Central Sleep Apnea
Pathophysiology
The instability of breathing that occurs with central apnea or hypopnea reflects brain stem interplay between the sensitivity to CO2 and the hypocapnic-apneic threshold. The inhibitory effects of sleep on ventilatory responsiveness are offset by neural mechanisms that stabilize ventilation. One such mechanism is short-term potentiation (STP), or a transient increase in ventilation occurring after a large breath (a sigh) or an apnea. STP may be abolished by prolonged hypoxia, which may explain the development of periodic breathing in patients at high altitudes or in patients with cardiopulmonary disease who have modest hypoxemia. Finally, upper airway obstruction may reflexly inhibit central neural ven-tilatory output and provoke central apnea in some patients.
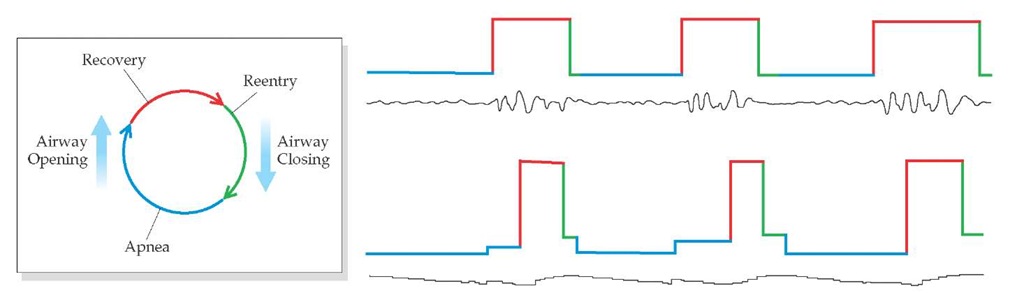
The occurrence of a central apnea or, for that matter, any ap-nea appears to set in motion events that conspire to promote further breathing instability [see Figure 6].K First, time delays in the ventilatory control system prevent resumption of rhythmic breathing after apnea until arterial CO2 levels increase by 4 to 6 mm Hg above the set point. Second, central apnea is associated with narrowing or occlusion of the pharyngeal airway.39 Resumption of ventilation thus requires opening of a narrowed or occluded airway, which involves overcoming mucosal adhesion and gravitational forces. (This narrowing of the upper airway may explain the overlap between central and obstructive apnea, or mixed apnea, and the successful use of nasal continuous positive airway pressure [CPAP] in some patients with central sleep apnea.) Third, a combination of hypoxia, hypercapnia, and transient arousal results in ventilatory overshoot, subsequent hypocapnia, and further apnea or hypopnea.
Mathematical models and studies in humans have focused on statistical correlations between the incidence of periodic breathing and the incidence of hypoxic sensitivity.40,41 Such periodic breathing during sleep occurs more frequently in individuals with higher peripheral chemosensitivity.42,43 Alternative explanations for repetitive apneas during sleep are that (1) patients with repetitive apneas have the same oscillations as normal individuals, but excitatory stimuli contribute to a larger amplitude of these oscillations in sleep apnea,41 or (2) recurrent apneas result from an intrinsic property in the feedback control of breathing in regard to either stability or instability in ventilation over time.44
Figure 6 Apneas can be thought of as a recurrent or "reentry" arrhythmia of ventilation, characterized in this example by a relatively long apnea followed by phases of recovery and reentry. Such periodicity is evident in both airflow and oxygen saturation measurements.
Risk factors
Several factors predispose persons to sleep apnea, and some of these factors are more selective for central apnea than for obstructive events.
Central sleep apnea is also more common in stroke patients than in control subjects matched for age, weight, and BMI.45 Interestingly, there is no difference between the prevalence of sleep apnea in patients with hemispheric involvement and that in patients with brain stem involvement. Although central sleep ap-nea is associated with stroke, the natural history and consequences of central sleep apnea in stroke patients remain uncertain. Available data on the effects of sleep apnea on blood pressure and sympathetic motor output suggest that it is prudent to identify and treat sleep apnea in the poststroke period.
