Buffering Systems
Any acid, whether metabolic or respiratory, entering the bloodstream immediately encounters the three chemical buffers that circulate throughout the body in the bloodstream. Bicarbonate (HCO3), the most common chemical buffer, almost instantaneously couples and neutralizes the acid (H+), releasing heat in the process. The result is carbonic acid (H2O3). Carbonic acid then reverts into water (H2O) and carbon dioxide (CO2) in the lungs. The water (H2O) is then either absorbed or excreted by the kidneys and the carbon dioxide (CO2) is exhaled in the breath.
While bicarbonate is a powerful buffer, the amount of bicarbonate in the bloodstream is limited and only provides approximately one half of the blood buffering capacity.
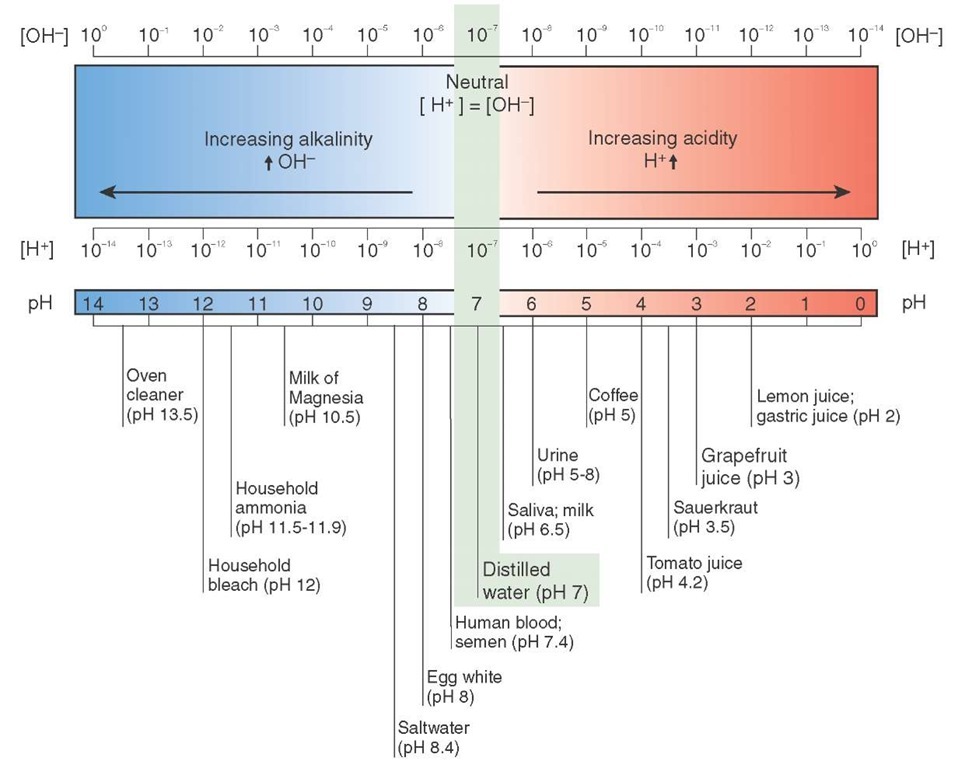
Figure 25-5 pH scale with common acids and bases shown.
Another chemical buffer, phosphate (PO4), also helps to buffer acids. Phosphate buffers bind with acid and carry the acid to the kidneys to be excreted, thus making urine acidic.
Finally, the proteins in the blood have a limited ability to buffer acid. All blood proteins, including albumin the most abundant blood protein, are made of chains of amino acids. These amino acids became neutralized when bonded in chains, but these proteins are capable of accepting more acids. Therefore, albumin is important to helping maintain an acid-base balance. Albumin is so important that patients who have liver disease, and subsequently reduced albumin, are more likely to have problems with maintaining acid-base balance.
Blood proteins also include the hemoglobin molecules contained within the red blood cells (erythrocytes). Hemoglobin can preferentially bind to either oxygen (O2) or acid (H+), and therefore it releases its oxygen at the capillary level and picks up acid at the venous side for removal in the lungs or kidneys. Patients who have lost large volumes of blood will have difficulty with maintaining an acid-base balance because they have lost hemoglobin.
