KEY CONCEPTS:
Upon completion of this topic, it is expected that the reader will understand these following concepts:
• Fluid balance
• Indications for intravenous access
• Method for venipuncture
• Complications of intravenous access
• Techniques and strategies for pediatric phlebotomy and intravenous access
• Alternative access points and central venous access devices
CASE STUDY:
As the second unit rolled up onto the scene of a two-car MVC, the Paramedics heard from the first unit that they should set up a trauma line for the driver of car #2. She was being extricated now and had significant injuries. Oh, and by the way, the driver was Mrs. Gorino.
Everyone knew Mrs. Gorino. She was a pleasant woman who had battled back from breast cancer but needed frequent hospitalizations for a myriad of medical problems. Only the best of the best Paramedics could find IV access on her.
OVERVIEW
Intravenous access allows the Paramedic to administer medications and manage a patient’s intravascular volume. To effectively care for the patient, the Paramedic must have a commanding knowledge of the equipment used for intravenous access, as well as complete assessment skills and techniques. By examining the sources of fluid loss and clinical signs of fluid displacement, the Paramedic can determine the need for intravenous access and develop an appropriate treatment plan. Needs and skills vary according to age and clinical condition.
Intravenous Access and Paramedics
The public distinguishes the Paramedic from basic life support providers by the Paramedic’s ability to start intravenous access (IV). The public knows that an IV permits the Paramedic to give pain medicine and other life-saving drugs. Perhaps no other ALS skill is practiced as often as intravenous access. Therefore, the Paramedic should be an expert at establishing intravenous access.
Physiology Review
The human body is primarily made up of water, about 30 liters of water, which is distributed across three compartments. When thinking of body fluids, the first compartment generally considered is the intravascular space in which the blood volume is contained within the arterial, capillary, and venous vessels. However, the bulk of the water is contained within the second compartment, the intracellular compartment (ICF), while the remaining volume is contained in the third compartment, the extracellular fluid (ECF). The extracellular fluid (ECF) bathes the cells as interstitial fluid.
The constant ebb and flow of these fluids across these three compartments, exchanging gasses, hormones, glucose, fatty acids, and wastes, is the basis for nutritional flow. Using this nutritional flow to an advantage, Paramedics can inject a concentrated quantity of medication, called a bolus, into the intravascular space and reasonably expect that the medication will make it into the cells of the target organ.
Medical vs Trauma
The rationale for obtaining intravenous access can be grossly broken down into two categories: medical and trauma. Both patient populations undoubtedly need venous access in cases of emergency, and the risk/benefit of obtaining an intravenous line leans so decidedly toward providing benefit that Paramedics attempt venous access almost all emergent patients and most urgent patients. What remains undecided is the use of intravenous infusions in specific cases.
Medical lines, sometimes called lifelines, are a means of giving medications directly into the circulation. A number of methods have been devised to gain venous access, yet one constant remains for all of them—intravenous access is necessary for medication administration.
The second indication for intravenous access is trauma. Blood losses can make the patient who has experienced trauma hypovolemic. A trauma line is inserted into the vascular space so that intravascular volume can be replaced and homeostasis restored. In some cases, a patient with traumatic injury may need medications. Conversely, a medical patient may experience a significant loss of fluid and require volume replacement, though there has been no trauma. It is apparent that the divisions are not clean and each type of line is sometimes used for the other purpose.
Sources of Fluid Loss
Fluid loss, due to either illness or injury, is an indication for intravenous access. By understanding the sources of fluid loss, the Paramedic can anticipate the need for intravenous access. Fluid loss is a normal function of the body. Such loss may be apparent, such as urination, or may be unsuspected (insensible). Insensible loss is that volume of fluid that is lost from the body in the form of perspiration off the skin (1.1 liters/daily) and the vapor in the breath. Normally, the patient would replace this loss through fluid intake as well as the water contained in the foodstuffs ingested.
