understand their impact on the use of these devices. Perhaps the most fundamental limit is that the patient must be producing carbon dioxide in order to exhale it. In patients in cardiac arrest, the lack of exhaled carbon dioxide may be mistaken for an esophageal intubation.20 Of much more concern, however, is the risk of mistaking an esophageal intubation for a tracheal intubation. Bag-mask assembly ventilation with gastric insufflations,21 ingestion of carbonated beverages and antacids,22 and hypopharyn-geal endotracheal tube placement23 have all been shown to produce waveforms that would indicate tracheal intubation. However, with the exception of hypopharyngeal placement, after six ventilations (approximately 30 to 60 seconds of ventilation), the waveforms diminish and eventually vanish. Therefore, end-tidal carbon dioxide measurements should always be accompanied by other methods of assessing endo-tracheal tube placement.
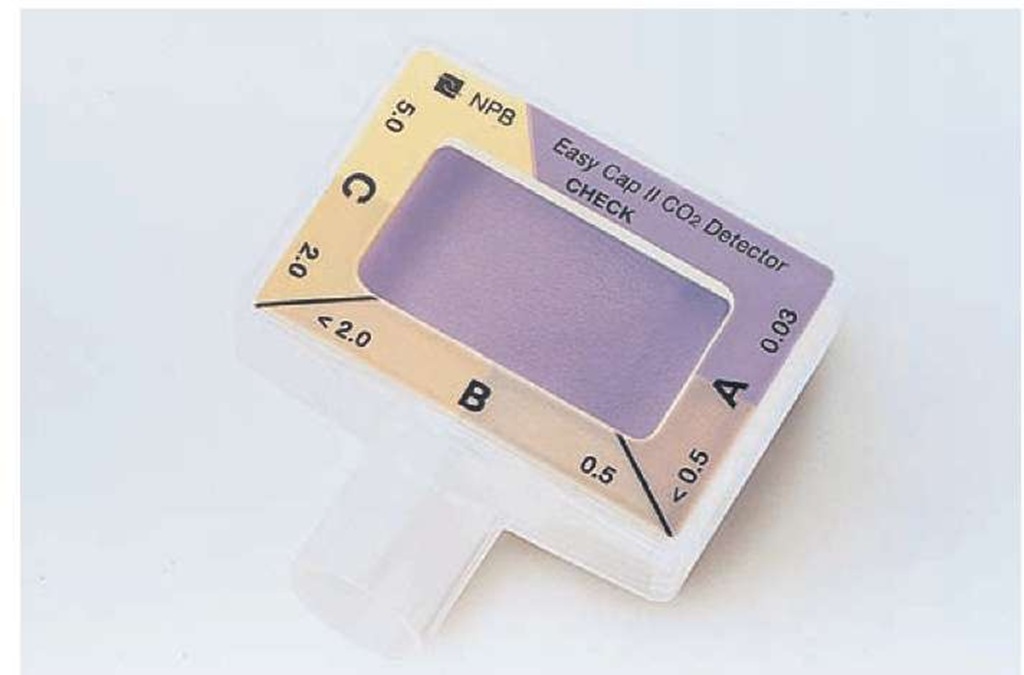
The least expensive, and probably most commonly used, device for measuring end-tidal carbon dioxide is the colorimetric device (Figure 23-14). These devices are simply encapsulated pieces of litmus paper over which the exhaled breath flows. When carbon dioxide is in the presence of water, it forms carbonic acid; the pH sensitive litmus paper in the colorimetric device detects this acid and changes color. These devices are as reliable as infrared cap-nometry and capnography for detecting esophageal and tra-cheal intubations20 and are reliable in infants and children larger than 15 kg.24 The devices are designed to be attached between the 15 mm adapter on the endotracheal tube or an alternative airway device and the BVM. Some manufacturers produce bag-mask assemblies with colorimetric ETCO2 devices built into the exhalation valves. When CO2 is < 0.5%, the paper is purple. When the CO2 is between 0.5% and 2.0% of the exhaled gas, the paper becomes tan. Finally, when the exhaled CO2 is > 2%, the paper turns yellow. Over time (approximately two hours for most in-line devices), the paper turns permanently yellow. Exposure to water, vomit, pulmonary secretions, medications, and so on, will hasten the deactivation of the device. Preparation of the colori-metric end-tidal CO2 monitor involves simply opening the packaging.
Figure 23-14 Colorimetric end-tidal carbon dioxide detector.
