Psoriasis is an immune-mediated inflammatory cutaneous disorder characterized by chronic, scaling, erythematous patches and plaques of skin. It can begin at any age and can vary in severity. Psoriasis can manifest itself in several different forms, including pustular and erythrodermic forms. In addition to involving the skin, psoriasis frequently involves the nails, and some patients may experience inflammation of the joints (pso-riatic arthritis). Because of its highly visible nature, psoriasis can compromise both the personal and the working lives of its victims.
Breakthroughs in the treatment of psoriasis have led to a better understanding of its pathogenesis. This topic reviews current knowledge of the genetics, pathogenesis, and treatment of psoriasis.
Epidemiology
The estimated prevalence of psoriasis ranges from 0.5% to 4.6% worldwide. The reasons for the geographic variation in prevalence are unknown, but climate and genetics may play a role. Psoriasis is uncommon in blacks in tropical zones, but it is more often seen in blacks in temperate zones. It occurs commonly in Japanese persons but rarely in persons native to North and South America. In the United States, studies have variously reported that 4.5 million adults1 or 7 million adults and children2 have psoriasis.
Psoriasis can occur at any age, with some cases being reported at birth and others being reported in patients older than 100 years. In Farber and Nall’s pioneer study of 5,600 patients, the average age of onset of psoriasis was 27.8 years; in 35% of patients, onset occurred before 20 years of age, and in 10%, onset occurred before 10 years of age.3Psoriasis occurs with equal frequency in men and women, but in Farber and Nall’s study, onset occurred later in men. In populations in which there is a high prevalence of psoriasis, onset tends to occur at an earlier age. In the Faroe Islands, for example, the prevalence is 3%, and the average age of onset is 12.5 years. The average age of onset is 23 years in the United States. In persons with earlier age of onset, psoriasis is more likely to be severe, with involvement of a large area of skin surface.
Pathogenesis
Psoriasis was once thought to be caused by an abnormality in epidermal cell kinetics; it is now thought that an abnormality in the immune system triggers epidermal proliferation. The role of activated lymphocytes in the development of psoriasis was first proved through investigations of DAB389 interleukin-2 (IL-2), a fusion protein consisting of molecules of IL-2 fused to diphtheria toxin. This fusion protein binds to high-affinity IL-2 receptors on activated T cells, destroying those cells. In a study of DAB389 IL-2 treatment in 10 patients, four patients showed dramatic clinical improvement and four others showed moderate improve-ment.4 Unfortunately, the side effects of DAB389 IL-2 have precluded its approval for the treatment of psoriasis.5
The skin of patients with lesional psoriasis has higher numbers of antigen-presenting cells that can activate T cells. For T cell activation to occur, antigen-presenting cells must deliver at least two signals to resting T cells. The first signal occurs when major histocompatibility complex (MHC) class II molecules of the antigen-presenting cells present antigens to the T cells. A second co-stimulatory signal must be delivered through the interaction of ligands on the surface of the antigen-presenting cells with receptors on the surface of T cells. Examples of this process include the interaction of B7 molecules with CD28 on the surface of resting T cells and the interaction of lymphocyte function-associated antigen 3 (LFA-3) with CD2 or intercellular adhesion molecule-1 (ICAM-1) with LFA-1 on the surface of T cells.67 Blockade of any of these steps results in clearing of psoriasis.8,9 Upon activation, T cells release Th1 (T helper type 1) cytokines, IL-2, and interferon gamma, which together induce proliferation of keratinocytes and further stimulation of T cells. Inflammatory cytokines such as tumor necrosis factor-a (TNF-a) are found in psoriatic skin lesions and joints, and treatment with TNF-a blockers results in clearing of psoriasis and of psoriatic arthritis.10
Etiology
Genetic factors
Several lines of evidence suggest that psoriasis has a genetic etiology. One third of persons affected have a positive family history. Studies have found a higher concordance rate in monozygotic twins than in dizygotic twins or siblings (70% versus 23%).
Current evidence suggests genetic heterogeneity. Both auto-somal dominant inheritance with incomplete penetrance and polygenic or multifactorial inheritance have been described. The most important psoriasis susceptibility gene appears to be PSORS1, which has been mapped to the region on chromosome 6p21 that codes for the MHC; seven other PSORS genes have been found on other chromosomes.12 Psoriasis is also associated with a single-nucleotide polymorphism on chromosome 17q25 that impairs binding of a runt-related protein (RUNX1).13
Contributing factors
The course and severity of psoriasis can be affected by a number of endogenous and exogenous factors, including stress, climate, concurrent infections, and medications.
