Electrode Placement
Accurate electrode placement is important. In some cases, the prehospital 12-lead ECG may not display ischemic changes. However, when serial ECGs obtained later are compared against the initial 12-lead ECG, the differences become apparent. These comparisons are only valid if the electrodes have been placed in the same position.
The American Heart Association emphasized proper lead placement in 1938 when it first standardized the placement of precordial leads. It continues to establish the standard for electrode placement in order to obtain a clinically relevant 12-lead ECG.18
Standard Limb Leads
Limb leads are traditionally placed where Einthoven placed them—on the end of the extremities. One electrode should be placed on the ventral surface of the right and the left wrist and another placed on the ankle proximal to the medial malleolus.
The electrode should be placed on the properly prepared skin overlying muscle, not bone. The resulting leads—Lead I, Lead II, and Lead III—are therefore a function of the polarity ascribed to them by the ECG monitor. Often these electrode wires are labeled for ease of application.
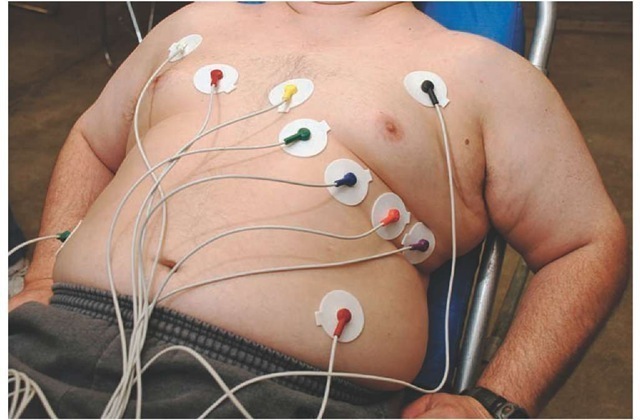
While technically correct, the placement of electrodes on the ankles and wrists of the patient is often mechanically inconvenient. Problems with resting tremors and clothing prevent the Paramedic from obtaining an accurate 12-lead ECG. This distortion can be minimized if the electrodes are moved more centrally. In 1966, Mason and Likar suggested moving the electrodes to the shoulders and the hip. To properly place the limb electrodes in the Mason-Likar modification, the right arm electrode is moved to the right infraclavicular fossa, approximately 2 cm below the clavicle. The left arm electrode is similarly placed in the left infraclavicular fossa, and the left leg electrode is moved next to the left iliac crest in the iliac fossa. This placement of the limb leads maintains the integrity of Einthoven’s Triangle without the inconvenience of distal limb lead electrodes.
Because the ECG machine electrically converts the bipolar limb leads into unipolar augmented leads using the same leads and electrodes, it is unnecessary to add additional electrodes for the augmented leads.
To ensure consistency in application of the 12-lead ECG data, the Paramedic should document if the 12-lead ECG was obtained using the Mason-Likar modification. The documentation may simply state that all electrodes were placed on the torso.
Precordial Leads
Wilson’s precordial leads measure the ECG potentials across the anterior wall of the left ventricle. Precordial leads are to be placed according to specific landmarks. Variation in the placement of precordial electrodes can sometimes produce diagnostically significant changes in the 12-lead ECG.
The first electrodes, V1 and V2, are placed within the 4th intercostal space at the right and left sternal border, respectively. Mistakenly, Paramedics may palpate the space just below the clavicle, assume it is the 1st intercostal space, and start counting down three more spaces. This placement is incorrect and will cause V1 and V2 to be placed too high.
The Paramedic should first identify the suprasternal notch above the sternum and palpate inferiorly until a ridge is felt. The ridge on the bone is the connection of the manubrium to the body of the sternum (the angle of Louis). Moving laterally to the right, the Paramedic should palpate the second intercostal space along the sternal border and then palpate the spaces downward until the 4th intercostal space is palpated.
Figure 34-5 Precordial electrode placement.
The first precordial electrode, V1, is placed on the right sternal border and V2 is placed across from V1 at the same level on the left sternal border.
From the V2 position, the Paramedic should palpate the 5th intercostal space and move laterally to the midclavicular line to place the V4, the third electrode. The fourth electrode placed is V3, which is placed midpoint along an imaginary line that runs between V2 and V4.
Continuing to palpate along the 5th intercostal space, the Paramedic should place V5 at the left anterior axillary line, in line with the iliac crest, and V6 at the 5th intercostal space along the left midaxillary line (Figure 34-5 and Table 34-1).
