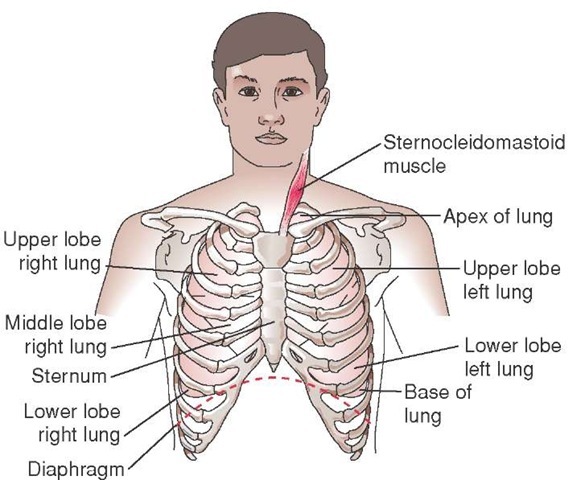
Bony Thorax Anatomy
The bony anatomy of the thorax not only provides protection to the thoracic organs and major blood vessels, but also produces the air pressure difference responsible for air movement in and out of the respiratory system. The bones of the thorax consist of the thoracic vertebrae, the rib cage, the sternum, the clavicles, and the scapulae (Figure 20-9). The clavicles and scapulae are not directly responsible for ventilation but serve as accessory anchoring points for either accessory muscles or for muscles that support the rib cage. The thoracic vertebrae are articulation points for the 12 ribs and form the posterior bony border of the thoracic cavity. The thoracic vertebrae typically do not move during respiration. The exception to this occurs during highly active breathing when an individual leans forward during expiration and then extends the spine and stands straight during inspiration. The ribs, however, do move and articulate with the transverse processes of the thoracic vertebrae. The sternum is a dagger-shaped bone that attaches to the clavicles and the ribs. It is the anterior-most bony structure of the thorax and provides structural support to the ribs during respiration.
The rib cage is the primary bony structure of respiration. Composed of 12 matched pairs of curved bones, the rib cage acts to protect the thoracic structures and serves as the fulcrum for the intercostal muscles of respiration. The ribs are numbered 1 through 12 and articulate posteriorly with their similarly numbered thoracic vertebrae. Anteriorly, the ribs are attached to the sternum by the costal cartilages. Ribs 1 to 7 are considered "true" ribs in that each has its own costal cartilage that attaches it to the sternum. Ribs 8 to 12 are considered "false" ribs. Ribs 8, 9, and 10 are attached to the sternum through a common costal cartilage; the cartilages from each of the rib tips merge into a single cartilage that is attached to the sternum. Ribs 11 and 12 are called "floating ribs" because, although they are attached to other ribs via the intercostal musculature and serve in respiration, they only articulate posteriorly on the thoracic vertebrae and are not directly attached to the sternum via a costal cartilage.6
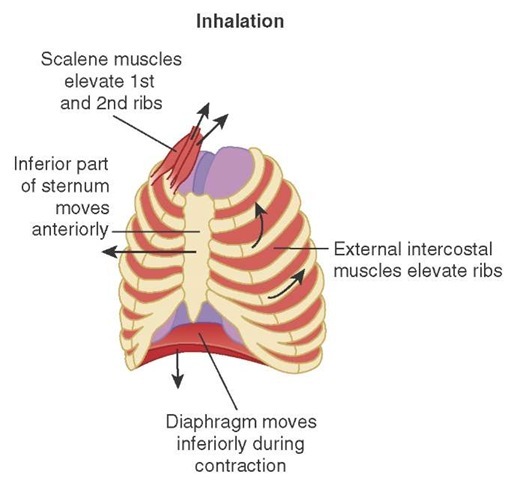
The muscles of respiration can be divided into the principal and accessory muscles of inspiration and the active muscles of expiration. During quiet breathing, without pathologic derangement, the principal muscles of inspiration drive inspiration while passive recoil of the chest wall and lungs drives expiration. During active breathing (e.g., with heavy activity or disease), the accessory muscles of inspiration are recruited, as are the active muscles of expiration. Knowledge of the normal muscles of quiet breathing is critical to understanding respiratory physiology (Figure 20-10).
Figure 20-9 The bony thorax.
One muscle and a major muscle group contribute to inspiration. The first and largest muscle involved in inspiration is the diaphragm. This large, thin, dome-shaped muscle divides the abdomen from the thorax. At rest, the diaphragm rises to the level of the 5th rib (approximately the level of the nipple). During inspiration, the diaphragm contracts and flattens. Since the margins of the diaphragm are fixed to the thoracoabdominal wall, contraction pulls the contents of the thorax inferiorly and pushes the abdominal contents inferiorly. Contraction of the diaphragm also assists the intercostal muscles to elevate the lower ribs.
The second major muscle group involved in inspiration is the intercostal group. The intercostal muscles are muscles that attach the ribs to each other. There are external and internal intercostals; the internal intercostals are further divided into interchondral (between ligaments) and intercostal (between bones) divisions. At rest, the ribs—attached anteriorly to the sternum and posteriorly to the thoracic vertebrae—tend to sag inferiorly and medially (Figure 20-11a). When the external intercostal muscles and the interchondral part of the internal intercostal muscles contract, they elevate the ribs in a motion similar to that of a bucket handle (Figure 20-11b). Functionally, when this happens in the rib cage, the volume of the rib cage increases.