The remaining two classes of monitoring—capnometry and capnography—are, outside of the operating room, based on infrared analysis of exhaled gasses. By shooting an infrared beam through a sample of exhaled gas, it is possible to measure the amount of CO2 in the sample based on the absorption of light in the correct wavelength. The infrared beam and sensor can either be attached directly to the gas exhaust stream, called mainstream or in-line monitoring, or can be housed in a device that takes a small sample from the exhaled gasses, called side-stream or microstream monitoring.
Although mainstream measurements have the advantage of being instantaneous, the probes are more vulnerable to breakage and are more expensive. Sidestream devices protect the infrared sensors, but they have a delay in measuring due to the distance the gas sample must travel from the exhalation to the sample chamber.
Microstream devices have less of a delay than standard sidestream devices. Microstream devices may also be better suited for use in pediatric patients with very small tidal volumes than standard sidestream devices or bulky mainstream devices that can kink an endotracheal tube.25 Regardless of the sampling system, however, the data interpretation and display methods differentiate between capnometry and capnography.
Devices that perform capnometry give a single, numeric peak reading of the exhaled CO2. These monitors are usually considerably less expensive than capnography devices although they are also much more expensive than disposable colorimetric caps. Most of these devices have a numerical as well as a bar graph display. Although they do not display trends over time nor show a graph of the exhalation curve, if the Paramedic records the peak ETCO2 over time it is possible to collect trending data. In addition, these devices are usually equipped with an apnea alarm and can alert the Paramedic to sudden changes in ventilatory function. Preparation of the equipment for use involves assuring that there is sufficient power. For a mainstream device, the probe must be attached to the monitor and an adapter that connects to the endotra-cheal tube (or alternative airway device) which should be attached to the probe. Sidestream and microstream monitors will have an adapter with a sampling tube that attaches to the exhalation stream.
End-tidal capnography gives the most information to the Paramedic. While numeric values for peak and trough ETCO2 levels are displayed, the monitor also displays a graph of the exhalation curve (Figure 23-15). This graph allows for trending over time; demonstration of changes associated with complications such as displaced, kinked, and occluded tubes; and respiratory mechanics.19 Capnography monitors are by far the most expensive, although they are often integrated into other multifunction devices such as cardiac monitors. Preparation of these devices for use, as with the capnometer, depends on whether the capnographer is a mainstream or sidestream/microstream device.
Rescue Devices
For a patient requiring airway and ventilatory assistance, the ideal situation is placement of an endotracheal tube. However, there will always be scenarios in which endotracheal intubation will not be possible. A review of the airway management algorithm clearly demonstrates that, after a third failed endo-tracheal intubation attempt, the Paramedic should strongly consider another approach to airway management. One class of rescue devices available are placed blindly and provide an airway that is superior to face-mask ventilation, yet not as protective as an endotracheal tube. These devices are collectively called supraglottic airway devices or blind insertion airway devices (BIADs). The most common supraglottic devices are the King LTS-D airway, the esophageal tracheal Combitube (ETC or Combitube), and the laryngeal mask airway (LMA). Although the esophageal obturator airway (EOA) and esophageal gastric tube airway (EGTA) were commonly used before the advent of the supraglottic airways, the need to maintain an adequate mask seal and inability to protect the trachea have decreased the use of the EOA and EGTA.
Figure 23-15 Capnography waveform.
The King LTS-D airway (Figure 23-16) is one example of a supraglottic airway. It is designed to be placed in the esophagus and seal off the pharynx and esophagus with two balloons filled through a single port. A standard BVM adapter at the end of the device is used to ventilate the patient via small holes located between the balloons. A channel located in the anterior between the two balloons allows the use of an elastic gum bougie or endotracheal tube exchanger to replace the device with a standard endotracheal tube. Finally, a posterior lumen allows for passage of a nasogastric tube into the stomach once the King airway is in place, allowing stomach decompression. Due to the ease of use, this device is becoming popular in the prehospital community.
The laryngeal mask airway (Figure 23-17), a blind rescue airway device, was originally designed for use in the operating room.
Figure 23-16 King LTS-D airway.
Figure 23-17 Larnygeal mask airway.
