ABSTRACT
Mobile information and communication technologies are advancing rapidly and provide great opportunities for home monitoring applications in particular for outpatients and patients suffering from chronic diseases. Because of the ubiquitous availability of mobile phones, these devices can be considered as patient terminals of choice to provide a telemedical interaction between patients and caregivers. The most challenging part still is the patient terminal, that is, to offer the user a method to enter measured data into a system as well as to receive feedback in a comfortable way. The objective of this topic is to present and compare solutions for mobile-phone-based patient terminals as developed by us and other authors.
INTRODUCTION
“Telemonitoring is defined as the use of audio, video, and other telecommunications and electronic information processing technologies to monitor patient status at a distance” (Field, 1996, p. 271). This concept may be particularly suitable in the management of chronic diseases where a close partnership as well as collaboration between patient and healthcare provider are essential. New paradigms such as prevention and patient empowerment promote the development of novel care approaches in which outpatient monitoring is a basic aspect.
Rapid advancements of information and communication technologies and the increasing availability of mobile phones open new perspectives in using these devices for tele-monitoring applications to deliver healthcare to people geographically remote from physicians or medical centers. The possibility to use the mobile phone for standard voice communication as well as for the transmission of a variety of multimedia information like text, audio, images, and videos makes it the communication interface of choice for patient-centered tele-monitoring applications.
The basic idea is to track patients’ personal health status using the mobile phone as a patient terminal and to send the data to a remote monitoring centre. An automated monitoring process checks the values and gives feedback in order to guide the patient through the self-managing process and to turn the doctor’s or other caregiver’s attention to the patient when necessary by means of notifications and alerts. The most challenging part in this scenario still is the patient terminal, that is, to offer the user an easy method to enter measured data into a system as well as to get feedback of the current health status in a comfortable way.
This topic will focus on the usage of mobile phones in the management of chronic diseases and gives an overview of available technologies. Furthermore, it will present and compare already implemented mobile-phone-based home monitoring concepts as developed by us and other authors.
brief historical outline
Basically, tele-monitoring combines topics from the fields of medicine, information and communication technology, and computer science. Particularly, information and communication technologies have undergone rapid advancements over the past decades, driven by the needs of modern information society. Communication devices such as mobile phones or personal digital assistants (PDAs) became smaller and more powerful, and advanced from single-purpose stand-alone devices to multipurpose networked devices that make them usable for tele-monitoring applications indeed.
However, reviewing the literature, the exact date when tele-monitoring was first mentioned in healthcare is still unknown (Brown, 1995). Starting with the first words transmitted by telephone in 1876 by Alexander Graham Bell, communication technology was ready to be used to facilitate healthcare services. For example, William Ein-thoven, the father of electrocardiography (ECG), transmitted ECG signals over wired telephone lines in 1906 (Barold, 2003).
In the 1930s, when the telephone became standard equipment in households, it also became the mainstay of medical communication and remained a major element until today. Wireless communication technologies were invented at the same time. Around the time of World War I, radio communication was established in a wider area, and, around 1930, it was used in remote areas such as Alaska and Australia to transfer medical information (Zundel, 1996).
Besides pioneering efforts of a few physicians using off-the-shelf commercial equipment to overcome time and distance barriers, current tele-monitoring concepts originated from developments in the manned space-flight program introduced by the National Aeronautics and Space Administration (NASA) in the early 1960s (Brown, 1995). The main intention was to monitor physiological parameters like heart rate, body temperature, ECG, and oxygen and carbon-dioxide concentration of astronauts in space and transmit the data to earth in order to establish an understanding of the health and well-being of the astronauts while they were in orbit.
Nowadays, tele-monitoring is adjudicated an important role in health systems since for a number of indications the cost effectiveness and the medical benefits have been approved (Meystre, 2005). Moreover, there is still a driving force to improve outpatient care by shifting tasks from hospitals to patients’ homes, particularly in the management of chronic conditions, which will be discussed in detail in this topic.
MANAGING CHRONIC DISEASES
Chronic diseases are cited in literature as diseases that have one or more of the following characteristics: They are permanent, leave residual disability, are caused by nonreversible pathological alteration, require special training of the patient for rehabilitation, or may be expected to require a long period of supervision, observation, or care (National Library of Medicine, 2005).
Chronic diseases such as heart failure, hypertension, cancer, diabetes, and asthma were the major cause of death (59% of the 57 million deaths annually) and global burden of disease (46%) in 2004 (World Health Organization [WHO], 2005).
It is also obvious that chronic diseases tend to become more common with age. WHO reported that in 1998, 88% of the population in developed countries over 65 years old suffered from at least one chronic health condition. Since populations are aging worldwide and chronic diseases have a significant impact on healthcare systems, new strategies in prevention, early detection of illness pattern, and long-term treatment are needed.
To address the quality and effectiveness of healthcare services for chronic-disease management, the chronic care model was developed at the MacColl Institute for Healthcare Innovation in 1998 (Wagner, 1998). The model describes the transformation of healthcare from a system that is essentially reactive, responding mainly when a person is sick, to one that is proactive and focused on keeping a person as healthy as possible. Besides strategic and lasting changes in health systems, the model suggests enforcing patients’ central role in their care and self-management (Epping-Jordan, Pruitt, Bengoa, & Wagner, 2004).
Effective self-management support means more thanjust telling patients what to do. Because of the fact that neither the chronic condition nor its consequences are static, the process of self-management might be complex and patients are often overstrained. Thus, a close partnership between patients and caregivers is essential in order to guide the patient through the self-management process and to the best possible health status.
It is widely recognized that the monitoring of health-related parameters like blood pressure, blood glucose, or well-being in regular intervals is the central element in the strategy of an effective self-management of chronic conditions. Basically, monitoring is defined as periodic measurements that guide the management of a chronic or recurrent condition. It can have an impact on the improvement of therapy adherence, the better selection of treatments based on individual response, or the better titration of medication (Glasziou, Irwig, & Mant, 2005).
