Treatment of Nonclassic Soft Tissue Sarcomas
Rhabdomyosarcomas Children with rhabdomyosarcoma are generally treated with multiagent chemotherapy in regimens combining vincristine, actinomycin, and either cyclophos-phamide or ifosfamide.5,53-55 Doxorubicin-based regimens are generally used in adults.111 Lymph node metastases occur more commonly than in other sarcomas. Although children with metastatic disease sometimes can be cured, the prognosis in adults is poor despite excellent responses to primary aggressive chemotherapy.111 Chemotherapy is followed by resection of residual rhabdomyosarcoma and radiation therapy.
Kaposi sarcoma Lesions of the classic variant of KS generally respond to resection, radiotherapy, or low doses of vinblas-tine, doxorubicin, or interferon alfa.111 Secondary tumors, especially lymphomas, are common. Transplantation-associated KS may be controlled by modification or cessation of immunosup-pression therapy. Although HIV-associated KS responds to radiation therapy and chemotherapy, the response is less durable than in classic KS. HIV-positive patients with KS lesions involving limited areas of the skin or oral mucosa are often most easily treated with radiation. Advanced or visceral disease may be treated with cytotoxic chemotherapy using doxorubicin, vin-blastine, or paclitaxel in single-agent or combination regimens; interferon alfa is usually used as a single agent.111
Mesothelioma No therapy for mesothelioma is considered standard. Cure is elusive even with resection, radiation, and combination chemotherapy.112,113 Tumor volume shrinkage of at least 50% is achieved in 15% to 25% of selected patients treated with gemcitabine- and cisplatin-based regimens.114,115
Gastrointestinal Stromal Tumors
Treatment of GIST has changed dramatically with improved understanding of its biology. Complete en bloc surgical resection, when possible, remains the cornerstone of curative therapy. Recurrent or metastatic disease carries a poor prognosis because of GIST resistance to chemotherapy and radiotherapy.
Imatinib is an oral, relatively specific inhibitor of three tyro-sine kinase receptors: (1) the protein produced by the Philadelphia chromosome translocation of chronic myelogenous leukemia, (2) the mutated c-kit receptor in GISTs, and (3) the platelet-derived growth factor receptor.116 In a European trial evaluating doses of imatinib ranging from 300 to 1,000 mg orally daily, tumor growth was inhibited in 32 of 36 patients, and in 19 patients tumor volume decreased more than 50%.117 In a study in the United States, 36 patients with unresectable or metastatic GIST were randomized to receive either 400 or 600 mg of ima-tinib daily; of these, 19 (54%) had a partial response of at least a 50% decrease in the size of the lesion; no advantage was shown for either dose. Disease progression occurred in four patients (11%).118 In the European dose-escalation study, nausea and vomiting, edema, and dyspnea precluded administration of doses of more than 500 mg twice daily. The most common side effects (generally resolving after the first 8 weeks) were nausea and vomiting, rash, edema (particularly periorbital), and conjunctivitis (rarely with bleeding sclera). Myelosuppression was infrequent, although anemia did occur. Intratumoral and gastrointestinal bleeding developed in fewer than 5% of patients.
Sarcomas of Bone and Cartilage
Sarcomas are the second most common primary tumor of bone, after myeloma. The most common sarcomas of bone are osteosarcoma, Ewing sarcoma, and chondrosarcoma. Bone sarcomas currently represent 1% of adult malignancies and 15% of pediatric malignancies. In 2003, an estimated 4,000 persons in the United States will have developed sarcoma of bone, and 2,000 will have died of this disease.
Primary malignant lesions of bone (arising de novo) and secondary malignancies (arising from a prior benign tumor) must be distinguished from the vastly more common metastases to bone. Radiographs of a lesion can help distinguish benign from malignant lesions and often suggest the histologic origin of the tumor. Osteosarcoma characteristically produces irregular cortical surfaces, whereas Ewing sarcoma has a layered appearance like that of an onion skin.
Osteosarcoma
Osteosarcoma, defined as a primary malignancy that produces osteoid, is the most common sarcoma of bone. The incidence ratio of men to women is 1.5:1 to 2:1. The age distribution is bimodal, with the first peak in the second and third decades of life and the second in the sixth decade.6 Osteosarcoma classically arises in growth plates (i.e., around the epiphyses) of long bones during the adolescent growth spurt.