Introduced in the mid-1980s, this device was designed to be used in situations where face-mask ventilation was inappropriate but the invasiveness of endotracheal intubation was not necessary.26 Although not originally designed as a "difficult airway" or "rescue" device, its potential was recognized early on. In the pilot study on its use, two of the patients were classified as having potentially difficult airways.27 Subsequent studies and clinical experience have demonstrated that the LMA adequately fills the role of a blind insertion airway rescue device in emergency airway management.28 Furthermore, introduction of devices such as the intubating LMA (ILMA) and disposable LMAs (LMA Unique®) have expanded the role of the LMA in prehospital airway management.
The laryngeal mask airway, in essence, moves the mask of face-mask ventilation from the face to the opening of the larynx. The LMA is composed of a single lumen tube with a standard 15 mm adapter at the proximal end and an inflatable mask at the distal end. The mask is designed to cover the opening of the larynx and, with the mask inflated, provide a seal. The intubating LMA, in addition to placing the mask over the larynx, is designed to pass an endotracheal tube through the lumen and direct it into the trachea. The LMA Unique®, as a disposable device, is most likely to be used in the prehospital environment. The LMA does require some preparation before use. Once it is removed from the package, the mask should be inflated to assure that it holds air. The LMA mask must then be pressed against a firm surface and the air aspirated from the mask. This causes the rim of the mask to fold backwards and allows for easier placement. Finally, the distal tip of the mask should be lubricated to improve ease of placement.
The design of the esophageal-tracheal Combitube (ETC) (Figure 23-18) reflects a response to the complications associated with the esophageal obturator airway (EOA) and the esophageal-gastric tube airway (EGTA). Like the
Figure 23-18 Esophageal-tracheal Combitube.
EOA and EGTA, the ETC is placed into the esophagus; however, tracheal placement of the ETC is possible. The double-lumen design allows for endotracheal as well as esophageal intubation.
The Combitube is a double-lumen device with two separate and distinct lumens, a proximal and distal lumen named by where they exit from the tube. Each lumen has a standard 15 mm connector at the proximal end to allow attachment to a ventilation device. Each has two cuffs: a large proximal cuff designed to seal the hypopharyngeal portion of the airway and a smaller distal cuff designed to seal the esophagus or trachea, depending on the placement.
There are several advantages and disadvantages to the use of supraglottic airway devices. Since they can be passed blindly, no special equipment is needed other than the device itself. The Combitube has been demonstrated to cause less C-spine movement than conventional endotra-cheal intubation,31 which may be clinically significant in the patient with known or suspected C-spine injury. The devices are easy to place and have success rates of almost 100%.32 Placement is easier with these devices than with standard intubation when patients are in unusual positions.33 There are, however, multiple disadvantages to these devices. The King airway and Combitube are currently only available for adult patients. They must be inserted orally and, when placed in the esophagus, are difficult to intubate around, owing to their large size and rigidity. Furthermore, caustic ingestions and known esophageal trauma or disease are contraindications to use of these devices. Finally, they are considerably more expensive than standard endotracheal tubes.
Both devices are intended for esophageal placement, which occurs approximately 90% to 99% of the time. In the esophageal position, the distal cuff seals the esophagus while the proximal cuff seals the hypopharynx. The proximal lumen ventilates through a number of small holes between these two cuffs. Since the opening to the larynx lies between these cuffs, ventilatory gasses passing through the proximal lumen can only go into the larynx and subsequently to the lungs. There are some limitations to the esophageal placement. Most importantly, epiglottic, perilaryngeal, and laryngeal injury or deformity (burns, trauma, edema, etc.) can prevent effective ventilation. Furthermore, respiratory secretions and bleeding between the two cuffs will be aspirated. Finally, medication administration and deep suctioning of the lungs are not possible with esophageal placement.
It is possible to obtain endotracheal placement of the Combitube. Anecdotally, increased rates of tracheal placement occur with well-performed cricoid pressure. When the devices are placed in the trachea, the distal cuff serves to seal the trachea (like the cuff of an endotracheal tube) while the proximal cuff helps stabilize the device. Ventilation is performed through the distal lumen that opens at the end of the tube, distal to the smaller cuff. Tracheal placement allows the device to function as an endotracheal tube and all procedures and medications normally performed with an endotracheal tube can be performed with the Combitube. In contrast, the King airway is not designed to be used if placed in the trachea. If tracheal placement of the King airway is suspected, immediately remove the device.
Preparation of these devices is similar to that of an endotracheal tube. They must be removed from their packages and the cuffs inflated to test their integrity and the functioning of the valves. For the King airway and Combitube, this is done with the syringes that are prepackaged with the device. The distal end of the tube should be lubricated with a water-soluble lubricant and the devices returned to the packaging.