In addition to the chemical buffering that occurs to handle the day-to-day production of acids in response to metabolism, there are two other ways the body can compensate for increased acid production. Both respiratory compensation and renal compensation kick in during times when the body is producing additional acids, whether through increased metabolic load, disease, or lack of oxygen. The three means of buffering—chemical, respiratory, and renal—are interlinked and any weakness in one is compensated for by the others.
Respiratory Compensation
The lungs also have an ability to help rid the body of acid by driving the acid-bicarbonate formula. The acid-bicarbonate reaction is easily reversible, releasing acid back into the bloodstream in the form of carbonic acid (H2CO3) (Figure 25-6). Sensitive central chemoreceptors monitor cerebrospinal fluid (CSF) for an increase in carbonic acid, the respiratory acid, and stimulate the medulla to increase respirations. Increased respirations increase removal of carbon dioxide and drive the formula to the left, forcing the conversion of acids into bicarbonate, then carbon dioxide and water, which are removed through ventilation and urination. This process of increasing the respiratory rate in response to increased acidity of the cerebral spinal fluid occurs rapidly, within several minutes.
Figure 25-6 The acid-bicarbonate reaction. Increased ventilation forces this chemical equation to move to the left, increasing production of carbon dioxide and water, which are then removed from the body.
Renal Compensation
In the triad of buffering systems, the kidneys are the last line of defense. When carbonic acid reaches the kidneys, an enzyme called carbonic anhydrase (an- – "without", hydra -"water", -ase – "enzyme") breaks the carbonic acid down into bicarbonate (HCO3) and acid (H+). The acid is excreted in the urine. In the process, the bicarbonate (HCO3) is regenerated for use in the bloodstream. The kidneys also can create ammonia from the breakdown of the amino acid glutamine by the enzyme glutaminase, an enzyme that works best in an acidic environment. Ammonia (NH3) then couples with acid (H+) to become ammonium (NH4) and is excreted in the urine. Ammonium is a volatile acid, meaning that it off-gasses into the atmosphere and gives urine its distinctive odor.
This process of enzyme activation, reabsorption of bicarbonate, and excretion of acids can take up to 49 hours to fully activate. For this reason, compensation by the kidneys is ineffective during an acute emergency. Renal compensation only comes into action in patients who are chronically ill or who have been acutely ill for several days.
Effects of an Acidic Environment
The efficiency of all of the body’s chemical processes, whether in the bloodstream, within the cells, or in the space between the cells, depends on the local pH where the process takes place. If the local environment becomes too acidic or too basic, the chemical process may not occur at all. Transport of materials across cell membranes may also not occur if the pH of the blood is too far outside the normal range. This can affect important body functions (e.g., produce cardiac dysrhythmias, affect oxygen transport, and affect muscle strength). Two important areas pertaining to Paramedic practice are oxygen transport and the effect of medications.
Acidosis and Oxygen Transport
As discussed earlier in this topic, oxygen is picked up by the hemoglobin in the red blood cells and transported to the tissues where it is released and used to produce energy. Hemoglobin’s attraction, or affinity, for oxygen is due to the iron molecules that make up the hemoglobin. However, acids have a greater affinity for oxygen. When acid is present, it will cause oxygen to separate (dissociate) from the hemoglobin. This phenomenon, called the Bohr effect, is responsible for oxygen entering the tissues at the cellular level in the interstitial space, where the environment is slightly more acidic than in the central circulation. The process of cellular respirartion starts with meta-bolically active cells. These cells produce acid as one of the by-products of metabolism. These cells also need more oxygen to sustain their aerobic (with oxygen) metabolism. The acid causes the capillary beds to dilate, permitting more oxygen-carrying hemoglobin red blood cells in the blood to enter the capillary. Once the blood is in the capillary bed, and in the presence of the acid, the oxygen is released from the hemoglobin and moved into the cells. The use of oxygen in the cell is a process called cellular respiration.