Patients with hypothyroidism and renal failure have an unexpectedly high prevalence of both central and obstructive sleep apnea (OSA).47,48 Similarly, patients with acromegaly have a high rate of central and obstructive apnea, which correlates with higher biochemical markers of disease activity and higher chemoresponsiveness.49-51
Diagnosis
Clinical Presentation
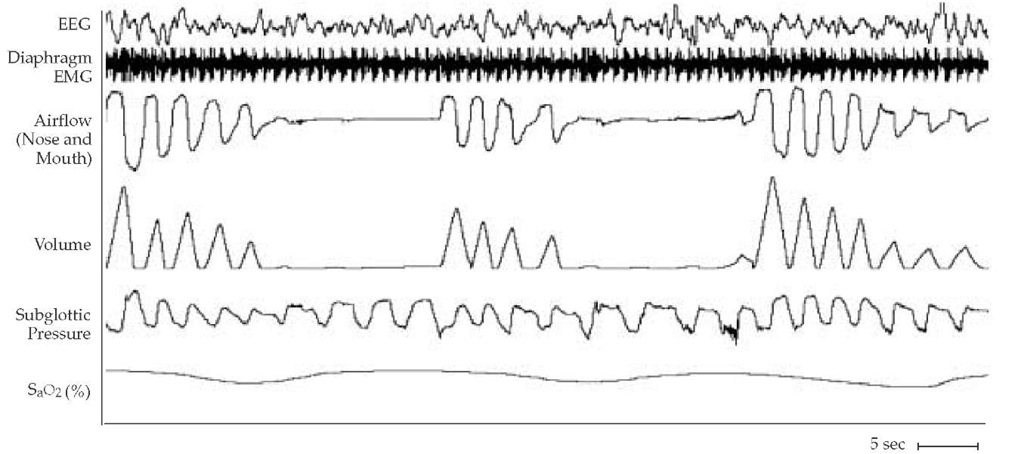
Cheyne-Stokes respiration, or CSR, is the signature feature of central apnea. CSR is marked by a crescendo-decrescendo pattern of breaths, followed by central apneas or central hypopneas, some lasting as long as 30 seconds [see Figure 7]. Patients are often hypocapnic during wakefulness and sleep. CSR commonly seen in healthy persons at high altitude results from hypoxic stimulation of breathing and resultant hypocapnia. Conditions that promote CSR at normal altitude include hypoxia, decreased lung volume, decreased metabolic rate, renal failure, and cere-brovascular disease.
CSR occurs in 25% of congestive heart failure (CHF) patients. A seemingly minor ventilatory disturbance may initiate an appropriate change in ventilation and overcompensation. Then, a change in ventilation in the opposite direction occurs, with overshoot, and an oscillating breathing pattern is established.
Diagnostic Testing
The severity of central apneas during sleep is determined by a polysomnographic study of the frequency of respiratory events per hour of sleep (i.e., the apnea-hypopnea index or respiratory disturbance index), the severity and frequency of O2 desatura-tion or hypercapnia, changes in sleep-stage distribution, and clinical symptoms produced by the disorder.
Treatment
Central apneas in otherwise healthy persons are usually not treated. Approximately 25% of patients with CHF, even those who are well compensated, have clinically significant central sleep apnea.52 CHF patients with CSR have a higher mortality and a greater need for cardiac transplantation than CHF patients without CSR events.53,54 The clinical management of CSR in the setting of CHF is well documented, and data indicate CPAP as the recommended therapy.
In a randomized study, CHF patients with CSR and central sleep apnea who received treatment with CPAP for up to 6 hours a night had a significantly greater rate of transplant-free survival than control subjects, who did not receive CPAP.55 In patients with stable chronic CHF who have CSR, CPAP has been shown to reduce CSR, left ventricular afterload, plasma catecholamine levels, and sympathetic nervous system activity and to improve left ventricular ejection fraction and quality of life.56 Application of CPAP therapy is discussed elsewhere [see Obstructive Sleep Apnea, Continuous Positive Airway Pressure, below].