If the patient has large breasts, male or female, place V4 under the breast and V3 over the breast. The V4 electrode should be placed flat against the chest and not partially on the breast and the chest. This position would cause the electrode to fold over on itself and will not sense the electrical activity. If the patient is small or thin, then place the electrodes between the ribs, avoiding the bony prominences, if possible.
Table 34-1 Lead Names with Correct Electrode Placement
|
LA |
Left arm over muscle or flesh |
|
RA |
Right arm over muscle or flesh |
|
LL |
Left leg over muscle or flesh |
|
RL |
Right leg over muscle or flesh |
|
V1 |
4th ICS RSB, 4th right intercostal space at the sternal border |
|
V2 |
4th ICS LSB, 4th left intercostal space at the sternal border |
|
V3 |
Between V2 and V4 |
|
V4 |
5th ICS MCL, 5th left intercostal space at the midclavicular line |
|
V5 |
5th ICS LAAL, 5th left intercostal space at the anterior axillary line |
|
V6 |
5th ICS LMAL, 5th left intercostal space at the midaxillary line |
The Paramedic should document if it is necessary to perform the 12-lead ECG on a patient in a semirecumbent position, such as in a wheelchair or recliner. The patient’s change in position from Fowler’s position, at a 45-degree angle, causes the heart to swing anterior and closer to the chest wall.
Dextrocardia
Some patients have a congenital condition in which the body’s organs are mirror opposite of normal. Situs inversus, which is a complete reversal of all thoracoabdominal organs, occurs in less than 1 in 10,000 patients but has been a documented medical phenomenon since 1643. If the heart and lungs are opposite and the abdominal organs are in their usual position, this is referred to as dextrocardia.19
When the Paramedic initially places the patient on the monitor to determine a rhythm, it will be noted that Lead I is inverted. An inversion in Lead I is suggestive of dextrocar-dia. A standard 12-lead ECG will support the diagnosis. The patient with dextrocardia will have a P wave axis greater than 90 degrees and a poor R wave progression, both discussed shortly.20
If dextrocardia is suspected, or the patient confirms dextrocardia, then the Paramedic should proceed by placing the electrodes on the right side of the thorax. The Paramedic should make a note on the 12-lead ECG printout that dextro-cardia is suspected and right-sided chest leads were placed.
12-Lead ECG Tracing
Before reading a 12-lead ECG the Paramedic must understand the standard layout of the printout. Like a rhythm, a 12-lead ECG is never read off the monitor screen but instead is printed out for careful analysis.
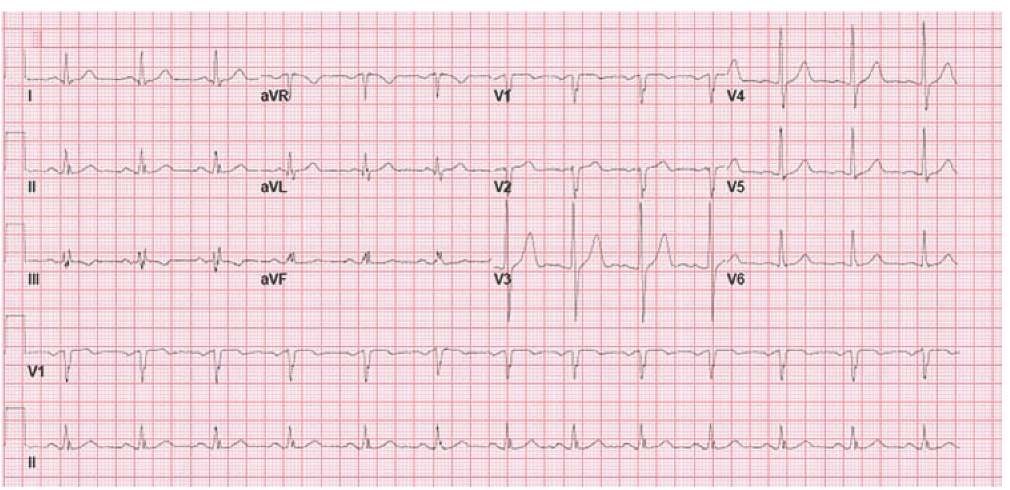
Figure 34-6 Normal 12-lead ECG.
A 12-lead ECG is printed in a standard four-column format. The 12-lead ECG machine reads three leads simultaneously for 2.5 to 3 seconds until all 12 leads are obtained and then prints out the 12-lead ECG.
Beginning on the far left column, the printout contains the standard limb leads I, II, and III. The 12-lead ECG machine then uses the limb leads and, with the creation of Wilson’s central terminal, creates the augmented leads, aVR, aVL, and aVF.