The amount of fluids normally lost, both sensible and insensible losses, can be accelerated by disease. Paramedics who are confronted with a patient who has a medical complaint and has signs of hypoperfusion should perform a complete history and physical assessment of the patient to ascertain the source of the fluid loss as well as ascertain the degree of hypovolemia.
A common cause of increased insensible fluid loss is increased perspiration secondary to fevers due to infection.1,2 This loss, combined with the anorexia (lack of appetite) that often accompanies a fever, can result in an imbalance of fluid intake versus output. Add the vomiting and diarrhea which often accompanies many illnesses, and the patient may quickly develop a significant fluid imbalance.
During a 24-hour period, the average person will excrete—and then reabsorb—approximately one-half of her intravascular volume into the lumen of the intestines. This process of excretion and reabsorption of nutrient ladened fluids constitutes nutritional flow and is essential to the body’s sustenance. Any process which interferes with that flow can create fluid imbalances.
Beyond the fluid loss that accompanies vomiting and diarrhea, other gastrointestinal problems can create hypo-volemia secondary to the fluid loss. For example, a patient with a small bowel obstruction will not be able to reabsorb the fluids in the large bowel as the patient normally would. Subsequently, the fluids excreted into the small bowel are sequestered behind the obstruction, leading to a distended abdomen. The volume of fluids is not returned to the central circulation as would normally occur.
Draining abdominal fistula, ileostomy, colostomy, and aggressive nasogastric tube suctioning, as well as overuse or misuse of renal diuretics, are other examples of important sources of fluid loss.
However, it is trauma, with its problematic hemorrhage, that can cause the quickest fluid loss. Rupture of solid organs, such as the spleen and liver, following either blunt or penetrating trauma can quickly create profound hypovolemia. The Paramedic is well-advised to consider occult trauma whenever confronted with hypoperfusion of unknown origin.
Past Medical History
A number of pre-existing medical conditions can also contribute to increased fluid loss. The following short list of medical conditions can lead to increased and/or excessive fluid loss leading to hypovolemia; this list not all inclusive of medical conditions that can lead to fluid loss.
Diabetes insipidus, secondary to brain tumor or any other space-occupying lesion, can cause life-threatening dehydration within hours. Diabetes insipidus causes the kidneys to pass the filtrate from the plasma almost unchanged. Normally 99% of this filtrate is reabsorbed.
Emphysema, with its accompanying persistent tachy-pnea, can lead to significant insensible fluid loss through rapid respiration. Coupled with the diuretic action of many respiratory drugs such as aminophylline, and without adequate fluid replacement, the patient can become markedly dehydrated.
Initially, the thought of congestive heart failure summons thoughts of fluid overload, and during an acute exacerbation this may be the case. However, the combination of forward failure and subsequent inadequate renal perfusion, coupled with overuse of prescribed diuretics and a constant shifting of fluid volumes across all three fluid compartments, can culminate in a complicated clinical picture which can include cellular dehydration, vascular volume depletion, and electrolyte imbalances. Heart faiulure, therefore, is a problem of fluid maldistribution coupled with interstitial dehydration.
Despite an apparent constant intake of fluids, the alcoholic patient is prone to fluid deficits as well. While alcohol itself is a diuretic, the impact of liver cirrhosis is probably greater upon the patient’s fluid volume state. When the liver is not producing sufficient blood proteins, such as albumin, secondary to cirrhosis, the colloidal osmotic pressure (COP) within the blood falls, and with it the patient’s intravascular volume.
Hyperglycemia can be another cause of acute fluid loss. Hyperglycemia, the hallmark of new onset diabetes mellitus, acts as an osmotic diuretic and draws fluid from the interstitial space into the central circulation. As this volume increases, the kidneys increase urine output to excrete the excess volume. The patient, whose tissues are now dehydrated, craves water. Despite drinking steadily (polydipsia), the patient cannot take in enough fluids to offset the excessive output from urination (polyuria).