Osteosarcoma in older adults often develops in previously irradiated sites or in existing benign bone lesions, such as paget-oid bone, solitary osteochondromas, or multiple enchondro-matosis (Ollier disease). The risk of sarcoma is 0.2% in patients with Paget disease. Axial lesions are more common in adults than in children, occurring in fewer than 10% of pediatric patients but in 30% to 50% of adult patients. Extraosseous presentations are rare and occur in older adults.
Diagnosis
Clinical manifestations Patients with osteosarcoma present with severe pain of relatively short duration, often after a sports injury. Osteosarcoma may present as an obvious firm-to-hard mass covered by stretched, shiny skin, with prominent vascular markings, or may be evident only on radiograph. Mul-ticentric osteosarcomas have developed in watch-dial painters who are subject to chronic radium ingestion and occasionally in persons without risk factors, most commonly in children younger than 10 years.
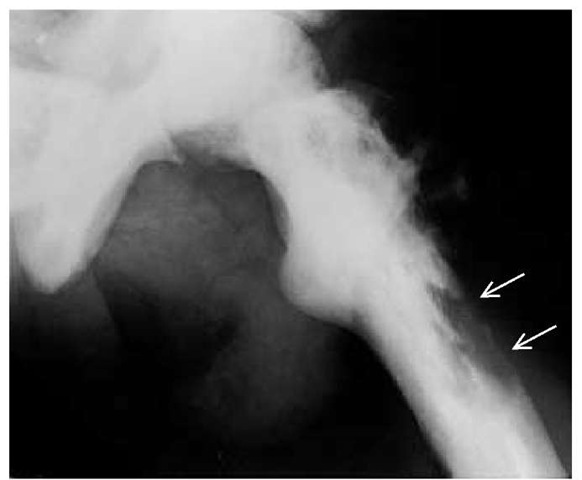
Imaging studies Radiographs and CT scans reveal osteoly-sis [see Figure 1], periosteal new bone formation, and late cortical destruction. Periosteal elevation may produce the classic Cod-man triangle on radiograph. Radiologically, the differential diagnosis includes osteochondroma and myositis ossificans.
Pathology Superficial, low-grade juxtacortical or parosteal osteosarcomas constitute only 3% to 4% of osteosarcomas, arise equally in males and females, and tend to affect adults with no prior risk factors. Low-grade osteosarcomas typically present in the third and fourth decades of life, whereas high-grade os-teosarcomas appear in the second decade. Grossly, these bulky tumors encircle the cortex of bone (generally, the distal femur and, less commonly, the proximal humerus).
Staging Evaluation
Staging evaluation includes radiographs and CT scans of the primary lesion and the lungs, which is the most likely site of metastases. Bone scans generally reveal intense uptake in the lesion and may detect additional lesions more proximal than the dominant lesion in the same bone (so-called skip lesions), metastases to other bones, or multicentric primary tumors; pulmonary uptake suggests lung metastases. Levels of alkaline phosphatase at diagnosis, which are generally elevated except in very undifferentiated lesions, correlate with prognosis, and elevated values after amputation predict residual or relapsing disease.
Patients in whom osteosarcoma is possible should be referred to an institution with an experienced sarcoma service. Expert multimodal consultation is essential before biopsy. Inci-sional biopsy should be performed by the surgeon who will do the definitive resection, because an improperly placed biopsy, particularly of proximal tibial lesions, may render limb-sparing surgery impossible and significantly compromise local control.
Figure 1 Radiography reveals osteosarcoma in a 62-year-old man with Paget disease of bone. The patient had pain associated with a soft tissue mass in the area of the greater trochanter of the left femur. Note the destruction of the cortex by the osteosarcoma in pagetic bone. The position of the original cortex is indicated by the arrows.
If the radiologic picture is virtually diagnostic, a fine-needle biopsy may be adequate to confirm the clinical diagnosis.