Table 1 Risk Factors for Sleep Apnea with Associations to Apnea Type
|
Risk Factors |
Apnea Type |
|
Increasing age |
CSA, OSA |
|
Male gender predominance |
CSA, OSA |
|
Family history of apnea or snoring |
OSA |
|
Head form (craniofacial morphology) |
OSA |
|
Poor physical fitness |
OSA |
|
BMI |
CSA (lower BMI); OSA (higher BMI) |
|
Alcohol ingestion |
OSA |
|
Smoking exposure |
OSA |
|
Sleep restriction |
OSA |
|
Cardiovascular disease |
CSA, OSA |
BMI—body mass index
CSA—central sleep apnea and Cheyne-Stokes respiration
OSA—obstructive sleep apnea
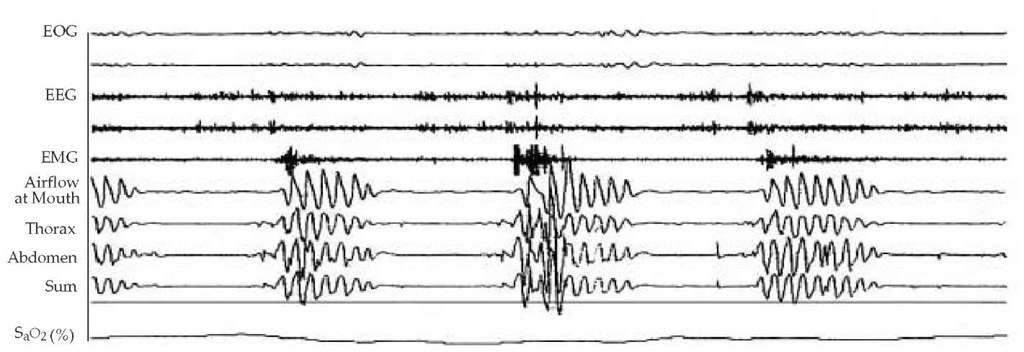
Figure 7 A fragment of a polysomnogram shows a series of central apnea episodes during slow wave sleep. Each episode of absent flow is accompanied by a cessation of thoracoabdominal efforts. Central sleep apnea has this pattern as its signature.
Supplemental O2 has also been shown to reduce the severity of CSR, decrease urinary catecholamine levels, and improve exercise capacity.57 Theophylline reduces the severity of central sleep apnea43; however, long-term use of theophylline is associated with proarrhythmic effects,58 and sustained benefits are un-proven. Thus, further study is necessary before theophylline or O2 therapy can be recommended over CPAP.
Nonhypercapnic idiopathic central sleep apnea without CSR may improve with supplemental O2 therapy or treatment with acetazolamide. Treatment for hypercapnic central sleep apnea, a disorder of the ventilatory control system, should be aimed at improving alveolar ventilation. Noninvasive ventilation or tracheostomy and mechanical ventilation should improve PaCO2, cor pulmonale, and symptoms of daytime hyper-somnolence.
Obstructive Sleep Apnea
The fundamental feature of obstructive apneas and hypo-pneas, including snoring, is a functional narrowing or collapse of the upper airway. Illness occurs in the context of repetitive events.
Pathophysiology
The presence of an anatomic abnormality is not sufficient or necessary to produce overt disease. Nevertheless, there is evidence that persons with OSA have a smaller-caliber pharyngeal airway during wakefulness than the airway in persons without OSA. In addition, the pharyngeal airway in patients with OSA syndrome has an elliptical anterior-posterior configuration, in contrast to a more circular configuration in normal persons.34 This asymmetry seems to predispose patients to anterior-posterior collapse.
A collapsing transmural pressure is generated either by a negative intraluminal pressure or a collapsing surrounding pressure; however, pharyngeal obstruction does not require negative pressure, because complete upper airway collapse occurs during central apnea.35 The occurrence of upper airway obstruction in the absence of negative intraluminal pressure is consistent with the hypothesis that the intrinsic properties of the upper airway (e.g., stiffness of the pharyngeal wall) will or will not permit collapse to occur.
Another factor in airway collapse is the mechanical interdependence of the upper airway and the thoracic cage and mediastinum. An increased lung volume is associated with increased upper airway caliber in awake humans, independent of muscle dilatation in the upper airway.59 Caudal traction may stiffen the pharyngeal airway and permit greater dilating force or, at the very least, prevent inspiratory collapse, both of which effects have been demonstrated in model systems. Therefore, a reduction in functional residual capacity could also contribute to a reduction in upper airway patency during sleep.