Physical Examination for Dehydration
The patient who has lost significant intravascular volume, secondary to dehydration, may manifest signs of hypoper-fusion which will be evident during the initial assessment. These signs include decreased level of responsiveness, tac-hypnea, tachycardia, hypotension, or postural hypotension. When these signs culminate to present a clinical picture of hypoperfusion, the Paramedic may decide to institute fluid replacement immediately.
A number of other signs may precede this presentation and suggest dehydration and impending hypoperfusion. These signs, in a head-to-toe fashion, are lackluster eyes, eyes that are sunken into their sockets and appear dull. The absence of tears in a child’s eyes should alert the Paramedic to the presence of dehydration.
Dry and cracked lips along with pale mucous membranes in the oropharynx are signs of dehydration. The tongue may be the best external measure of the patient’s hydration. Normally, a tongue is plump, and moistened with saliva. However, when a patient is dehydrated the tongue becomes dry and furrowed (furrows being long fissures in the tongue).
Next, the Paramedic should examine the neck, particularly the jugular veins. Some Paramedics regard the jugular veins as the "dipstick" of the heart. Under normal conditions when a patient is lying flat, the external jugular veins are at least minimally distended and clearly visible, indicating a sufficient blood volume. In the case of the patient who is dehydrated, the jugular veins will lie flat against the neck when the patient lies flat.
The next indicator of hydration is the urine output. While not practical in the field, unless the patient has an indwelling urinary catheter, measuring a patient’s hourly urinary output is an excellent indicator of vascular volume. When urine output drops below 20 mL per hour (oliguria), then the patient is experiencing significant hypoperfusion of the kidneys, an early indicator of shock.
In the hospital setting, the gold standard for fluid balance is the patient’s weight. Even with constant monitoring and recording of intake and output, many critical care units weigh their patients regularly, in some cases daily, in order to monitor fluid balance. Long-term care facilities also regularly weigh their patients.
The Paramedic who looks for these early signs of dehydration and fluid deficits will not be surprised when the patient becomes hypotensive. Perhaps more importantly, the Paramedic may be able to intervene early and prevent hypotension.
Intravenous Fluids
Intravenous fluids used for medical patients are intended to be either intravenous routes for therapeutic medications, or to be therapeutic in and of themselves. Intravenous fluids used for trauma patients are more often intended to replace lost volume and therefore are therapeutic.
In the case of trauma, the optimal fluid replacement for lost blood would be blood. However, current blood storage requirements and inadequate prehospital equipment make blood replacement in the field impractical. In an effort to overcome these obstacles, physicians and scientists are trying to create a variety of blood substitute.To date, trials of these blood substitutes are falling short of expectations, but more blood substitutes are being researched.
These blood substitutes contain proteins, and are thus called a colloid. These colloidial fluids are capable of both pulling fluids from within the interstitial space into the circulation, to help augment the circulating volume, and remaining within the blood stream for a prolonged period of time, helping to maintain the circulating volume.
In the interim, and until these solutions are available, Paramedics must use electrolyte-containing fluids during trauma resuscitation. These electrolyte solutions, when dehydrated, create crystals. Thus, these electrolyte-containing fluids are referred to as crystalloids.3-6
The electrolytes commonly found in crystalloid solutions—sodium, chloride, and potassium—are the same electrolytes found within the blood. In fact, several crystalloid solutions were created in an effort to reproduce a "bloodlike" mixture. British physicist Sidney Ringer was made famous when he tried to create a "balanced solution" in 1873, the solution which still bears his name, but was unable to bottle the solution because of its effervescence. Improving on Dr. Ringer’s solution, and solving the problem of effervescence, Dr. Hartmann added lactate, resulting in lactated Ringer’s solution (LR). Lactated Ringer’s solution remains the solution of choice of trauma surgeons (advanced trauma life support, or ATLS) and in the treatment of burn patients (American Burn Foundation or ABF).7-10
When caring for a medical patient, a number of additives may be added to the solution to provide a therapeutic benefit. The most common additive is dextrose, a simple sugar which can be quickly metabolized to meet the ill patient’s higher energy demands. Other additives include antibiotics, vaso-pressors, antidysrhythmics, and a host of other medications. Many of these therapeutic solutions are run intermittently, as a secondary intravenous solution, through a primary infusion line containing either 0.9% sodium chloride in sterile water (0.9% NaCl) or 5% dextrose in sterile water (D5W).