Moving from the limb leads to the precordial leads, the 12-lead ECG machine reads and records the precordial leads, starting with V1, V2, and V3, then reads and records V4, V5, and V6 (Figure 34-6).
In some instances, the 12-lead ECG machine will simultaneously record both the 12-lead ECG and the monitor lead and a single monitoring strip may be printed across the bottom. Although most machines will default to Lead II for the monitoring strip, the Paramedic may choose to record a different lead depending upon the patient’s condition.
STREET SMART
Some older 12-lead ECG machines can only print a single lead at a time. These machines, called single-channel machines, print the 12-lead ECG in the same sequence but in one very long ECG strip.
Electrocardiographic Assessment of Left Ventricular Function
The left ventricle is essential for cardiac output to the body (in general) and to the brain (in particular). All other portions of the heart (the atriums and the right ventricle) could be considered auxiliary to the left ventricle. In fact, loss of any one of these auxiliary portions of the heart is survivable, whereas loss of the left ventricle is usually fatal. For this reason, the 12-lead ECG focuses on the left ventricle.
For ease of conceptualization, the left ventricle is said to have four walls. It is actually a cone-like shape with artificially contrived sides. The lower portion of the left ventricle, next to the epigastrium, is called the inferior wall. The portion of the left ventricle that is shared with the right ventricle (the septum) is called the septal wall. That foremost portion of the left ventricle, where the bulk of the myocardium exists, is called the anterior wall. The last wall, the lateral wall, is actually an extension of the left ventricle’s anterior wall.
Contiguous Leads
An ECG lead gives the Paramedic a view of a particular portion of the left ventricle. The 12-lead ECG allows the Paramedic to have several views of the heart in an effort to try and capture evidence of myocardial injury. When two or more leads look at the same wall of the left ventricle, they are said to be contiguous leads.
ECG leads are related to each other by the position of the positive electrode which, in turn, affords a specific view of a particular portion of the ventricle. In the standard 12-lead ECG, the limb leads II, III, and the augmented lead, aVF, the positive electrode is located on the lower extremity and looks up toward the bottom of the heart. The bottom of the heart is a portion of the left ventricle called the inferior wall. Thus, these leads (II and aVG) are called inferior leads and can be said to be contiguous.
Leads I, aVL, V5, and V6 have the positive electrode located on or beneath the left arm. These leads look at the heart’s lateral wall and are called lateral leads. Similarly, leads V1 through V4 have the positive electrode on the front of the chest. These leads look at the front portion or anterior wall of the left ventricle. The front of the chest is a large area. Thus, these leads are broken into subcategories. V1 and V2 have the positive electrode over the interventricular septum and are also referred to as septal leads. V3 and V4 continue to be known as true anterior leads.
In some cases, the evidence of myocardial damage spreads across two walls of the left ventricle. In those cases, both walls are used in the description. For example, injury to both the anterior wall and the septal wall, as evidenced by ECG changes in the contiguous leads V1, V2, V3, and V4, would be referred to as anteroseptal. Similarly, myocardial damage to both the inferior and the lateral wall, as evidenced by ECG changes in Leads I, II, III, aVL, aVF, V5, and V6 would be called inferolateral. If there are changes suggestive of damage to the entire myocardium (i.e., ECG changes in all leads), then the term "global" is used. ECG changes in only two contiguous leads are necessary to make a presumption of myocardial injury (Table 34-2).
Table 34-2 Contiguous Leads
|
• Pure changes |
|
|
II, III, aVF |
= Inferior |
|
V1, V2 |
= Septal |
|
V3, V4, V5 |
= Anterior |
|
I, aVL, V5, V6 |
= Lateral |
|
• Mixed changes |
|
|
V1, V2, V3, V4 |
= Anteroseptal |
|
I, II, III, aVL, aVF, V5, V6 |
= Inferolateral |
|
I, aVL, V3, V4, V5, V6 |
= Anterolateral |
|
II, III, aVF, V1, V2 |
= Inferoseptal |
|
• Global changes |
|
|
V1, V2, V3, V4, V5, V6 |
= Global anterior |
|
I, II, III, aVL, aVF, aVR, |
|
|
V1, V2, V3, V4, V5, V6 |
= Global |
STREET SMART
When a Paramedic sees global changes across all of the 12-leads, consideration should first be given to extra-cardiac causes (i.e., those conditions, such as hypoxia, that could lead to damage to the entire heart).21-23 The likelihood that all of the coronary arteries could have a catastrophic event simultaneously is extremely unlikely.