Proposed mechanisms for the pathophysiology of OSA involve alterations in the neuromuscular control of upper airway muscle, the resting size of the upper airway, and the degree of stiffness of the upper airway wall. The underlying defect is a pharynx that is susceptible to narrowing and collapse. The change in respiratory drive that occurs with sleep onset leads to reduced ventilatory motor output to upper airway muscles, which triggers the cascade of events leading to pharyngeal obstruction during sleep. Upper airway obstruction often occurs during experimentally induced periodic breathing at the lowest point of respiratory drive. Central ventilatory control instability is a key mechanism for repetitive obstructive apnea.60
Risk factors
Obesity is the strongest risk factor for OSA [see Table 1], and the prevalence of OSA substantially increases with age. OSA has a strong familial component that likely involves multiple genetic influences. Several anatomic abnormalities may predispose a patient to OSA; in men, a large neck size (>17 in) may be a risk factor for OSA.61 Additional risk factors include ethanol and nicotine use, because these agents promote airway collapse.
Osa-associated morbidity and mortality
The mortality associated with sleep apnea has not been satisfactorily explained. Early reports suggested mortality from car-diorespiratory failure, pulmonary embolus, and renal failure. Death has been reported to result from sedative drug use, particularly preoperative medications, which suppress breathing and the arousal response to an obstructive apnea. Automobile accidents related to excessive daytime sleepiness may have a substantial impact on morbidity and mortality. Taking a broader view, sleep quantity and quality are associated epidemiologically with hypertension, all-cause cardiovascular risk, and early mortality.
The occurrence of sleep apnea with the features of syndrome X—hypertension, obesity, diabetes, and hyperlipidemia—has prompted a call to rename this disorder syndrome Z.65 This cluster of diseases and disorders may occur through a common set of neuroendocrine factors, genetic predispositions, or both. Both the physiologic plausibility that sleep problems relate to insulin resistance66 and the epidemiologic association between snoring and cardiovascular risk factors offer a rationale to explore the pathogenesis of OSA as it relates to obesity, race, and cardiovascular disease and the pathogenesis of central apnea as it relates to aging, cardiovascular disease, and stroke. It may be that prevention of disease progression in sleep apnea may be nested within the factors that increase cardiovascular risk—namely, obesity, hypertension, lack of exercise, and alcohol use.
Diagnosis
Clinical Presentation
Self-reported snoring and excessive daytime sleepiness are the major presenting symptoms of OSA. One might suspect that the bed partner rather than the patient would report snoring more reliably; however, reports by the patient and bed partner are similar.67 Other complaints include apneas, choking during sleep, restless sleep, and, in some patients, insomnia-like symptoms along with excessive daytime sleepiness.
Diagnostic Testing and Imaging
Overnight polysomnography is the current gold standard for the diagnosis of OSA and should be considered in any patient suspected of having this disorder [see Figure 8]. Split night polysomnograms provide adequate time for both diagnosis and proper CPAP prescription. Home-based studies provide data comparable to data from laboratory studies; however, devices vary substantially. Oximetry alone cannot be recommended as a screening tool for OSA. Nasal-pressure changes detected during inspiration and expiration reflect changes in airflow with greater accuracy than thermistors.
Treatment
OSA patients should be counseled about the risk of sleepiness and offered therapy when it is clinically indicated.68
Therapy for sleep apnea is diverse and includes correction of associated medical conditions (e.g., cardiopulmonary disease) and treatment of SDB by specific interventions (e.g., surgery or use of mechanical aids). The principles of management are directed toward improvement in gas exchange, sleep continuity,15 and chronic cardiopulmonary symptoms during wakefulness. Management approaches start with consideration of mechanical devices; when mechanical devices prove inadequate, surgery to remove nasal or pharyngeal obstruction is considered.
Treatment is customized to the individual patient and may require avoidance of agents that provoke apneic episodes (e.g., alcohol, sedatives, and androgens). Obese patients with OSA who are treated for obesity may show improvement in the severity of sleep apnea, but long-term weight reduction is often difficult to achieve. Dietary management alone is effective in producing long-term weight reduction in a small minority of morbidly obese patients. However, even modest weight reduction achieved by dieting can improve SDB. Gastric stapling can achieve weight reduction in approximately 60% of patients who undergo the procedure, and appears to be effective in improving or reversing sleep apnea in most morbidly obese patients.