Psychological Stress
Many patients believe that anxiety or psychological stress has an adverse effect on the course of their psoriasis. The etiologic significance of stress in psoriasis is difficult to evaluate, however, because of the subjective nature of the evidence used in many of the investigations into this question.14 In a prospective study, a multivariate statistical method revealed a positive correlation between severity of psoriasis symptoms and psychological stress related to adverse life events.15 Psoriasis itself can be a source of stress: the effects of psoriasis on physical and mental function have been compared with the effects of cancer, heart disease, diabetes, and depression.16
Climate
It has long been known that psoriasis improves when patients are exposed to sunny climates and to regions of lower latitude. In northern latitudes, exacerbation of psoriasis commonly occurs during the fall and winter.
Infection
Viral or bacterial infections, especially streptococcal pharyngitis or tonsillitis, may precipitate the onset or exacerbation of pso-riasis.17 Guttate psoriasis, in particular, is often attributed to a previous streptococcal infection. Attempts to reverse psoriasis by treatment with oral antibiotics have not proved effective in double-blind trials.18 Nevertheless, some investigators advocate antibiotic therapy for psoriasis.19
Infection with HIV has also been associated with psoriasis. In some patients with HIV infection, preexisting psoriasis becomes exacerbated; in other patients, psoriasis develops within a few years after HIV infection. Often, HIV-infected patients present with symptoms similar to those of Reiter syndrome.20
Drugs
Numerous drugs can worsen psoriasis.Antimalarial agents such as chloroquine can cause exfoliative erythroderma or pustular psoriasis. Up to 31% of patients experience new onset or worsening of psoriasis as a result of antimalarial therapy. Lithium and beta blockers such as propranolol may precipitate the onset of psoriasis or cause exacerbations of psoriasis.22 Some nonsteroidal anti-inflammatory drugs (NSAIDs) also exacerbate psoriasis, although this effect is sufficiently minor to allow NSAIDs to be used in the treatment of psoriatic arthritis.23 Flares of pustular psoriasis may be precipitated by withdrawal from systemic corticosteroids or withdrawal from high-potency topical corticosteroids. Interferon therapy has been associated with development or exacerbation of psoriasis, presumably because of the Th1 effects of this therapy.24
Other Factors
Trauma to the clinically uninvolved skin of patients with psoriasis can cause a lesion to appear at the exact site of injury; this phenomenon is known as the Kobner response. Cuts, abrasions, injections, burns resulting from phototherapy, and other forms of trauma can elicit this reaction.
Smoking may be an exacerbating factor in psoriasis.25 Alcohol use has also been implicated in the exacerbation of psoriasis.
Surveys have suggested that diet plays a role in the development of psoriasis, and attempts have been made to affect the clinical course of psoriasis through modification of diet.27 Double-blind studies, however, have failed to show that diet has either a beneficial or a detrimental effect on the severity of psoriasis.
Diagnosis
The diagnosis of psoriasis is usually made on clinical grounds. If unusual features are present, biopsy of affected skin can be done to confirm the diagnosis.
Clinical variants
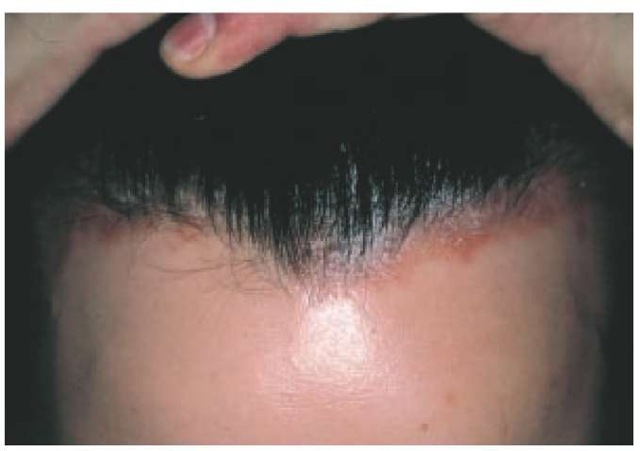
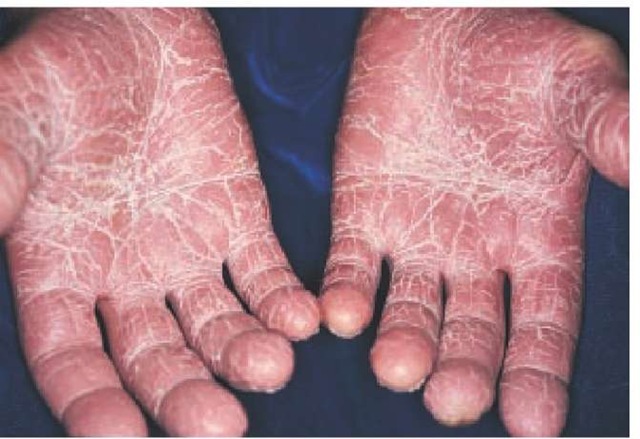
Nearly 90% of patients with psoriasis have plaque type, a form that is characterized by sharply demarcated, erythematous, scaling plaques. The elbows [see Figure 1], knees, and scalp [see Figure 2] are the most commonly affected sites. The intergluteal cleft [see Figure 3], palms [see Figure 4], soles [see Figure 5], and genitals are also commonly affected, but psoriasis can involve any part of the body. Lesions frequently occur in a symmetrical pattern of distribution.