A problem occurs when the blood in the central circulation becomes acidotic from a large "acid load" developing within the body. Under normal conditions the acid in the blood, as carbonic acid, changes to carbon dioxide, diffuses in the alveoli, and is exhaled. With the acid eliminated from the blood, the oxygen in the alveoli can be attached to hemoglobin and carried out to the capillary beds. If the acid load in the central circulation is too great (e.g., secondary to hypoventilation or an increase in metabolic acids), then the oxygen will not be released into the tissues and the patient may experience hypoxemia. Due to the effect of acid and temperature on the oxyhemoglobin curve described in Figure 25-4, the oxygen saturation of a patient who has a fever or who has a large acid load, as is the case with a septic patientfrom a severe infection, will be lower than expected. The oxygen saturation may remain lower than expected despite the presence of high-flow oxygen via nonrebreather face mask until the underlying metabolic cause—in this case, the infection—is treated.
Acidosis and Medication
Acidosis, excessive acid in the system, can have a profound effect upon the body’s uptake, distribution, and the effectiveness of medications administered by the Paramedic as well. Once a medication is in the bloodstream and enters the interstitial space it must cross the cell wall, a lipid-protein matrix. This semipermeable membrane readily accepts those medications that are not ionized (i.e., did not dissolve in solution). These "lipid-soluble" medications easily diffuse across the lipid-protein cell membrane (i.e., "like dissolves like"). The problem occurs when a medication enters the bloodstream and is dissolved, meaning the medication becomes divided into two charged or "ionized" portions. Some medications start as a salt and then dissolve in solution to become ionized as either a weak acid or weak base. These ionized (charged) medications are repelled by the cell membrane and are called lipophobic (lipo- – "fat", phobic -"fear") medications. Lipophobic medications require carriers or other compounds (e.g., bicarbonate or an amino acid) to carry the medication into the cell. When the surrounding tissues are acidotic, the medication is not dissolved normally and absorption is reduced, thus reducing the drug’s efficiency.
Acid-Base Disorders
Changes in the acid-base balance in the body can have dramatic effects on the patient’s signs, symptoms, physiology, and the effects of medications on the patient. Even in the brief patient contact time as part of many EMS calls, the Paramedic can detect subtle signs of these derangements and initiate treatment that can prevent or slow catastrophic deterioration in the patient’s condition. These disorders are typically identified through either an arterial blood gas or a venous blood gas, where a blood sample from either an artery or a vein is analyzed for the pH, the partial pressures of carbon dioxide and oxygen (pCO2 and PO2), the bicarbonate, and the oxygen saturation. These parameters are examined to assess for an acid-base disorder. While the interpretation of arterial and venous blood gas is outside the scope of the typical street Paramedic, there are several causes for each and associated signs and symptoms.
The blood can either become acidotic if the pH falls below 7.35 or alkalemic if the pH rises above 7.45. Each of these main disorders has respiratory causes and metabolic causes for the acidosis and alkalosis. Therefore, the four main acid-base disorders, in order of most common to least common for Paramedics, are respiratory acidosis, metabolic aci-dosis, metabolic alkalosis, and respiratory alkalosis.
Acidosis
The blood becomes acidotic if the pH falls below 7.35. As previously discussed, the blood in the capillaries is slightly more acidotic than the blood in the central circulation, which assists in the off-loading of oxygen and removal of carbon dioxide from the tissues. Acidosis can occur as a result of either problems with the respiratory acids or the metabolic acids. It is possible to have a mixed respiratory and metabolic cause for a patient’s acidosis when a chronically ill patient has an acute exacerbation of her disease or when more than one active disease process is present.
Respiratory Acidosis
The problem of respiratory acidosis can be further subdivided into two categories: either too much carbonic acid production or too little ventilation. The classic case of too much carbonic acid production is the patient with a fever, pyrexia, whose body is hypermetabolic. The acute nature of fever causes the body’s metabolism to increase, producing additional carbon dioxide and other by-products.
The more traditional cause of respiratory acidosis is hypoventilation. Conditions such as strokes, brain trauma, and drug intoxication—especially with opiates—can depress the respiratory drive at the respiratory center in the medulla. Spinal cord trauma and diseases that affect the nerves or the muscles can cause either the respiratory muscles or the nerves controlling the respiratory muscles to provide inadequate ventilation, which in turn causes hypoventilation. Illness and injury to the lungs themselves can result in hypoventilation. Any condition, either traumatic or medical, that impairs gas exchange reduces the lungs’ ability to exchange oxygen and carbon dioxide, producing a respiratory acidosis.
Treatments for the patient experiencing respiratory aci-dosis focus on ensuring the patient has adequate oxygenation and ventilation. This may include administration of supplemental oxygen or invasive airway management maneuvers as discussed in previous topics.