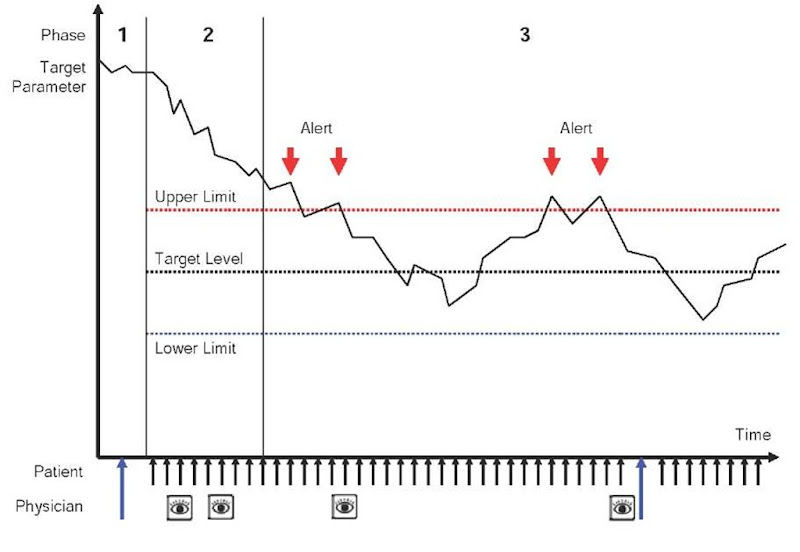
Depending on the target parameter and the phase of treatment, monitoring can be done by clinicians, patients, or both. The strategy of monitoring can be divided mainly into three phases shown in Figure 1. Blue arrows indicate visits at the physician’s office. The eye icon indicates tele-monitoring activity. Short, black arrows show the patient’s self-monitoring activity.
• Pretreatment. Monitoring before treatment is mostly performed at the physician’s office by the physician. The main goal is to access the patient’s current health status and to verify the need for a medical intervention. Beside standard measurements like the assessment of blood pressure, more complex diagnostic tests like blood tests or urine tests are performed to confirm decisions. At that stage, a person has to be accustomed to his or her new role as a patient in the patient- physician relation. Moreover, objectives of treatment, monitoring parameters, target levels, and their upper and lower limits should be well defined.
Figure 1. Three phases of monitoring (pretreatment, adoption, long-term treatment)
• Adoption. After establishing the target level, application of medication will be started in order to reach the objectives of treatment. Monitoring disease-related parameters, for example, blood pressure in case of hypertension, will show the effect of treatment in a representative way. In case of the necessity to titrate medication, monitoring has to be done very carefully and in shorter intervals to avoid abnormalities or the worsening of the health status.
• Long-term treatment. Although the target level has been reached periodically, monitoring is essential because the course of a chronic condition is rarely static. Overstepping or undershooting the predefined target level should be observed carefully. Additionally, alerts could be generated in order to turn the patient’s and physician’s attention to this special situation. Periods of problems can easily be identified via graphical representation. If noticed problems cannot be solved via tele-medical intervention, the patient has to be ordered to the physician’s office for further examination. However, the main objective of tele-monitoring is to detect illness patterns at the earliest possible stage in order to avoid emergency situations and hospitalization.
Today, patients are asked to track their key measures like blood pressure, heart rate, diabetes-relevant data, well-being, or side effects of medication by daily taking notes on a piece of paper, called a health-data diary. The captured data are expected to show trends in the illness patterns and to help the doctor to guide the patient to the best possible health status.
However, patients’ motivation for using the conventional method in self-management is often poor. This is hardly surprising since patients are often confronted with complex documents and instructions. On the other hand, paper-based diaries lack proper data representation, feed back, and timely delivery of data. Therefore, an easy-to-use and patient-centered data-acquisition system is essential to guide the patient through data capturing and the complex process of self-management.
USING INFORMATION AND COMMUNICATION TECHNOLOGIES IN HOME MONITORING ENVIRONMENT
The effective management of chronic diseases requires a close partnership between the patient and healthcare provider, which can be supported by contemporary information and communication technologies (Celler, Lovell, & Basilakis, 2003). The timely delivery of data is indispensable to detect an aggravation in illness patterns and to ensure appropriate medical decisions at the earliest possible stage.
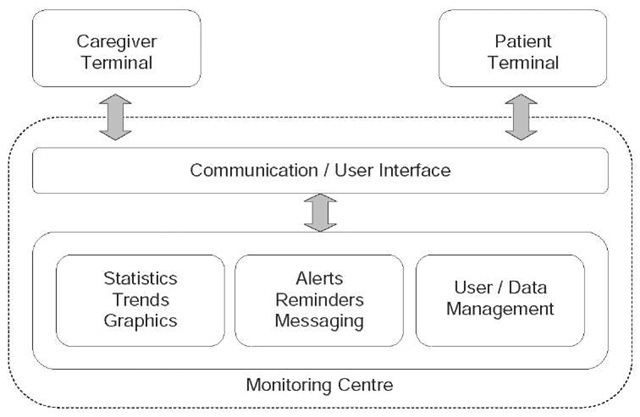
The basic idea is to track the patient’s personal health status using a patient terminal, and to transmit the data to a remote monitoring centre where the data are processed and trends, statistics, and graphical representations are generated. An automated monitoring process checks the values and gives feedback. When necessary, the doctor’s or other caregivers’ attention will be turned to the patient by the means of notifications or alerts.
In our research, we developed a home monitoring platform for regular and home-based measurement and transmission of health parameters like blood pressure, body weight, symptoms, and medication. The system, shown in Figure 2, has been built using mostly standard components and state-of-the-art Internet technology, and it comprises the following.
Monitoring Centre
A 24/7-accessible server system receives, stores, and processes the data. The results are forwarded to the caregivers in a standardized and easily comprehensible format. Central components are user and data management to ensure the security, integrity, and traceability of data. Role-based, hierarchical user management guarantees that only authorized users are able to view, edit, or enter data in the system.