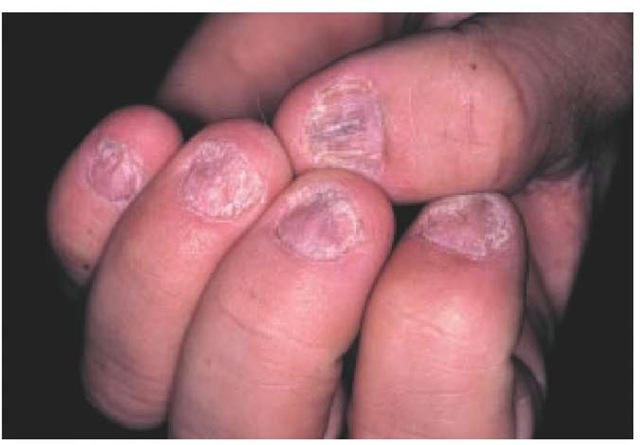
Many patients have only one or a few lesions that persist for years and that occasionally resolve after exposure to sunlight. Other patients can be covered with plaques that become confluent, affecting nearly 100% of the body surface area. Nail involvement is common, particularly in patients with severe disease.
The second most common form of psoriasis, guttate psoriasis, affects fewer than 10% of patients and is characterized by the development of small, scaling, erythematous papules on the trunk and the extremities [see Figure 6]. This form of psoriasis often follows streptococcal infection. Patients with plaque-type psoriasis can develop guttate psoriasis. Conversely, patients with guttate psoriasis frequently develop plaque-type psoriasis. Occasionally, guttate lesions enlarge and become confluent, resulting in the formation of plaques.
Figure 1 Involvement of the elbows is characteristic of plaque psoriasis.
Figure 2 The scalp is affected in the majority of patients with plaque psoriasis.
Figure 3 The intergluteal cleft is a common site of involvement in patients with plaque psoriasis.
Figure 4 Psoriasis of the palms is shown in this patient.
Figure 5 Sharply demarcated, erythematous, scaling plaques on the feet are apparent in this patient with psoriasis of the soles.
Erythrodermic psoriasis is a severe form of psoriasis that often affects the entire cutaneous surface. Patients present with an ex-foliative erythroderma in which the skin is very red and inflamed and is constantly scaling [see Figure 7]. Patients are acutely ill, their skin having lost all protective function. Loss of temperature control, loss of fluids and nutrients through the impaired skin, and susceptibility to infection make this a potentially life-threatening condition.
Erythrodermic psoriasis can develop de novo or evolve from typical plaque-type or guttate psoriasis. Erythrodermic psoriasis can occur after withdrawal of systemic corticosteroids, after phototherapy burns, as a result of antimalarial treatment, as a result of a drug-induced hypersensitivity reaction, or for no apparent reason. Cutaneous T cell lymphoma may also present as erythroderma and needs to be differentiated from erythroder-mic psoriasis.
Pustular psoriasis, another severe form of the disease, can occur in patients with preexisting psoriasis or can arise de novo. Pustular psoriasis can be generalized (von Zumbusch type) or localized to the palms and soles [see Figure #]. In either case, the condition is severe and debilitating. In generalized pustular psoriasis, the body is covered with sterile pustules.
Figure 6 Guttate psoriasis is characterized by small scaly papules and plaques.
Figure 7 Erythrodermic psoriasis is characterized by generalized erythema and desquamation.
Figure 8 Pustular psoriasis can be localized to the palms and soles or generalized.
Figure 9 Involvement of the nails is common in psoriasis.
As with erythrodermic psoriasis, the protective functions of the skin are lost, and patients may succumb to infection or hypo-volemia and electrolyte imbalance caused by loss of fluid through the skin. Although fever and leukocytosis are common features in pustular psoriasis, the possibility of infection should not be overlooked; patients with pustular psoriasis have died of staphylococcal sepsis.28
As with erythrodermic psoriasis, pustular psoriasis is most commonly precipitated by withdrawal of systemic cortico-steroids. However, it can also result from therapy with anti-malarial drugs or lithium, and it can develop spontaneously.