Metabolic Acidosis
During metabolism, the body makes acids other than carbon dioxide. These metabolic acids can cause systemic acidosis as well. The quintessential example of metabolic acidosis is the patient experiencing diabetic ketoacidosis. During hypoglycemic conditions, the body breaks down fats for energy and produces ketonic acids in the process, leading to ketoaci-dosis, or ketonic acids in the blood. Other causes of metabolic acidosis include cyanide poisoning and carbon monoxide poisoning. Both of these conditions deprive the cells of oxygen and force anaerobic (without oxygen) respiration.
While too much lactic acid, pyruvic acid, or ketonic acid can produce metabolic acidosis, the absence of bicarbonate can also result in a relative metabolic acidosis. Under normal conditions, the kidneys and the bowels reabsorb bicarbonate, making it available for reuse. Therefore, any gastrointestinal or urinary disease can cause serious problems with maintaining acid-base balance. For example, the gallbladder secretes bicarbonate to neutralize the acid created by the stomach. This bicarbonate is then reabsorbed in the intestines. When massive or persistent diarrhea occurs, then the intestines cannot reabsorb the bicarbonate. When a patient experiences renal failure, the kidneys cannot absorb the bicarbonate that is excreted into the urine. The patient may become acidotic from the lack of the bicarbonate buffer.
Metabolic acidosis can also be caused by ingestion of substances that are toxic or in toxic doses. Certain alcohols cannot be metabolized by the body and produce metabolic acids as a result of this incomplete metabolism.
Aspirin is another medication that can lead to acidosis. Aspirin is a medication that many people take to decrease the risk of a heart attack, whereas some people take it as an analgesic. Aspirin is the active ingredient in many over the counter (OTC) medications. In high doses, aspirin, (chemical name: acetylsalicylic acid and abbreviated as ASA) can cause metabolic acidosis. In severe cases of aspirin overdose aspirin inhibits the respiratory center in the medulla, leading to hypoventilation and compounding the metabolic acidosis with a respiratory acidosis.
Treatment of acidosis from a metabolic cause typically involves first ensuring adequate circulation. This may include administering intravenous fluids, administering medications to increase the patient’s blood pressure, administering antibiotics to treat infection, or performing chest compressions during cardiac arrest. These supportive measures help the body resolve the acidosis naturally. Sodium bicarbonate is sometimes administered intravenously in an attempt to correct a severe metabolic acidosis by providing additional bicarbonate to buffer the acid.
As acidotic patients tend to hyperventilate as a way of compensating for the metabolic acidosis, if the Paramedic needs to secure the airway, the Paramedic must remember to either ventilate the patient at a higher rate or set the respiratory rate on the ventilator to a higher-than-normal rate in order to maintain an adequate ventilatory rate for that compensation. If too low of a respiratory rate is provided, and the underlying metabolic process is not corrected, the patient will continue to become more acidotic until the patient goes into a cardiac arrest. Cardiac arrest in these cases often does not respond to treatment because of the severe acidosis.
Alkalosis
The blood becomes alkalotic if the pH rises above 7.45. As with acidosis, this can be due to either a respiratory or metabolic cause. Alkalosis from a metabolic cause occurs more often than from respiratory etiologies.
Metabolic Alkalosis
Metabolic alkalosis is caused by an increase in the production of bicarbonate in the blood. This can be due to a metabolic process in the body and can also be due to increased kidney reabsorption of bicarbonate from the urine. Common causes of metabolic alkalosis include severe volume depletion and acid loss, as occurs in dehydration from vomiting, and electrolyte disturbances (e.g., low potassium), which triggers reabsorption of bicarbonate by the kidneys. Certain endocrine disorders can also produce a metabolic alkalosis by decreasing the serum potassium level. The use of some diuretics, specifically those that spill potassium into the urine (e.g., potassium wasting diuretics), can cause a metabolic alkalosis because they cause an increase in reabsorption of bicarbonate.