STREET SMART
A solution of 0.9% sodium chloride in sterile water (0.9% NaCl) contains the same amount of salt as does the blood. For this reason, many healthcare providers refer to 0.9% NaCl as normal saline solution (NSS). NSS has become an EMS standard solution in many systems because it is compatible with all medications as well as blood.
Tonicity
A solution is considered balanced if it has the same concentration of solutes to solvent as there are solutes to solvent present in the blood. Any imbalance of this solute concentration would cause an osmotic effect to be created when administered intravenously, potentially overhydrating or dehydrating a cell. In other words, tonicity could be thought of as the solution’s ability to alter a cell’s internal fluid balance through osmotic force created by the imbalance between the tonicity of the solution outside of the cell versus the tonicity of the fluid within the cell. When the percentage solute in the solution is similar to the percentage solute in the blood, such as is the case with a balanced solution, the solution is said to be isotonic. Examples of nearly isotonic fluids include D5W, LR, and NSS. When additional substances or additives are added, thus increasing the concentration of the solutes compared to blood, then the solution is said to be hypertonic. Hypertonic solutions will, by osmotic force, draw water out of the cell, causing the cell to dehydrate and collapse or cre-nate. Conversely, if pure sterile water, or a solution which has fewer solutes than blood, was injected, then the solution would be referred to as a hypotonic solution. Cells would then, by osmotic force, draw water into themselves, expanding in the process to the point where the cell would burst. Various changes occur when isotonic, hypotonic, and hyper-tonic solutions are mixed with red blood cells as shown in the following figure (Figure 27-1).
Intravenous Fluid Administration
Once a solution has been selected, the Paramedic turns his attention to the administration of that fluid. Intravenous solutions come in either plastic containers or, more rarely, glass bottles and in volumes ranging from 25 mL to 3,000 mL. Paramedics typically use 250 mL, 500 mL, and 1 L solutions. Glass containers are noncollapsible and must be open to air, or vented, to prevent the creation of a vacuum. While plastic containers are increasingly more common, glass containers are still used for medications which react with or are absorbed into the plastic. IV bags are soft plastic solution containers which collapse as the solution is withdrawn, eliminating the need for venting, and create a closed system which helps to decrease the risk of outside contamination.
Figure 27-1 (a) Isotonic solution. (b) Hypertonic solution. (c) Hypotonic solution.
A careless infusion of intravenous fluids can lead to serious systemic complications. For example, contaminated intravenous fluid can lead to septic shock. An intravenous infusion bypasses many of the body’s defenses against infection. Without these protections, the patient’s blood could become infected, a condition called septicemia, and the patient could develop a potentially life-threatening sepsis. When a Paramedic starts an intravenous access, it is understood that the Paramedic has the responsibility to take all reasonable precautions to prevent such an occurrence.
There are a number of occasions when the intravenous fluid can become contaminated. The intravenous solution could have become contaminated before the Paramedic handled the solution. The container could have been accidentally punctured, or contaminants accidentally introduced along with the additives during the manufacturing process. Understanding this risk, every manufacturer takes precautions to prevent contamination. However, despite these precautions, contamination can still occur. Most manufacturers will only guarantee a solution’s sterility for a certain period time, a date stamped on the package.
Understanding these precautions have already been taken, every Paramedic performs a three-step inspection of the solution before it is opened. After confirming that the correct solution has been chosen, the Paramedic verifies that the solution is not expired. The expiration date, stamped or printed on the container, is evidence that the solution is less likely to be contaminated.