The chest wall interacts with the lung parenchyma via the pleura (Figure 20-12). The easiest way to visualize the pleura is to think about standing a bottle up on a flat garbage bag.
Figure 20-10 Muscles of respiration.
Since the bottle is on the outside of the bag, there are two layers of the bag underneath the bottom of the bottle. If the bag is then lifted up around the bottle, there will be two layers of garbage bag all around the bottle. Finally, the bag is collected at the neck of the bottle and attached with a rubber band. The end result is a bottle inside of a two-layered bag. The layer of the bag against the plastic bottle represents the visceral pleura and the outside layer of plastic represents the parietal pleura. The sealed area at the neck of bottle represents the way the pleura seals against the bronchi as they leave the lungs. In the body, the visceral and parietal pleura lie against each other with a small amount of fluid between them. This allows them to slide against each other but not to pull apart from each other.
Under normal physiological conditions, the two pleural layers are held together by the pleural fluid and expand and contract as a unit. The space between the pleura is a "potential" space because, under normal conditions, it does not exist. However, excessive fluid can build up between these spaces during various disease states (e.g., heart failure) and air can potentially enter the space (e.g., during chest trauma). When the pleural layers separate, they no longer function as a unit. This disrupts the pleural layers’ ability to generate an adequate negative pressure during inspiration, thus reducing lung volumes and creating a sensation of difficulty breathing.
Figure 20-11 a-b Rib movement. (a) Full exhalation position. (b) Full inhalation.
Figure 20-12 Pleural layers against the organs (visceral pleura) and chest wall (parietal pleura).
Respiratory Physiology
Understanding the anatomy of the airway and respiratory system only tells half of the story. Knowledge of the physiology, or the function, of the respiratory system allows the Paramedic to understand the effects disease has on the patient, the effects treatments have on the patient, and ways to troubleshoot the process when the patient does not respond as expected.
Lung Volumes and Capacities
Physiologically, the lung can be divided into several components. The measurements of lung volumes and capacities (Figure 20-13) are important to facilitate descriptions of the physiologic occurrences during respiration. The total lung volume is divided into a number of volume subsets. The first, and most important, volume is the tidal volume. This is the volume of a normal breath and is approximately 5 to 7 cc/kg of ideal body weight.7 During exercise or certain pathological situations, a greater volume—the inspiratory reserve volume—is used. This is the maximum volume that can be inspired above the tidal volume. The maximum volume that can be expired beyond the tidal volume is the expiratory reserve volume. Any air left in the lungs after the expiratory reserve volume is exhaled is the residual volume and cannot be exhaled; it reflects the smallest possible airspace volume based on the anatomy of the lungs.
Alveolar volume is the volume of air in the alveoli. In the average adult male, this volume is 350 cc and reflects the volume of air available for gas exchange. The final volume is the anatomic dead space, which is the volume of the conducting airways. Gas exchange does not occur in the conducting airways, hence the term "dead space." The anatomic dead space is typically 150 mL in the average adult male. There is also a physiologic dead space, which is the volume of the lungs not eliminating carbon dioxide; in certain disease states (e.g., pneumonia, congestive heart failure (CHF), pulmonary embolus, chronic obstructive pulmonary disease (COPD), atelectasis, etc.) this volume may be greater than the anatomic dead space.8
Capacities are another way of describing the lungs’ respiratory volumes. Total lung capacity is the sum ofthe residual volume, the expiratory reserve volume, the tidal volume, and the inspiratory reserve volume. It is a measure of all of the airspace volume in the lungs with the potential to exchange carbon dioxide. The total lung capacity can be broken down into smaller capacities. The vital capacity is a measure of the maximum volume that can move through the lungs in a single respiratory cycle and equals the inspiratory and expiratory reserve volumes plus the tidal volume. The inspiratory capacity equals the tidal volume plus the inspiratory reserve volume and is a measure of the maximum air that can be inspired. The air that remains in the lungs at the end of expiration of the tidal volume is the functional residual capacity and equals the expiratory reserve volume plus the residual volume.9
Minute ventilation measures the total volume of gas that passes through the lungs in a minute. It equals the respiratory rate (RR) times the volume per breath (Tidal Volume, or TV). Normally, the volume per breath is the tidal volume. Therefore, the standard formula for minute volume is RR X TV9 (Figure 20-14). However, when other lung volume subsets are used (e.g., inspiratory and expiratory reserve volumes) or the patient is breathing breaths that are smaller than tidal volume breaths, the volume per breath will change and thus change the minute ventilation. Calculating minute ventilation becomes important when determining the rate and volume at which a patient should be ventilated.
Minute alveolar ventilation takes into account anatomic dead space (Figure 20-14). It is calculated by subtracting the dead space from the volume per breath and multiplying the result times the respiratory rate ([Breath Volume - Dead Space] X RR). This calculation becomes important as various devices such as endotracheal tubes, face masks, end-tidal carbon dioxide detectors, or ventilator circuits are added. These devices all increase the dead space.
Figure 20-13 Lung volumes.
Figure 20-14 Minute ventilation and minute alveolar ventilation.
Figure 20-15 Paramedic measuring peak flow in a patient.
While the capacities of the lungs and dead spaces are important, equally important is the flow of gasses through the structures. One of the most important flows is the peak expiratory flow, or maximum velocity of gas movement during exhalation (Figure 20-15 and Skill 20-1). Many diseases restrict the flow of gasses during exhalation. Peak flow measurement can be used in the prehospital environment in to assess an asthmatic patient’s response to treatment.