Treatment
Adjuvant chemotherapy On the basis of two small, randomized trials in which combination regimens were compared with observation, doxorubicin- and cisplatin-based adjuvant chemotherapy is the established treatment for osteosarcoma. The Pediatric Oncology Group and UCLA studies showed a significantly improved 2-year disease-free survival; the UCLA study also demonstrated a significantly prolonged overall sur-vival.120,121 The optimal combination of agents and schedule has not yet been established. Of six randomized trials evaluating high-dose methotrexate, one demonstrated an advantage for high-dose over standard-dose methotrexate, whereas five showed no advantage for high-dose methotrexate.122,123 In a study by the European Osteosarcoma Intergroup, short intensive chemotherapy using doxorubicin and cisplatin was compared with a complex multiagent protocol in patients with operable osteosar-coma. Progression-free survival at 5 years was 44% in both groups, and the two groups had comparable overall sur-vival.124,125 In a follow-up study, the addition of ifosfamide did not appear to improve these results.126
Preoperative chemotherapy Preoperative chemotherapy has many theoretical advantages over postoperative adjuvant chemotherapy.
Early systemic treatment may more effectively eradicate microscopic metastatic deposits. The response to preoperative chemotherapy can be evaluated histologically, and the regimen can be modified if the response is suboptimal. Patients receiving preoperative chemotherapy whose resected tumor specimen is more than 90% necrotic may have a significantly higher survival rate than patients receiving only postoperative chemother-apy.127 Patients who have less than 90% necrosis in the resected tumor after preoperative chemotherapy may have increased disease-free survival if switched to other effective agents post-operatively. Because resolution of tumor vascularity on angiog-raphy appears to correlate with histologic necrosis, monitoring angiographic findings may maximize tumor response to chemotherapy before surgery.128
Preoperative chemotherapy may facilitate limb-sparing surgery, preservation of muscle groups, and limb function. The delay in surgery also allows procurement of a correctly sized internal prosthesis for replacement of excised bone. However, patients receiving preoperative chemotherapy must be regularly evaluated and should undergo prompt resection if the tumor increases in size during chemotherapy.
Radiotherapy Osteosarcoma tends to be markedly radiore-sistant. Radiotherapy alone has not been shown to improve the rate of successful limb-sparing surgery or decrease the risk of local recurrence in tumors with close or positive surgical margins. However, in a randomized, controlled trial, higher doses of radiotherapy (given preoperatively with intra-arterial doxoru-bicin) significantly increased the rate of local complications.120
Surgical treatment Either amputation or limb-sparing surgery may be appropriate as long as lesions are widely excised with several centimeters of pathologically documented unin-volved margins. Lesions with a significant soft tissue component or neurovascular involvement generally necessitate amputation. Osteosarcomas arising in sites of prior Paget disease or irradiation tend to be vascular and centrally located and thus are difficult to resect for cure.
Although functional results after limb-sparing procedures are excellent in 60% to 75% of patients, relapse or complications from treatment may later necessitate amputation. In appropriately selected patients, local control rates (i.e., 90% to 97%) and survival rates for limb-sparing procedures are similar to those for amputation.120,128 Limb-sparing resection tends to be more successful for upper-extremity lesions than for lower-extremity lesions because upper-extremity lesions are associated with fewer complications from weight bearing and dependent edema. In children, an internal prosthesis whose length can be adjusted as the child grows can reduce limb-length disparity. Fractures remain an important complication in active individuals, and thus, amputations are actually preferable for individuals who wish to pursue contact sports.120
Treatment of metastatic disease Relapses tend to occur in the first 2 years after completion of primary therapy. Major prognostic variables include grade and invasion through the bone cortex to involve soft tissue. Metastases most frequently develop in lung and, less commonly, in bone. Patients who have already received adjuvant chemotherapy may respond to the same drugs if metastases develop more than 6 months after the last adjuvant treatment. Between 20% and 40% of selected patients with five or fewer pulmonary lesions and a disease-free interval of more than 12 months can be cured with combination chemotherapy and surgical resection.
Chondrosarcoma
Chondrosarcoma, which represents about 20% of bone sarcomas, is the most common bone sarcoma after osteosarcoma. Ex-traosseous chondrosarcomas arising in soft tissue are rare.129 Primary chondrosarcomas occur in previously normal bone; secondary chondrosarcomas arise in prior benign lesions, generally enchondromas.130 Chondrosarcomas in patients with multiple enchondromatosis (Ollier disease) are generally low grade, whereas chondrosarcomas associated with soft tissue heman-giomas (Maffucci disease) are frequently high grade. Chon-drosarcoma represents about 10% of radiation-associated sarcomas and may arise in pagetoid bone.