Figure 2. Main components of a home monitoring platform
Patient Terminal
The patient terminal provides the user with an adequate communication interface for entering data into the system as well as to receive feedback or medical advice. Although the availability of PCs (personal computers) with Internet access is already high in developed countries, the use of computers still presents a barrier to the adoption of Web-based solutions, especially by the elderly and technically unskilled people. Hence, different solutions have been developed during the last years to give such users an easy-to-use and intuitive way for entering their health data comfortably using manual, automatic, or semiautomatic methods in conjunction with standard medical measurement devices.
caregiver Terminal
The Web-based caregiver terminal gives authorized people access to assigned patients and their data via PC or mobile Internet-enabled devices like PDAs or tablet PCs. Specially designed GUI (graphical user interface) components give the physician a quick overview and support straightforward navigation. Transmitted values as well as statistics, trends, and graphical representations can be accessed easily.
Statistics, Trends, and Graphics
An automated process analyses incoming data and generates statistics, trends, and graphical representation. Additionally, the process is able to check for alert conditions (limits given by the responsible physician) or to correlate the values with predefined patterns to identify abnormalities in the course of treatment.
Messaging System
In case of detected aberrance, notification messages will be sent to the physician or the patient via SMS (short-message service) or e-mail immediately in order to initiate further action. Additionally, it turned out that reminder messages are useful for patients and caregivers. The possibility to send interactive messages in several ways enforces communication between patients and caregivers.
communication and User Interface
Besides the possibility to access or enter data via a Web interface, interfaces to several wireless communication technologies such as WAP (wireless application protocol), SMS, and MMS (multimedia messaging service) are provided in order to send or receive data.
going wireless
A current trend in information and communication technologies is the convergence of wireless communication and computer networks as well as a moving from stand-alone, single-purpose devices to multipurpose network devices. Up to now, several studies have demonstrated that tele-monitoring using information and communication technologies on different integration levels – reaching from a simple telephone call to wearable or implantable sensor systems – can effectively assist patients in the management of care. Although the use of older approaches (telephone, fax) is still common, latest innovations in computer and network technologies can be considered for tele-monitoring applications to support the patient with a method to enter and transmit data in a comfortable way.
The Telephone as communication Interface
Telephone care services represent the oldest method to deliver medical advice to the patients’ homes. Nowadays, standard telephone lines are available in almost every household and even technically unskilled people are able to handle the telephone. For monitoring purposes, patients are contacted by a call centre to hand over their key measurements in predefined follow-up intervals. Specially trained personnel check the values against the patient’s history and predefined limits and give feedback in order to assist the patient in self-management.
The usage of telephone interventions in the management of outpatients suffering from chronic heart failure was demonstrated in the DIAL (randomised trial of telephone intervention in chronic heart failure) trial (GESICA, 2005): 1,518 patients with stable chronic heart failure and optimal treatment were enrolled in 51 centers in Argentina. The DIAL trial intervention strategy was based on frequent telephone follow-ups provided by nurses trained in heart failure. The purpose of interventions was mainly to educate and monitor the patients as well as to increase the patients’ adherence to diet and drug treatments. The results indicate that patients in the usual-care group were more likely to be admitted to the hospital for reasons of worsening and they were also more likely to die than patients in the tele-monitoring group who received telephone intervention. Moreover, patients in the intervention group showed a better quality-of-life score than patients randomized to the usual-care group.
Besides the possibility to use plain old telephone systems (POTS) for voice communication, they can also be used to access the Internet and network-based data services. Medical measurement devices like blood-pressure meters, blood-glucose meters, or scales equipped with modems can be connected to the POTS directly or by the means of a home terminal.
The Trans-European Network Home-Care Management Systems study (TEN-HMS) was the first large-scale, randomized, prospective clinical trial to decide if home-based tele-monitoring services for heart-failure patients are able to reduce hospitalizations and to improve patient well-being while reducing the overall costs of care (Cleland, Louis, Rigby, Janssens, Balk, & TEN-HMS, 2005). In total, 426 patients were randomized to the control group, nurse telephone-support group, or tele-monitoring group. The results indicate that patients randomized to the tele-monitoring group faced a reduced number of days spent in the hospital (minus 26%). Furthermore, it led to an overall cost saving compared to the nurse telephone-support group (minus 10%). Tele-monitoring also significantly improved survival rates relative to the usual-care group and led to high levels of patient satisfaction.
Mobile Phone as Communication Interface
Recent statistics indicate that the number of mobile phones throughout the world exceeded 1.5 billion in 2004 (CellularOnline, n.d.). Moreover, it is estimated that within a few years, about 70% of cell phones in the developed countries will have Internet access. Thus, mobile phones have become potential devices for serving as patient terminals in tele-monitoring applications. Mobile phones as well as communication technologies have undergone incredible changes and advancements during the last years. The amazing employment of mobile phones started in the 1980s when first-generation (1G) cellular systems were introduced. This technology was based on analog circuit-switched technology. Low data rates prevented this technology from being used for data transfer. Up to now, most of the 1G networks have been replaced by second-generation (2G) wireless networks, which are based on digital circuit-switched technologies. Several standards have been developed in different parts of the world: the Global System for Mobile Communication (GSM) technology in Europe, code division multiple access (CDMA) technology in the USA, and personal digital communication (PDC) in Japan. Second-generation wireless networks are digital and expand the range of applications to more advanced voice services and data capabilities such as fax and SMS at a data rate up to 9.6 kbps, which still makes it mostly impractical for extensive Web browsing and multimedia applications.
Through the years, several advanced techniques based on 2G networks were introduced such as general packet radio service (GPRS) and enhanced data rates for global evolution (EDGE). These technologies, also known as 2.5G networks, make it possible to use several time slots simultaneously when sending or receiving data, resulting in a significantly increased data rate (171 kbps for GPRS, 384 kbps for EDGE). The data packages are sent over the network using an IP (Internet protocol) backbone so that mobile users can assess services on the Internet.
The Universal Mobile Telecommunications System (UMTS) presents the third generation (3G) of wireless communication technology. The broadband, packet-switched transmission concept supports the transmission of text, digitized voice, video, and multimedia at data rates up to 2 Mbps. At the moment, users in real networks can expect performances up to 384 kbps for downloading and at least 64 kbps for uploading data. Third-generation systems are expected to have the following features: fixed- and variable-rate bit traffic, bandwidth on demand, asymmetric data rates in the forward and reverse links, multimedia mail storage and forwarding, the capability to determine the geographic position of mobile units and report it to both the network and the mobile terminal, and international interoperability and roaming (Tachakra, Wang, Istepanian, & Song, 2003).