Continuous Positive Airway Pressure
Indication CPAP is considered the first choice of treatment for OSA.69 Treatment with CPAP improves vigilance and cognitive function in persons who report hypersomnolence; however, patients who do not have daytime hypersomnolence may not experience substantial improvement of cognitive function with CPAP.70 Treatment with CPAP will reduce blood pressure in normotensive and hypertensive patients; in the latter patients, control of blood pressure with drugs may become easier, or drugs may no longer be needed.71 Contraindications include bronchopleural fistula, acute pneumothorax, and sinus-communicating pneumocephalus. A relative contraindication is nasal or pharyngeal obstruction, which must be managed before CPAP treatment is attempted.
Figure 8 A fragment of a polysomnogram shows a series of obstructive apneas during sleep. Each episode of absent flow is accompanied by continued thoracoabdominal efforts. Apneas are terminated by arousals. Obstructive sleep apnea has this pattern as its signature.
Application Nasal CPAP is immediately effective in reversing airway obstruction in most patients with OSAS. The patient is outfitted with a nasal mask, which is attached to a blower that applies an adjustable positive pressure. The amount of pressure required to relieve upper airway obstruction (usually 5 to 20 cm H2O) is most often determined empirically during a sleep study. Effective CPAP is defined as the pressure required to prevent in-spiratory collapse of the upper airway when the patient is in the supine position and during all stages of sleep. Positive pressure applied to the nose presses the soft palate to the back of the tongue and thereby prevents leakage of air out of the mouth. If the apparatus fails, the patient is free to breathe through the oral cavity. Full-face masks or chinstraps may be needed for patients in whom air escapes through the mouth. Monitoring of pressure can be used to document the hours of use of CPAP and the effectiveness of CPAP in maintaining airway patency. Heated-hu-midification devices may increase patient compliance and reduce symptoms of nasal obstruction. For patients in whom standard CPAP is unsuccessful or intolerable, bilevel or self-adjusting modes may be attempted.
The routine use of bilevel therapy (i.e., devices that sense inspiration efforts and apply a higher positive pressure during inhalation) does not improve patient adherence; however, bilevel pressure is able to eliminate apneas with lower expiratory pressure and mean airway pressure in patients who are unable to tolerate high pressures. Devices that sense and then automatically triturate pressure to eliminate apneas operate in a way similar to personal titration; the routine use of unattended devices in the home is currently under study.
Oral Appliances
Intraoral devices to reposition the mandible are increasingly being used in the management of sleep apnea, both as primary therapy for heavy snoring and as an alternative therapy for patients who cannot tolerate CPAP.72 An oral appliance will reduce the apnea-hypopnea index and the arousal index and will improve O2 saturation even in patients with mild to moderate OSA. Oral appliances are modestly preferred over CPAP; however, CPAP is more effective than oral appliances in reducing the apnea-hypopnea index.73
Surgery
Surgical management of OSA encompasses several strate-gies74-76: (1) bypass of the anatomic obstruction by way of tra-cheostomy, (2) alteration of the bony structural support of the upper airway, and (3) alteration of the soft tissue attachments or deposits to improve airway patency. Of the surgical options, only tracheostomy is routinely effective in eliminating OSA. Central apneas may persist after tracheostomy. Despite the development of a new flap-type tracheostomy and low-profile tracheostomy tubes, local stoma problems are relatively common. Infections, local discomfort, formation of granulation tissue, and the distortions of self-image produced by tra-cheostomy have limited the use of this procedure to relatively few patients. Adaptation to a tracheostomy often takes a year or more.
Pharmacologic Therapy
Pharmacologic therapy plays a very limited role in the management of upper airway obstructions during sleep. Modafinil is the only drug approved by the Food and Drug Administration for treatment of OSA,77 and it is effective for the management of residual sleepiness after treatment with CPAP. Use of modafinil may be considered when CPAP compliance is acceptable and other behavioral issues, such as sleep restriction, have been addressed.
Medroxyprogesterone is not effective therapy for OSA in patients with normal levels of PaCO2 , but it may be used in the management of obesity hypoventilation syndrome. Acetazol-amide therapy is not effective treatment for OSA, but it will reduce the CO2-apneic threshold and thus may improve central sleep apnea. Protriptyline (a nonsedating antidepressant) increases alertness and may modestly reduce the apnea-hypopnea index, but its anticholinergic side effects limit its routine use. Nicotine may modestly reduce the apnea-hypopnea index in patients with OSA; however, current delivery methods and available doses do not have clinical utility. Serotonin agonists do not generally affect the apnea-hypopnea index or the neurocognitive defects associated with sleep apnea. Thus, these agents are not currently recommended for management of OSA, but they can be used to treat comorbid depression or mood disorder.