Treatment of metabolic alkalosis depends upon the cause. In the case of volume depletion (e.g., from vomiting, diarrhea, or overdiuresis), administering normal saline will help correct the volume loss. It is important to monitor the patient’s oxygenation, as the body’s primary means of compensating for a metabolic alkalosis is to hypoventilate, producing a mild respiratory acidosis to compensate for the metabolic alkalosis. In patients with normal respiratory function, the effect of the hypoventilation is minimal. However, in patients who have a significant respiratory condition (e.g., chronic obstructive pulmonary disease (COPD)), hypoventi-lation may not be tolerated well and the patient may become hypoxic. Supplemental oxygen may be required to treat the hypoxia. In patients who are paralyzed and on a ventilator, the respiratory rate can be decreased to help treat the metabolic alkalosis.
Respiratory Alkalosis
Respiratory alkalosis occurs when ventilation is greater than the body’s CO2 production. As previously discussed, the CO2 generated by the body is primarily removed by the respiratory system. Changes in the respiratory rate occur very rapidly in response to an increase or decrease in the circulating CO2 level. When the metabolic rate increases quickly (e.g., when a person jumps up from a resting position and runs a quarter mile sprint), the respiratory rate increases rapidly in response to the increased metabolic CO2 production. At the end of the race, when the metabolic production of CO2 decreases, the respiratory rate will decrease to the baseline rate over the course of several minutes. In some conditions, however, there is a mismatch between the respiratory rate and CO2 production, with the patient breathing at a faster rate than required to handle the production of CO2. This increased minute ventilation lowers the CO2 level, producing the alkalosis. When a patient has a condition that causes metabolic acidosis, this mechanism compensates for the acidosis and helps move the pH back toward the normal range. However, when the patient does not have an existing metabolic acidosis, this increased ventilation stimulus produces the respiratory alkalosis.
There are several causes for the increased stimulation. Normally, if hypoxemia occurs in the central circulation, receptors in the aorta and carotid arteries will signal the respiratory center to increase the respiratory rate in order to compensate for the decreased oxygenation. However, in some situations, the central circulation is not hypoxemic. However, the tissues are hypoxic, and cause an increase in respiratory rate. Any condition that decreases the off-loading of oxygen at the tissue level (e.g., shock or anemia) can cause an increase in the respiratory rate.
A second abnormal stimulus for increased ventilation can occur with abnormal stimulation of the stretch receptors located in the alveoli and smaller air passages in the lungs. Normally, the stretch receptors help signal the start and stop of ventilation. However, in the case of irritation of the alveoli from pneumonia, pleural effusion (abnormal liquid in-between the pleural layers), or congestion in the pulmonary capillaries, the stretch receptors can trigger increased ventilation, producing a respiratory alkalosis.
The respiratory center can be directly stimulated by a variety of conditions and produce increased ventilation. Certain toxins, either ingested or produced by other conditions (e.g., liver failure or renal failure) can trigger increased ventilation. Fever or the toxins in sepsis can also increase ventilation and produce a respiratory alkalosis. Certain hormones can also stimulate increased ventilation. This occurs as a normal part of pregnancy to increase respiratory rate late in pregnancy to compensate for difficulty in fully expanding the lungs due to the growing fetus. Changes in blood chemistry that occur when at altitude also produce a mild hyperventila-tion to compensate for the lower partial pressure of oxygen at high altitude.
Finally, psychologically induced hyperventilation can occur as a response to fear, anxiety, pain, or any number of emotional stressors. This increased respiratory rate can be either involuntary or voluntary and often responds to calming and reassurance. With severe hyperventilation, the decrease in blood CO2 causes vasoconstriction of cerebral blood vessels, reducing blood flow. In some cases, this can cause light-headedness or even syncope.
STREET SMART
It is very easy to blame hyperventilation on a psychological cause. Be aware that many other conditions can produce hyperventilation, including hypoxia, shock, and sepsis. Search for these causes during your patient assessment and treat them appropriately. Do not allow the patient to breathe into a paper bag or an oxygen mask that is disconnected from supplemental oxygen! This rebreathing will produce an abnormal increase in CO2. For the patient that is hyperventilating in response to a pathologic cause, this increase in CO2 may produce unconsciousness, profound metabolic derangements, and cardiac arrest.
Treatment of respiratory alkalosis depends on the cause. If the patient is hypoxic or there is a reason for tissue hypoxia (e.g., shock), then providing supplemental oxygen or treatment of shock may improve the alkalosis. If psychogenic causes are present, attempt to calm the patient, provide reassurance, and appropriately treat pain and anxiety. Consider other respiratory or central causes when developing a paramedical diagnosis, ensure the patient’s ABCs, and provide supportive care.