Next, the Paramedic examines the solution for clarity. Intravenous solutions are generally clear, with some notable exceptions being medications like diazepam (pale yellow). With the solution held up to a light, the Paramedic should inspect the solution for any discoloration or any particulate matter. If contamination is suspected, then the solution should be discarded immediately.
Finally, the Paramedic should test the container to see if it is intact and without microscopic holes that could be portals for contamination. A firm twist of the bag should reveal any leaks. If the bag does leak, it should be discarded and another solution chosen.
STREET SMART
Some intravenous solutions come with a second protective outer wrap around the bag. Due to differences in humidity from the site of manufacture and the present location, condensation may have occurred. The Paramedic should first wipe the bag down and then test the container’s integrity. Follow this rule, however: "If in doubt, throw it out."
Administration Sets
The next step in preparing to administer an intravenous solution is connecting an administration set to the solution. During this procedure, the greatest risk of contamination may occur. Careful attention to detail is important to prevent sterile components from contacting nonsterile surfaces. The purpose of an intravenous administration set is to provide a sterile pathway for the intravenous fluid from the container into the patient.
The selection of an administration set is largely dependent upon the patient’s condition. When volume replacement is needed (e.g., during a trauma resuscitation), then a short,straight line with the fewest obstructions, such as filters or medication portals, is desirable. These administration sets are referred to as macro-drop administration sets (Figure 27-2).
Figure 27-2 Macro-drop intravenous administration set.
When careful titration of medicated fluid is desired (e.g., when a medical patient needs a slow infusion of a drug), then fine control of the infusion stream is needed. These administration sets are referred to as micro-drop administration sets.
Anatomy of an Administration Set
Every administration set has a spike, sometimes called a bayonet, which is used to pierce the fluid container. As the name implies, the spike is very sharp and is as capable of cutting flesh as easily as it is capable of piercing a plastic seal in a bag of intravenous solution. Caution should be observed when mating the spike of the administration set to the solution bag to prevent inadvertent puncture of the side of the solution bag, which can result in a puncture of the Paramedic’s finger as well.
Below the spike is the drip chamber. Hanging drops are formed inside the drip chamber. These drops can be counted, as drops (gtt) per minute (gtt/min), and the rate of flow established. If the chamber has a thin, or needle, dropper, then the administration set is called a micro-drop set. By convention, all manufacturers have set 60 drops from a micro-drop set to equal 1 mL. The needle dropper is visible within the drip chamber (Figure 27-3).
If the drip chamber does not have a needle dropper, then the set is called a macro-drop set. Unlike the micro-drop set, macro-drops can vary in size. The variation in the size of the drop directly relates to the number of drops per 1 mL. To determine the drip rate for a particular macro-drop administration set, the Paramedic should refer to the labeling on the packaging. In some cases, the drip rate is embossed directly into the plastic on the spike as well.
Further down the length of the tubing is a drip rate control device. The drip rate control device allows the Paramedic to regulate the flow (i.e., the rate of drop formation) so that precise volumes can be administered (drops per minute being equated to mL per hour). Most control devices have either a roller clamp (Figure 27-4) or screw-type device, both of which function by compressing the tubing. The roller clamp, a common control device, has a thumb wheel which compresses the tubing against a hard plastic back and thus limits flow.
Figure 27-3 Micro-drop drip chamber.
Figure 27-4 Control devices: Roller clamp type.