In the course of rapid advances in communication technology and increased data rates, new multimedia services appeared that are the basis for further developments of mobile-phone-based applications for healthcare.
Short-Message Service
SMS allows sending and receiving text messages of up to 160 characters in length to and from mobile phones as defined within the GSM digital mobile-phone standard (Buckingham, 2000a). The text can comprise words or numbers or an alphanumeric combination. SMS is a store and forward service. This means that SMS messages are not sent directly from sender to recipient. Each mobile telephone network that supports SMS has at least one messaging centre to handle and manage the short messages.
To receive the text message on the server side, a mobile phone is connected to the server via standard interfaces such as RS232. Using the Hayes command set (Attention (AT) commands), the arrived messages can be accessed and stored in the database for further processing.
There are several reports on the use of SMS in medical application areas. SMS has been basically used for patient and appointment reminders. Outpatient clinics that are using SMS-based appointment reminder systems are seeing a reduction in missed appointments or “did not attends” (DNAs). It has been demonstrated that outpatient clinics that deployed SMS patient reminder systems saw DNA rates fall by as much as 30% even though less than 20% of patients chose to use the service (Research and Markets, 2005).
Besides the usage of SMS as a reminder service, SMS has also been applied in several medical application areas to transmit data from patients’ homes to a monitoring centre. In 2004, Ferrer-Roca, Cardenas, Diaz-Cardama, and Pulido presented the use of SMS for diabetes management. Twenty-three diabetic patients (18 to 75 years old) were asked to transmit data such as blood-glucose levels and body weight to a central server. The server automatically answered via SMS with a prerecorded acknowledgement, specific help, or warning messages when data were out of range. During an 8-month study period, an average of 33 SMS messages was sent per patient and month. Unfortunately, no medical benefit was reported. However, they conclude that SMS may provide a simple, fast, efficient, and low-cost adjunct to the management of diabetes at a distance.
Figure 3. WAP programming architecture. The application is stored on the content server and the requested pages are generated dynamically
On the other hand, medical benefit in asthma monitoring could be demonstrated by Ostojic, Cvoriscec, Ostojic, Reznikoff, Stipic-Markovic, and Tudjman (2005). Sixteen patients (24.6 +/- 6.5 years old) were asked to transfer peak expiratory flow (PEF) measurements at least three times a day during a 16-week study period. Patients randomized to the tele-monitoring group received a weekly adjustment by an asthma specialist based on the values sent to the monitoring centre. They reported that asthma overall was better controlled in the intervention group, according to their findings of reduced PEF variability.
Wireless Application Protocol
WAP is an open global standard for communication between mobile phones or other mobile devices and the Internet (Buckingham, 2000b).
WAP-based technology enables the design of advanced, interactive, and online mobile services, such as mobile banking, Internet-based news services, or even tele-monitoring applications.
The WAP standard is based on Internet standards like the hypertext markup language (HTML), extensible markup language (XML), and transmission control protocol/Internet protocol (TCP/IP). Basically, it consists of the wireless markup language (WML) specification, which is a markup language derived from HTML. However, WML is strongly based on XML, so it is much stricter than HTML. WML is used to create Web pages including text, images, user input, and navigation mechanisms that can be displayed on a WAP micro browser.
The WAP architecture consists of a WAP device, a WAP gateway, and a content server (Figure 3). The handheld WAP device communicates with the content server, which stores information and responds to user requests. The gateway in between translates and passes information between the device and the server. To access an application stored at the content server, a connection to the WAP gateway is initialized. Thereafter, the WAP request is converted to HTTP (hypertext transfer protocol) and forwarded to the content server.
Upon handling the request, the requested content is returned to the gateway, transformed into WAP, and sent back to the device to be displayed via the micro browser. The new version of WAP, WAP 2.0, is a reengineering of WAP using a cut-down version of the extensible hypertext markup language (XHTML) with end-to-end HTTP connection. This means that using WAP 2.0, the WAP gateway becomes dispensable.
A couple of authors (Hung & Zhang, 2003; Salvador et al., 2005) have already demonstrated tele-monitoring applications using WAP technology after WAP browsers became a standard feature of mobile phones. It is mentionable that besides demonstrating principal functionality in several pilot trials, only few clinical trials using WAP for patient monitoring have been mentioned in the literature yet.
For example, Italian researchers have shown that aftercare and patient communication might be improved if patients are asked to fill in daily questionnaires using WAP ontheirmobile phones (Bielli, Carminati, La Capra, Lina, Brunelli, & Tamburini, 2004). They developed the Wireless
Health Outcomes Monitoring System (WHOMS), which allows structured questionnaires to be sent to the patient by the medical management team. Each day, an SMS message was sent informing patients of the survey and giving a link to a WAP site accessible through a standard GPRS connection. Users were asked to rate symptoms such as pain, lack of energy, and difficulty sleeping. The collected data were viewable by the doctors in a graphical format that highlighted the patients’ states of health.
Although 42% of the patients failed to fill in the questionnaires mainly because of neophobia and unfamiliarity with the technology, the researchers concluded that health-outcome monitoring using mobile phones can be the method of choice for future developments in quality-of-life assessments. They address the need to develop more user-friendly communication terminals supported by upcoming technologies for mobile phones to increase the adoption rate.
In the course of our research, a lot of effort has been done to make WAP technology applicable for the broad usage in home monitoring applications and the management of chronic diseases.