Other Conditions Associated with Sleep-Disordered Breathing
Asthma
Cough and cough-induced arousals from sleep may be the presenting complaint of patients with reactive airway disease. Cough may be caused by changes in airway smooth muscle tone during NREM sleep and by bronchoconstriction during REM sleep. Gastroesophageal reflux may contribute to awakenings and bronchoconstriction. Nighttime cough occurring in a patient with uncomplicated asthma may indicate inadequate therapeutic effect of asthma medication or exacerbation of airway disease by exposure to allergens [see 14:II Asthma]. Morning dipping refers to the fall in lung function that occurs in the early morning hours and represents an extreme form of diurnal variation in lung function present in most patients with airway reactivity. Reports describing morning dipping emphasize that lung function measured at midday may be normal, whereas nighttime values may show moderately severe airway obstruction.
Upper airway disease
Patients with disease of the nose, larynx, and pharynx may be disturbed during sleep by apnea or aspiration of secretions caused by excessive production of mucus (e.g., chronic allergic rhinitis) or by impaired swallowing (e.g., bilateral recurrent la-ryngeal nerve paralysis). In both instances, frequent arousals from sleep are associated with cough or a choking sensation. During sleep, particularly REM sleep, the cough response is less than it is during wakefulness. As a result, greater amounts of secretions are tolerated before a cough ensues. After awakening, this larger amount of material may precipitate paroxysmal cough. Patients who are being treated with hypnotic medications may tolerate greater amounts of secretions before cough-induced arousal from sleep, which increases the likelihood of aspiration injury to the lungs. Hypnotic medications used to manage insomnia should be used with caution in these patients.
Chronic obstructive pulmonary disease
Patients with COPD may present with a variety of sleep problems. Nocturnal cough can be related to bronchitis. Insomnia may be the consequence of therapy with methylxanthines (e.g., aminophylline). Hypoxemia during sleep may occur as a consequence of a mechanical airway impairment present during wakefulness that is exacerbated during sleep by the normal fluctuations in gas exchange. Hypoxemia that occurs only during sleep in patients with moderately severe COPD is associated with the development of cor pulmonale. In these persons, complications attributed to hypoxemia and hypercapnia are associated neither with a severe mechanical defect (forced 1-second expiratory volume of less than 1 L) nor with symptomatic apnea. Other diagnostic entities, such as recurrent pulmonary emboli or chest wall muscle weakness, should certainly be considered.
The combination of COPD and sleep apnea is called the overlap syndrome in the European literature, and it is estimated to be present in 20% to 25% of patients presenting with moderate and moderately severe COPD. There is usually historical evidence for snoring, pauses during sleep, and arousals from sleep, and the patient should be treated for OSA [see Obstructive Sleep Apnea, Treatment, above]. Patients with SDB that is not caused by OSA may experience a good sleep response to supplemental O2. Symptoms persisting after nocturnal O2 may warrant a sleep study.
Interstitial lung disease
Respiratory disturbances during sleep for patients with inter-stitital lung disease include cough and hypoxemia. Patients also may have a concomitant sleep apnea. Sleep hypoxemia may be a factor in the development of pulmonary hypertension. A restrictive defect on pulmonary function testing and interstitial fibrosis on chest roentgenogram may reflect a history of chronic aspiration. In patients with interstitial lung disease, during sleep, the tone of the gastroesophageal junction relaxes, allowing stomach contents to regurgitate to the level of the pharynx. In such patients, it may be useful to measure pH levels in the pharynx and esophagus during sleep.
Neuromuscular disorders
Respiratory disturbances caused by OSA during sleep may occur because the underlying disease process affects upper airway muscles. Sleep disturbances associated with cough, choking, or aspiration and with SDB may be the first indications of ventilatory problems in patients with neuromuscular disease. Occasionally, sleep fragmentation and the effects of sleep deprivation dominate the clinical presentation of the patient with neu-romuscular disease. After treatment for SDB, the clinical manifestations of the primary neuromuscular disorder may not appear so severe.
Kyphoscoliosis
Treatment of hypocapnic respiratory failure by tracheostomy with or without positive-pressure ventilator support during sleep can reverse cor pulmonale and improve the appearance of the chest roentgenogram.