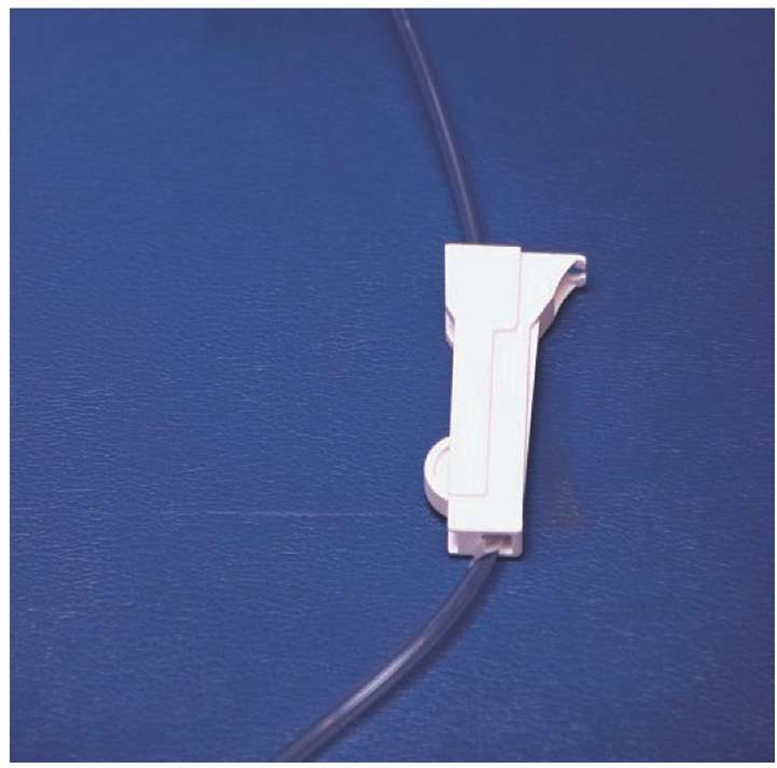
Another control device, the slide clamp (Figure 27-5), is used to cut off flow entirely. This is necessary during intravenous drug boluses to prevent retrograde infusion of the medication into the intravenous tubing rather than into the patient. By sliding the tubing into the groove, flow is stopped. Similar to a slide clamp, some administration sets have a squeeze-clamp which can cut off solution flow.
Some administration sets come with a mid-line, in-line check valve designed to prevent the administration set from running dry. If an administration set does run dry, there is a risk that the venous catheter will become clogged by a blood-clot, rendering it useless. To prevent the catheter from clogging, the check valve leaves a standing column of solution in the line.
Figure 27-5 Intravenous administration slide clamp.
Figure 27-6 In-line medication port.
Hard plastic in-line medication ports (Figure 27-6) provide access for injection of drugs into the solution stream. These ports can be either capped with a self-sealing membrane, into which a needle would be inserted, or a needleless check-valve system designed to accept a syringe’s luer lock tip.
Some intravenous administration sets have a device called a flash bulb. The flash bulb is a soft in-line pyramid-shaped device. When the tubing is clamped and the flash bulb is squeezed, a show of blood can be seen in the distal tubing. This blood "flash" is an indicator that the venous access is still patent. Some flash bulbs are made of self-sealing materials which permit insert of a needle for injection of medications, thus making the flash bulb the most proximal medication port to the venous access.
Some intravenous administration sets also have an in-line filter. The in-line filter is designed to strain the solution for large particles of undissolved medication, solution crystals,contaminants, and the like. Disk-like in appearance, these inline filters are usually found proximal to the drip chamber but distal to any medication ports.
Figure 27-7 Anatomy of an intravenous administration set.
The place where the administration set inserts into the hub of the venous catheter is called the adaptor. The adaptor is sterile where it couples with the catheter hub and a cap is in place over the adaptor to prevent contamination. In some cases, the impervious hard plastic adaptor must be removed in order to allow the solution to be run through the administration set prior to insertion. In those cases, the cap must be retained to re-cover the sterile adaptor once the solution has been run out in order to maintain the sterility of the adaptor. Other adaptors have a semi-porous cap which permits fluid to run out through the cap without compromising sterility (Figure 27-7).
STREET SMART
When the adaptor’s cap is misplaced, the administration set can be capped with a spare covered sterile needle. The diameter of the hub and a needle are the same. When the administration set is to be attached to the hub of the venous catheter, the needle is then discarded into a sharps container.