Figure 4. Graphical user interface generated by WML guides the patient through the data-acquisition process
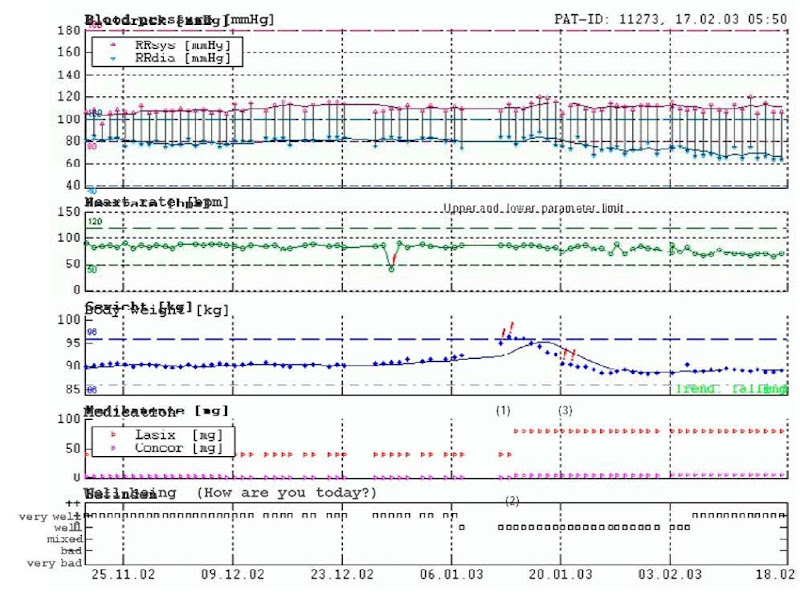
The aim of the Cardio-Memory study (Scherr, Zweiker, Kollman, Kastner, Schreier, & Fruhwald, in press) was to evaluate whether WAP technology would be an acceptable, feasible, and reliable option to provide tele-monitoring for patients with chronic heart failure or hypertension. In the course of a clinical pilot trial, 20 patients (mean age 50 +/- 14 years) were enrolled. Each participant was equipped with a mobile phone, an automatic blood-pressure device, and a digital weight scale. Patients were asked to measure their blood pressure, heart rate, and weight every day. After accessing the system with the micro browser, the menu promptly routed the patients through subsequent entry templates generated by WML syntax (Figure 4). Eventually, all data were sent to the central database at the remote monitoring centre for further processing.
Authorized physicians could access the data via a secure Web site at any time. The Web site provided the data of each patient in numerical format and graphical trend charts, including patient-specific upper and lower parameter limits. Furthermore, it allowed physicians to set automatic reminders: These computer-generated SMS messages reminded patients to take their medications, weigh themselves, measure blood pressure and heart rate, and to transfer the respective data to the secure server at the monitoring centre. Furthermore, the physician could individually configure an automatic warning system for each patient. If the patient’s values exceeded individually predefined vital parameter limits, physicians were notified immediately by a computer-generated SMS or e-mail warning. If an intervention (e.g., adjustment of medication dose) was indicated (for example, because a patient exceeded a vital parameter limit), the physician was able to contact the patient directly via mobile phone to confirm the parameters and ask the patient to make an adjustment in medication.
During the 3-month monitoring period, there were 2,040 data-transfer sessions (mean 102 +/- 43 per patient). Only 1 out of 20 patients dropped out after 25 days due to severely impaired vision. The Cardio-Memory system was evaluated through a questionnaire at the end of the study. Eighteen out of 20 patients rated the software as easy to operate, which allows us to conclude that overall patients’ acceptance with the system was high. The entire process (measurements and data transfer) took approximately 3 minutes to be completed. Moreover, patients felt that computer-generated reminders about missing data increased their compliance with the treatment regime.
An example of a successful tele-medical intervention of a patient suffering from chronic heart failure is shown in Figure 5. Cardiac decompensation caused a weight gain of more than 2 kg within 3 subsequent measurements and led to a patient alert (1). The physician contacted the patient and increased the diuretic dose (2). Subsequently, the patient lost weight and remained in stable conditions until the end of the observation period (3).
Following the promising results of the Car-dio-Memory trail, an advanced study was set up in October 2003 in order to evaluate WAP technology in the management of chronic heart failure (Scherr et al., 2005). In a randomised, prospective, multi-center study, 240 patients who had been admitted to the hospital because of heart failures will be randomised to either pharmacological treatment (control group) or to pharmacological treatment plus tele-medical care (telegroup). Telegroup patients are provided with a mobile telephone, a digital weight scale, and a fully automated blood-pressure device. During the follow-up period of 6 months, patients are asked to send their self-measurements using a WAP application on the mobile phone on a daily basis. Up to now, 65 patients (45 male, 20 female; 64 ± 11 years old) from six centers have been randomised, and 44 patients have completed the study so far. Three patients from the telegroup dropped out due to being not able to handle the monitoring system equipment, in particular, the mobile phone.
Figure 5. Trend chart of a patient monitored with Cardio-Memory
Intermediate results indicate that WAP-based tele-medical surveillance of patients with a recent episode of acute heart failure significantly contributes to an improvement of functional status and may be a promising tool to improve heart-failure therapy and reduce emergency situations and hospitalizations.
Java-Based Software Application Running on Mobile Phones
Java 2 Platform, Micro Edition (J2ME), the small footprint version of the Java technology, is optimized to run on memory-constrained devices like mobile phones, PDAs, and TV-set-top boxes. Each device category receives its own profile that includes a set of category-specific application program interfaces (APIs) and a configuration that consists of a minimum set of APIs and a Java virtual machine. In particular, mobile phones support the mobile information device profile (MIDP), which includes APIs covering the user interface, networking, persistent storage (a record-oriented database), security, and messaging (Sun Microsystems, 2002).
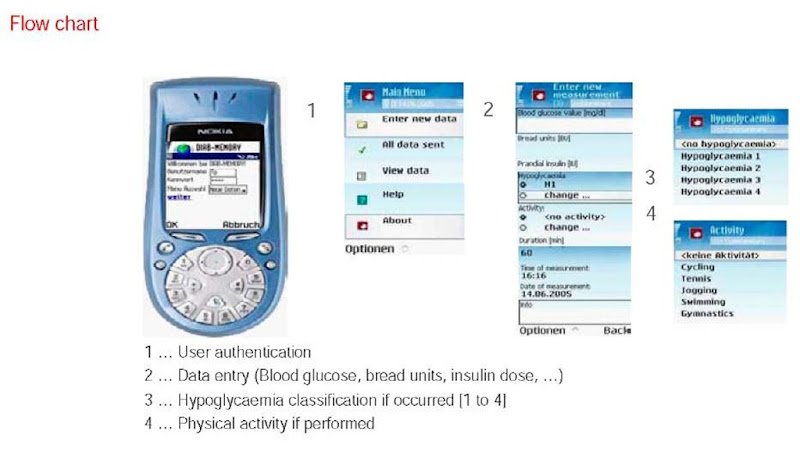
The usage of a J2ME-based software application running on mobile phones has been evaluated in a pilot trial concerning the management of diabetes patients (Riedl, Kastner, Kollmann, Schreier, & Ludvik, 2005). The software has been designed to support the user in entering diabetes-related data like blood-glucose level, insulin dose, bread units, well-being, and activities with remote synchronization to the database at the central monitoring centre. The graphical user interface is shown in Figure 6.