Mixed Disorders
The four acid-base disturbances should not be thought of as isolated entities. In reality, the body is complex and will respond both acutely and chronically to compensate for these dysfunctions. Some disease processes, or combination of disease processes, may cause a mixed acid-base disorder, where a primary disorder (e.g., respiratory acidosis) is partially compensated by the body by another disorder (e.g., a metabolic alkalosis). In some cases, the acidosis and alkalo-sis can have both a respiratory and metabolic cause (e.g., a respiratory and metabolic acidosis that can occur with some conditions). These disorders can be challenging to sort out. When in doubt, fall back to the ABCs and ensure the patient has a patent airway, is well ventilated and oxygenated, and is not in shock. This can be easily summarized as supporting the ABCs. This initial attempt at resuscitation and stabilization can go a long way in improving the patient’s condition.
Assessment of Oxygenation and Ventilation
The Paramedic has several tools at her disposal to help assess oxygenation and ventilation in the critical patient.In this section, we will discuss some of the objective measures of oxygenation and ventilation, including pulse oximetry, capnography, co-oximetry, and arterial blood gas sampling.
Pulse Oximetry
Pulse oximetry is a non-invasive measure of the percentage of hemoglobin sites in the red blood cells that are bound to oxygen, or oxyhemoglobin. This percentage of oxyhemoglobin is called oxygen saturation and is abbreviated as SpO2. A normal SpO2 is between 95% and 100%. An SpO2 reading between 90% and 95% indicates mild hypoxemia, and a reading between 85% and 90% indicates moderate hypoxemia. A reading below 85% indicates severe hypoxemia requiring intervention by the Paramedic. There are two ways to report oxygen saturation: One is displaying a quantitative measure of the oxygen saturation and the other is displaying the oxygen saturation as a waveform over time. For oximeters that only display a numerical value, there is an indication of signal strength that provides the Paramedic with an indication of the strength of the blood flow across the sensor. For oximeters that provide a waveform display in addition to the numerical value, the shape of the waveform provides the Paramedic with a visual indication of the strength of the blood flow across the sensor (Figure 25-7).
Technology
Measurement of the SpO2 involves beaming a light wave across the patient’s capillary bed and detecting the wavelength on the opposite side of the capillary bed. The light wave is combined red and infrared frequencies.
Figure 25-7 Pulse oximeters may display a numerical indication of SpO2 or waveform display of SpO2.
As the wave passes through the capillary bed, the light is absorbed by the hemoglobin differently depending on if it is in the oxyhemo-globin form or the deoxyhemoglobin form. The oxyhemo-globin form absorbs more infrared light than red (therefore explaining the bright red color of oxygenated blood) and deoxyhemoglobin absorbs more red light than infrared. The wavelengths at the light source are known and compared to the wavelengths detected at the sensor. The ratio between the wavelengths transmitted and received is compared with a database of known values and is used to calculate the SpO2. These known values are only available in the range of 70% to 100% saturation as this information was derived from actual patients.
The most common source used to measure SpO2 is the tip of a finger. Light travels easily through the fingertip and the capillary bed is relatively superficial to the skin surface. Alternatively, the earlobe can also be used for a similar reason. Two other sites include tip of the toes, useful in children, and the skin on the forehead, useful in hypothermic patients.
The strength of the signal detected by the pulse oximeter is reported as the perfusion index on oximeters that do not display a waveform. The perfusion index is measured from 0.02% to 20%, with the larger number indicating a stronger signal. The higher the perfusion index, the more accurate the reading. Therefore, when using device pulse oximeter, the Paramedic can use the perfusion index indicator to know if the pulse SpO2 reading displayed is an accurate reading. In some cases, the Paramedic will need to try several different sites before obtaining an accurate SpO2 reading. The pulse rate is calculated from the time between peaks of the fluctuating pulse oximetry wave.
For devices that display a waveform, the shape of the waveform can be used to determine the accuracy of the SpO2 reading (Figure 25-8). The waveform amplitude fluctuates normally, corresponding to the flow of blood through the capillary bed. If the Paramedic encounters a poor quality waveform (Figure 25-9), the Paramedic will need to place the sensor on a different site.