The incidence of chondrosarcomas increases steadily with age.6 The most common sites of involvement are the pelvis (31%), femur (21%), shoulder (13%), face (9%), and ribs (9%).6 Lesions can be painless but tend to be painful if they grow rapidly.
Diagnosis
On radiograph, central chondrosarcomas appear as popcorn-shaped calcifications. Peripheral chondrosarcomas may appear as long, slightly calcified spicules radiating from the cortex to a flattened outer surface; there may be little cortical or medullary involvement and a faint Codman triangle caused by a disruption of the smooth periosteal surface. Bone scans generally demonstrate intense uptake in the lesion.
Chondrosarcomas are defined as malignant stromal tumors of bone that produce cartilage but no osteoid. Histologically, the tumors have the appearance of cartilage with malignant chon-drocytes. Low histologic grade is less reliable than patient age, site of origin, lesion size, and radiographic appearance in determining biologic behavior.
Mesenchymal chondrosarcoma is a histologic variant that tends to arise in the ribs, mandible, maxilla, skull, and ex-traosseous sites; it is characterized by a small round cell histo-logic component and has some sensitivity to chemotherapy.
Treatment
Chondrosarcomas, which are relatively resistant to both radiotherapy and chemotherapy, must be adequately resected at the time of initial diagnosis. Aggressive resection is particularly appropriate for eminently curable low-grade chondrosarcomas. Local recurrences tend to increase with histologic aggressiveness.
Ewing sarcoma
Ewing sarcoma constitutes 10% to 14% of primary malignant bone tumors in whites but is rare in other races.8 The peak incidence occurs between 10 and 25 years of age (range, 2 to 65 years), and the risk in men is twice that in women [see Table 1].6 Ewing sarcoma and osteosarcoma occur in the same sex and age groups, but they can usually be distinguished radiograph-ically and histologically.5
Diagnosis
Patients with Ewing sarcoma present with fever, weight loss, malaise, poorly localized bone pain, and a rapidly enlarging mass. Leukocytosis, fever, and an elevated erythrocyte sedimentation rate mimic osteomyelitis. The most common sites of involvement are femur (27%), pelvis (18%), and tibia and fibula (17%).6 Diagnosis of pelvic Ewing sarcoma is frequently delayed because pain is poorly localized and the mass is not clinically apparent.
Histologically, Ewing sarcoma on reticulin stain appears as clusters of small blue cells bordered by fibrous septa (in contrast to lymphoma cells, which have no septa).83 Cytogenetics generally reveal the t(11;22) translocation, which is identical to that found in PNETs, suggesting a possible neurogenic origin of Ew-ing sarcoma.19
Radiographically, Ewing sarcoma forms a fusiform enlargement of the long bones, with onion-skin layering of the periosteum and central mottling (so-called cracked-ice appearance). A pulmonary CT scan, bone scan, and marrow aspirate and biopsy are necessary for staging.
Clinically detectable metastases are present in about one third of patients at diagnosis. The most frequent sites of metastasis are the lung, bone, and marrow. Vertebral metastases commonly lead to spinal cord compression. Ewing sarcoma results in 90% mortality in patients who undergo surgical resection alone, which suggests that systemic disease may be present in a substantially higher percentage of patients than those who have detectable metastases at presentation.
Treatment
Initial treatment consists of a multiagent chemotherapy regimen of doxorubicin, vincristine, and cyclophosphamide, alternating with etoposide and ifosfamide administered before and during radiotherapy to the involved bone.111,131 Radiotherapy concentrating on the primary lesion, if begun during the fourth or fifth cycle of chemotherapy, controls local disease in 70% of patients and provides good functional results. Because of a high risk of local failure and secondary radiation-associated osteosar-comas, expendable bones (e.g., rib, tibia) are often resected, particularly if biopsy after radiotherapy and chemotherapy reveals residual viable tumor.
Survival rates correlate inversely with age (i.e., 70% for patients younger than 10 years and 46% for those older than 16 years).132 Lower survival rates are associated with primary lesions of the pelvis, humerus, and rib; high levels of lactate dehy-drogenase; and extensive soft tissue involvement. One third of pediatric patients with metastases are cured by current therapy, but few adults with metastases survive.
Other bone sarcomas
Fibrosarcoma, chordoma, angiosarcomas, and MFHs of bone are usually treated with resection. Radiation to the site of the lesion and adjuvant chemotherapy with doxorubicin and either cisplatin or ifosfamide may also be used.