After having logged in, the data is entered via the well-designed graphical user interface and stored directly in a local database on the mobile phone. From time to time, the user can initiate a synchronization process via HTTP request and GPRS data transfer. After the uploading of the data to the remote monitoring centre, the user is able to access several graphical representations, statistics, and trends on his or her data through a secure Web interface.
Figure 6. A Java-based software application running on mobile phones supports the user in home-based data acquisition of diabetes-related key measurements
The software has been evaluated in a clinical pilot trial. Ten diabetes mellitus type 1 patients (36.1 ± 11.4 years) were asked to collect dia-betes-related data (blood glucose, bread units, insulin dose, well-being, activity, etc.) at least 3 times and up to 10 times a day by using J2ME software application running on a NOKIA 7650 mobile phone. In case of less than 3 transmitted data records a day, an automatic reminder SMS message was sent to the patient. The total number of received messages was 10,053 (1,257 +/- 351 per patient). Average blood-glucose level during the initial and final 14 days was 138.5 +/- 63.7 vs. 137.1 +/- 69.2 mg/dl, and HbAlc values were 7.7 +/- 0.4% vs. 7.6 +/- 0.4%, respectively. Although no tele-medical intervention by the physician was yet established, corresponding parameters decreased due to an advanced adherence to therapy. Additionally, ubiquitous availability and the appealing user interface were well perceived by the patients resulting in a high success rate for data transmission and patient acceptance.
Semiautomatic Methods
Running a J2ME-based software application on mobile phones supports also the possibility to access integrated mobile-phone features like Bluetooth. Bluetooth wireless technology is a short-range radio technology that makes it possible to transmit data over short distances between mobile phones, computers, and other devices. Supporting standard measurement devices like blood-pressure meters or glucose meters with a Bluetooth communication module gives them the possibility to transfer data to the mobile phone in an automated way. The software running on the mobile phone handles data exchange and triggers further data transmission to a central monitoring centre (Husemann & Nidd, 2005).
Multimedia Messaging Service
MMS, an extension to the SMS, defines a way to send and receive wireless messages that may include images, audio, and video clips in addition to text. When the technology will be fully developed, the transmission of streaming videos will be supported as well. A common current application of MMS messaging is picture messaging – the use of camera phones to take photos for immediate delivery to a mobile recipient.
MMS has been used in our research as a unique approach to the human-computer interface challenge based on digital-camera-enabled mobile phones. Values shown on the display of the measurement device were taken by a camera-enabled mobile phone. Special Symbian-based (Symbian, 2005) software, running on the mobile phone, helps the user to handle this data-acquisition process. All necessary configurations are made by the program automatically. If an online connection to the data carrier service (GPRS, UMTS) at a given location and time is not available, the mobile phone repeatedly tries to send the data until the message has been sent successfully. Data acquisition and transmission can be achieved with only two keystrokes.
At the monitoring centre, the MMS arrives as a photo attached to an e-mail. The subject of this e-mail contains the IMEI (international mobile station equipment identity) of the mobile phone. Thus, the photo can unambiguously be assigned to a patient. Other important parameters like capturing date and time are also stored within the e-mail.
Special software, running on the Web server, fetches the e-mail available on the mail server, extracts the photo, and moves it to the local file system. Subsequently, the incoming photo is registered to the database and assigned to the corresponding patient.
Thereafter, a special character-extraction algorithm starts to process the photo in order to extract the numerical values. In case of successful character extraction, the values are stored into the database and the report-processing unit isstarted.
Figure 7. “MoniCam “principle: A special software application helps the user to take a photo of the display and send it to a central monitoring centre via MMS, where the values are extracted and stored in the database automatically
Graphs and trends are generated and limit checks are performed. Finally, all information is made accessible via the Web interface to authorized users. In case of unsuccessful character extraction or failed plausibility check, the user may receive a message via SMS to repeat the measurement.
This new method has been evaluated in a feasibility study on five users with four different blood-pressure devices and two different camera-enabled mobile phones (Schreier, Kollmann, Kramer, Messmer, Hochgatterer, & Kastner, 2004). The results indicate that the rate of correct value extraction varied considerably with respect to the type of the measurement device but was comparable for the two different types of mobile phone. For two types of blood pressure meters the method was capable of determining the correct values in well above 90% of the cases. The MMS-based transmissions of the taken photos succeeded in all cases.
Requirements on mobile-phone-based telemonitoring application
Because of the ubiquitous availability of mobile phones, these devices may be considered to be the patient terminal of choice to provide an interface to home monitoring systems. It has to be taken into account, however, that elder patients are often very unskilled and not familiar with the handling of mobile phones. To avoid rejection of this concept as well as to motivate the patients in using such devices, consequentially, an easy-to-learn and easy-to-use system for data acquisition is essential. Based on our experience, the ideal human-computer interface would have the following properties.
High usability
Usability tells us how well the users can use the system productively, efficiently, and pleasantly to reach the goals in a certain environment. Using mobile phones as home monitoring terminals is limited in terms of input interaction (small buttons to enter data as well as to navigate) and output interaction (small display size and poor resolution). To overcome these limitations, an appealing user interface, well-structured graphical design (metaphoric), and intuitive navigation are essential. The number of buttons to be used as the necessary number of button clicks for navigation and entering data should be reduced to a minimum. Moreover, the data-acquisition process should be easy to learn, intuitive, and well structured to decrease barriers against technical devices and improve users’ satisfaction in using the system.
Low cost
The main driving force for introducing new innovations into healthcare is to reduce costs. Hence, patient terminals for home monitoring applications should ideally be based on off-the-shelf technology available without significant set-up expenses or extra costs.