Relationship to Coronary Arteries
The main coronary arteries perfuse specific areas of the heart and, in particular, the left ventricle. By evaluating the 12-lead ECG for evidence of myocardial injury in the contiguous leads, the Paramedic can infer that ECG changes in those contiguous leads raises a suspicion of involvement of specific coronary arteries.
The coronary arteries originate at the sinus of Valsalva and proximal to the aortic valve, with which they have a symbiotic relationship. There are two coronary arteries which are simply called the right coronary artery and the left coronary artery. The right coronary artery (RCA) runs the length of the heart and has a minor branch, called the marginal branch, towards its terminus. Conversely, the left coronary artery (LCA) divides almost immediately at its mainstem into the left anterior descending coronary artery (LAD) and the circumflex (Cx).
The right coronary artery (RCA) provides blood to the inferior wall of the left ventricle and to the AV node in the majority of patients. Thus, ECG changes in the inferior leads of II, III, and/or aVF would suggest that the RCA may be involved.
The left main coronary artery serves the entire anterior wall including the septum. Occlusions of the left main stem, referred to as "widow makers" (thus emphasizing the importance of the LCA), can cause global anterior wall damage. ECG changes in the anterior leads of V1 to V4 and the lateral leads of I, aVL, V5, and V6 suggest that the LCA is affected.
The LCA almost immediately bifurcates, giving rise to the left anterior descending (LAD) coronary artery and the circumflex coronary artery (Cx). The LAD artery serves the central portion of the anterior wall of the left ventricle. Therefore, anterior wall ECG changes would be expected (V3 and V4).
Lesser branches off the LAD, called the septal perforators (SP), provide the septum with blood, including the bundle branches. Atherosclerotic involvement of the SP will injure the septum and may cause ECG changes in leads V1 and V2 and possible bundle branch blocks.
The LAD then continues to run along the anterior inter-ventricular (AIV) groove which separates the right and left ventricles toward the apex of the heart. Along its path another minor branch of the LAD, which cuts diagonally away from the AIV and toward the anterolateral wall and the apex of the heart, is the diagonal (Dx). Distal occlusions of the Dx can give rise to ECG changes in leads I, aVL, V5, and V6 as well as V4 and V5.
The circumflex coronary artery (Cx) was the second artery at the bifurcation of the left coronary artery. The Cx follows the atrioventricular groove to the lateral wall of the left ventricle. In most cases (approximately 85% of patients), the Cx stops at the left lateral wall. In 15% of patients, the Cx continues and provides perfusion to the AV node. Normally blood for the AV node comes from the right coronary artery. In those cases, the patient is said to be "left dominant," indicating an alternative blood supply to the AV node as opposed to the normal blood supply. The difficulty for the patient who is left dominant arises when an occlusion of the left coronary artery occurs and almost the total of the left ventricle’s myocardium is hypoperfused (Figure 34-7 and Table 34-3).
Interpretation
The primary value of a Paramedic-obtained 12-lead ECG in the field is the identification of myocardial injury and the patient’s transportation to the definitive care center. However, the value in a 12-lead ECG is not only in the identification of myocardial injury but also in the Paramedic’s ability to make a prognosis based on that information. By having information about the location of the myocardial injury, the Paramedic can prepare for complications associated with that injury.
Figure 34-7 Coronary artery anatomy.
Table 34-3 Relationship of Leads to Walls to Coronary Arteries
|
• |
II, III, aVF |
= |
Inferior |
Right coronary artery (RCA) |
|
• |
V1, V2 |
= |
Anteroseptal |
Left anterior descending (LAD)/(SP) |
|
• |
V3, V4 |
= |
Anterior |
Left anterior descending (LAD) |
|
• |
V3, V4, V5, V6 |
= |
Anterolateral |
Diagonal (Dx) |
|
• |
I , aVL, V5, V6 |
= |
Lateral |
Circumflex (Cx) |
|
• |
V1, V2, V3, |
|||
|
V4, V5, V6 |
= |
Global anterior |
Left mainstem (LCA) |
12-Lead ECG Identification of Myocardial Injury
The era of the ECG identification of acute myocardial infarction may have started with Harold Pardee when he published the first ECG of an acute myocardial infarction, describing the T wave as "tall" and "starts from a point well up in the descent of the R wave." From that point, physicians have had a keen interest in using the 12-lead ECG to identify the patient with acute coronary syndrome who is at risk for an acute myocardial infarction.