Error Resistant
User actions as well as data entries should be checked for plausibility on the earliest possible stage. For example, a data-entry plausibility check on the side of the patient will exclude errors at origin. A major aspect in handling errors is to provide the user with well-defined error messages that are also easy to interpret and to understand. Well-structured error handling can guide the user through difficulties without confusing him or her.
Off-Line Data Acquisition
It is a well-known fact that wireless networks especially sometimes lack availability (e.g., in buildings). To provide the user with the possibility to enter data at any time and any location, intermediate local data storage is desirable. When the network is available again, stored data can be synchronized with the central database.
High Flexibility and Adaptability
Patient terminals should provide flexibility in terms of adding or removing parameters to the user interface, corresponding to changing conditions in the treatment of chronic diseases. For meeting the needs of an adjusted, personalized patient terminal, the system should support the possibility to interrogate different parameters depending on the time of day or the patient’s history. The user interface for daily use should be configurable to different patients and conditions such as displaying the appropriate drug name to enter the correct dosage. Ideally, user interactions or setup procedures are no longer necessary.
High Security Level
Handling data about the health status of patients, in general, requires a high standard of security.
In most countries, end-to-end encryption is compulsory to meet security directives and laws. As a consequence, most standard communication technologies and protocols already provide some sort of data protection to guarantee that data cannot be accessed, stored, or manipulated while they are transmitted via Internet or wireless networks.
Bidirectional Communication
The ideal patient terminal combines the possibility to provide the user with an interface not only for entering data but also for receiving feedback, reminders, or medical advice on the same device.
Device Independency
Currently, numerous models of mobile phones from various manufacturers are available on the market to be used as patient terminals. Therefore, a software application that provides a graphical user interface highly demands independency of device specifications like operating system, display resolution, mobile Internet browser, menu navigation, and so forth to ensure high usability for a wide range of mobile phones.
Table 1. Overview of the properties and technologies (+ means the method complies with the requirement, +/- means it complies only partly, – means does not comply)
|
|
Technology |
||||
|
Requirement |
SMS |
WAP |
J2ME |
MMS |
Automatic |
|
Overall usability |
- |
+/- |
+ |
+ |
+/- |
|
Low cost |
+/- |
+/- |
+/- |
- |
- |
|
Error resistant |
- |
+/- |
+ |
+ |
+ |
|
Off-line data acquisition |
+ |
- |
+ |
+ |
+/- |
|
High level of flexibility/ adaptability |
- |
+ |
+/- |
- |
- |
|
High security level |
- |
+ |
+ |
+/- |
+ |
|
Bidirectional communication |
+ |
+/- |
+/- |
+ |
+/- |
|
Device independency |
+ |
- |
+/- |
+ |
- |
Table 1 gives an overview of the requirements and the degree of compliance of the various technologies as discussed in this topic and proposes a three-level classification based on our experience and the results of trials of other authors.
SMS
Using SMS technology for data acquisition is not very suitable due to the lack of usability and the fact that a graphical user interface cannot be provided. Basic skills in handling mobile phones as well as knowledge in using the keypad are essential to enter values in a predefined template. SMS for data transmission can be considered when only a single value has to be transmitted (e.g., PEF value in case of monitoring asthma patients; Ostojic et al., 2005). On the other hand, SMS is very suitable for sending messages, automatically generated reminders, or medical advices from the healthcare provider to the patient as an additional way of communication.
WAP
Several studies have been performed utilizing a WAP browser to provide the user with a user interface to enter data. Although a graphical user interface is provided, basic skills in handling a mobile phone and using the numeric keypad are important. Moreover, WAP lacks the possibility of client-side data-entry plausibility checks. The data have to be sent to the server before the values can be processed or checked for plausibility. In case of an error, the user is prompted to the page where the error occurred and asked to reenter the data.
On the other hand, WAP technology provides high flexibility and adaptability because WML scripts are server based and can be generated dynamically depending on user settings and requirements. This fact makes this method seem quite suitable for providing dynamical questionnaires such as quality-of-life assessments or to track medication intake, which is quite different from patient to patient. WAP technology may also be useful were a stepwise data input is required.
A disadvantage of WAP-based systems is that an online connection has to be established during the whole data-entering process. We experienced that this fact can lead to problems. For example, when the data connection is lost, users are confused by the corresponding error message. Thus, incomplete record sets are common and some patients were not able or willing to use the method for daily data acquisition.
Java
Java-based software is less affected by temporary lack of network availability because the data can be stored locally on the mobile phone and the data-transmission process may be postponed until network connectivity is available. Additionally, implementation of checking the plausibility of the entered data is also feasible, resulting in a lower error rate.
Moreover, Java technology allows one to improve usability through the design of user-friendly GUIs by using metaphoric elements. However, updating software applications running on the mobile phones is difficult and requires some additional user experience, although over-the-air application downloading (OAD) simplifies the way applications are delivered to customers.
In addition to standard TCP and HTTP, the Java environment supports the secure hypertext transfer protocol (HTTPS) using standard secure socket layer (SSL) to enable encrypted, secure connections. J2ME is particularly suitable for monitoring applications where frequent data acquisition is necessary (e.g., diabetes) and provides a fast and efficient method to enter, store, and transmit data.
Irrespective of which technology will be used, the most challenging part in developing mobile- phone-based applications for home monitoring is to guarantee interoperability. For example, WAP technology is strongly based on standards but every mobile-phone manufacturer speaks a slightly different WAP language. According to our experience, J2ME applications also change their looks depending on the type of the mobile phone.
MMS
Using a camera-enabled phone for data acquisition by taking a photo of the display provides a really easy and intuitive method for health-data acquisition at home. On the other hand, there is a huge effort on the server side to provide an image-processing algorithm to extract and interpret values correctly. This method lacks also in terms of flexibility and adaptability. Furthermore, costs for the MMS picture transfer are an obstacle for daily usage.
Automatic
Some measurement devices are already equipped with short-range wireless communication technologies like Bluetooth or infrared to transmit data to the mobile phone, which operates as a hub and a gateway to relay those data to a central monitoring centre. Because there is no mass market for such devices yet, they are usually considerably more expensive. Another weak point of this concept, according to our experience, is that it is sometimes not straightforward to establish communication between the mobile phone and the measurement device. Depending on the model, it may be necessary to navigate deep into the menu for setting up the connection. This makes such methods often unusable for technically unskilled people. However, once the system is set up correctly, data acquisition is fairly automated and error resistant. Using the mobile phone as a hub provides a bidirectional communication between patients and healthcare providers; hence, the mobile phone can receive SMS. Therefore, in the long run, automated systems will be the method of choice for elderly and unskilled or handicapped patients to transmit their self-measurements to the monitoring centre.
Developing mobile applications for Telemonitoring Applications
Because of small display sizes, limited resolution, and restricted possibilities for user interaction, navigation design and the implementation of software applications for mobile devices is quite different from software developments on other platforms like stationary desktop PCs.
Mobile software applications can be divided into two groups:
1. Highly goal driven.
2. Entertainment focused.
Highly goal-driven services aim at providing fast replies to specific problems, whereas entertainment-focused services enable the user to pass the time, for example, by offering gossip, games, or sports results (Ramsay & Nielsen, 2001). Mobile applications for home monitoring are definitely goal-driven, that is, to provide the users with a method to enter data in the most suitable way. Therefore, a user-centered design process is necessary. This process involves a number of important phases.
Analysis
The initial phase of software development is the most critical one. In this stage, the requirements of the patient terminal should be clearly defined by determining the user-group characteristics and the monitoring scenario. Typical attributes of the user group are age, expertise, experience level, and physical limitations. The definition of the monitoring scenario comprises the parameter to be monitored, the way feedback is given, and the demand in terms of flexibility.
Thereafter, the use case of the specific monitoring scenario should be clearly described in order to define objectives and features that require close cooperation between technician and physician. Once the general use case has been defined, the technology has to be selected that best supports the requirements of the respective application. Table 1 can serve as a guide to get an overview of properties of available technologies. Features as well as limitations of the selected technology should be carefully balanced during the design process.
Design
According to our experience, the typical software application for home monitoring applications comprises the following four stages:
1. Identification: The user is asked to log onto the system with a unique user name and password combination to facilitate authentication and access control.
2. Data acquisition: Menus and input templates guide the user through the data-acquisition process.
3. Transmission: Entered data are either stored locally or are transmitted to a central database in a monitoring centre.
4. Feedback: To indicate that data storage or transmission has been executed successfully or the presence of special situations, feedback should be given to the user immediately after data transfer in a representative form.
The development of a consistent, easy-to-use application does not require coding at this stage. On the contrary, ideally, a conceptual framework is established, representing the application and its workflow on a metaphoric level (e.g., a storyboard).
Evaluation
The concept designed in Step 2 should be evaluated by both types of users: patients and physicians. Usability considerations should be made; for example, unnecessary button clicks or confusing workflows should be avoided. There is also the need to identify sources of errors. If significant changes are necessary, an iteration starting with the design step is required.
Implementation
There are several software-development kits (SDKs) available to develop software for mobile devices. However, irrespective of which SDK or programming language is adopted, developing software applications for mobile phones requires substantial experience in programming efficient and reliable software.
Testing
The developed software can be tested and debugged on emulators that are provided by the mobile-phone manufacturers. However, according to our experience, emulators are often error prone and sometimes special features are not supported. Hence, it is essential to test developed software on target devices themselves.
FUTURE TRENDS
Current trends in chronic-disease management enforce shifting tasks from the clinic to patients’ homes. This means that self-management and collaboration between patients and caregivers will become more and more important and may benefit from upcoming technologies.
Technical Advancements for Mobile-Phone-Based Patient Terminals
Phones enabled with radio-frequency identification (RFID) and near-field communication (NFC) may soon be used as patient terminals to provide an intuitive and easy-to-use way for health-data acquisition at home.
RFID tags are able to uniquely identify an object, animal, or person, or to store data. They have been introduced in the industry as an alternative to the bar code. Passive RFID tags are powered by the magnetic field generated by the reader. The tag’s antenna picks up the magnetic energy, and the tag communicates with the reader in order to retrieve or transmit data.
In a current research project, we developed a scenario where RFID tags are used in a home monitoring environment. Objects to be tracked or identified are equipped with RFID tags. For example, tagging medication boxes with RFID tags provides an easy and intuitive method for the patient to indicate which medication has been taken simply by touching the box with an RFID-reader-enabled phone. Special software running on the mobile phone fetches the information from the tag, adds a time stamp, and initializes a transmission to the monitoring centre automatically. Hence, no cumbersome user interaction and configuration is needed.
Electronic Data Capture in Clinical Trials
The combination of mobile and Web-based technologies will improve clinical-trial efficiencies through increased data accuracy, higher data yield per patient, and real-time access to trial data (Stokes & Paty, 2002) by using mobile phones for timely and patient-centered data acquisition. Patient diaries as well as consequent monitoring of health parameters of interest can add meaningful information about the safety and efficacy of a treatment and can save time and money. Additionally, quality-of-life data will also play a central role in future clinical trials, which can be accessed easily by mobile-phone-based software solutions.
LESSONs LEARNED
Self-management and cooperation between patients and healthcare providers are the basic aspects and strategies of efficient chronic-disease management. An important element in efficient self-management is the monitoring of health-related data reliably. Because of the ubiquitous availability of mobile phones, these devices can be used as patient terminals so as to provide the patient with a method to enter data easily as well as to receive feedback or medical advice from remote healthcare professionals.
The most critical part in this respect is the user interface. Software specifically developed to the needs of the respective patient group is required to guide them through the data-acquisition process. Mobile data services and transmission protocols like SMS, MMS, WAP, and HTTP can be used to exchange data and information between patients and their caregivers. These methods have already been evaluated in several clinical trials and feasibility studies, and medical benefit could be demonstrated as well. However, using mobile phones as patient terminals is limited due to small display, poor resolution, and small buttons for user interaction.
Up to now, there is no method that fulfils all criteria of an ideal patient terminal in terms of high usability, adaptability, flexibility, and low cost. Every method for entering data implies specific advantages and disadvantages. Hence, when designing a mobile-phone-based home monitoring system, the patient terminal that best fits into a particular monitoring application has to be chosen on an individual basis, depending on the requirements, the user group, and the medical demand.